Abstract
Objectives
The goal of the present study was to investigate the hypothesized complex interactions between dimensions of self-compassion and obsessive-compulsive symptoms (OCD) in a non-clinical sample.
Method
Four hundred and twenty-four individuals (273 women) ranging in age from 18 to 83 years (M = 41.00; SD = 14.50) participated in the cross-sectional survey. The participants completed the Self-Compassion Scale (SCS) and the Obsessive-Compulsive Inventory—Revised (OCI-R).
Results
Certain dimensions of self-compassion were found to be associated with specific OCD symptoms, with positive dimensions (except Common humanity) correlating with reduced Obsessing, Hoarding, and Ordering, and negative dimensions correlating with all OCD symptoms. Canonical correlation analysis indicated three significant linkages: (1) between Isolation, Over-identification, and Obsessing, (2) between Self-judgment, Over-identification, Ordering, and Checking, and (3) between Self-judgment and Neutralizing. Exploratory graph analysis challenged the structure of the SCS and the OCI-R, suggesting two dimensions of self-compassion, compassionate self-reference and uncompassionate self-reference; and two dimensions of OCD, obsessing and other OCD symptoms. The Obsessing subscale appeared as a bridge between uncompassionate self-reference and OCD symptoms. Compassionate self-reference was negatively correlated with uncompassionate self-reference and obsessing, whereas uncompassionate self-reference was positively correlated with obsessing and OCD symptoms.
Conclusions
Investigation of the associations between self-compassion and psychopathology should avoid aggregating the uncompassionate and compassionate dimensions of self-compassion. The significant associations in the network of self-compassion and OCD symptoms were between uncompassionate self-reference, obsessing, and OCD symptoms.
Preregistration
This study is not pre-registered.
Similar content being viewed by others
Self-compassion has recently been demonstrated as a protective factor for various dimensions of well-being (Phillips & Hine, 2021; Zessin et al., 2015), while lack of self-compassion was regarded as a risk factor for distress and psychopathology (Marsh et al., 2018). These results underpin therapeutic approaches based on self-compassion and focused on focus on reducing self-criticism, over-identification, and isolation and on developing self-kindness, communal approach, and mindfulness (e.g. Wakelin et al., 2022), which were found to be relatively efficient in reducing psychopathological symptoms (Wilson et al., 2019). The highest reductions in symptoms due to self-compassion-based therapy were observed for eating behaviors and rumination, while moderate effects were observed for stress, depression, self-criticism, and anxiety outcomes (Ferrari et al., 2019). In addition, these promising results could enhance attempts at using self-compassion-based interventions in other categories of psychopathology as well.
Despite the fact that symptoms of lacking self-compassionate reference (e.g., self-criticism and refusing negative, intrusive thoughts) are very common in obsessive–compulsive symptomatology (OCD; Abramowitz et al., 2003), associations between self-compassion and obsessive–compulsive (OCD) symptomatology remain understudied. Initial results in this area showed negative associations between overall scores of self-compassion and OCD (Eichholz et al., 2020; Leeuwerik et al., 2020). Given significant impairments caused by OCD, including a high risk of suicidal thoughts and behaviors (Benatti et al., 2021)—primarily due to high comorbidity of OCD with depression (Angelakis et al., 2015)—and severe reductions in quality of life (Skapinakis et al., 2019), the possibility of using self-compassion-related intervention in this particular psychopathology could be helpful for clinical practice (e.g., Quinlan, 2021).
Self-compassion was originally based on Buddhist philosophy. Thanks to Kristin Neff (2003a), this concept became a permanent fixture in psychology and psychiatry. Self-compassion can be defined as understanding or kindness towards oneself, connected with the ability to understand one’s own suffering, one’s limitations, failures, and negative emotions (Neff, 2003a, 2003b). Self-compassion is also described as being open to and sensitive toward one’s own suffering, accompanied by a feeling of caring and kindness towards oneself by adopting understanding and a non-judgmental attitude about one’s own imperfections (Neff, 2003a). A fundamental aspect of self-compassion is awareness of the fact that all people are imperfect and make mistakes, all people sometimes fail and experience life problems. Self-compassion is structured by three components, or, more specifically, six, as each positive element has its negative counterpart. The first element is self-kindness, whose negative side is self-judgment. The second element is common humanity, whose negative counterpart is isolation. The third element is mindfulness, whose negative counterpart is over-identification. The Self-Compassion Scale (SCS; Neff, 2003a), developed to measure six dimensions of self-compassion, is one of the most frequently used measures in the field (Muris & Otgaar, 2022).
Previous meta-analytical and review studies have shown that self-compassion is significantly correlated with mental health. MacBeth and Gumley (2012) showed a large effect size for the negative relationship between self-compassion and depression, anxiety, and stress. In the later meta-analysis, a broader range of psychopathology was examined (e.g., bipolar disorder, paranoid ideation, eating problems, body preoccupation, anxiety, depression, stress). Experimental studies have shown that self-compassion-related interventions result in substantial reductions in self-criticism (Wakelin et al., 2022) and lower eating pathology (Turk & Waller, 2020). Self-compassion was negatively related to suicidal thoughts and behaviors and non-suicidal self-injuries (Suh & Jeong, 2021). These associations might be due to the fact that in general, individuals high in self-compassion use more adaptive coping strategies and fewer maladaptive coping strategies (Ewert et al., 2021), as well as fewer repetitive negative thoughts (Wadsworth et al., 2018).
Previous studies have exposed a differential role taken on by self-compassion components for psychopathological symptoms. In their psychometric study of the internal structure and validity of the SCS, Muris and Petrocchi (2017) demonstrated that negative aspects of self-compassion (self-judgment, isolation, and over-identification) had a stronger negative impact on psychopathology compared to positive aspects of self-compassion (self-kindness, common humanity, and mindfulness). Depression and vulnerable personality styles (self-criticism etc.) were lower among individuals high in self-kindness and mindfulness as dimensions of self-compassion (Wong & Mak, 2013). In research conducted by Phillips (2021), latent profile analysis of the six self-compassion dimensions variables identified three self-compassion mindsets: uncompassionate, moderately self-compassionate, and highly self-compassionate self-responding. Uncompassionate individuals reported the highest indices of depression and stress compared to moderately and highly self-compassionate individuals. Highly self-compassionate individuals additionally reported lower anxiety compared to uncompassionate and moderately self-compassionate people (Phillips, 2021). According to these findings, dimensions of self-compassion had different patterns of associations with psychopathological symptoms, while the particular profile of self-compassionate responding also had different relationships with psychological distress, anxiety, and depression.
These results, however, should be interpreted in the context of the ongoing debate regarding the internal structure of self-compassion. Recent methodological and empirical studies questioned the internal structure of the SCS, which is frequently used to assess self-compassion (Muris & Petrocchi, 2017). The criticism consists in suggestions that the sub-dimensions of isolation, over-identification, and self-judgements should be regarded not as constituting a part of a compassionate reference to oneself but rather as being closer to psychopathological symptoms (Muris et al., 2018; Muris & Petrocchi, 2017; Muris et al., 2019). Aggregating the positive and negative sub-scales of self-compassion into one global score, therefore, could lead to ambiguous results concerning the associations between self-compassion and psychopathology (Muris & Otgaar, 2022). There is a need for studies which would examine the boundaries and associations between various dimensions of symptoms of psychopathology and manifestations of compassionate and uncompassionate self-reference.
OCD remains an understudied area of research in terms of the associations between self-compassion and psychopathology (Muris & Petrocchi, 2017). OCD has two main characteristics: (a) unwanted, recurring, and bizarre thoughts, impulses, or doubts that lead to distress (obsessions); and (b) repetitive rituals (behavioral or mental) performed in order to reduce this distress and also referred to as compulsions (Abramowitz, 2006). OCD has several common presentations which include obsessions regarding contamination, responsibility for harm caused by a catastrophe, aggressive intentions, unwanted sexual behaviors, and blasphemous thoughts or behaviors (Abramowitz et al., 2003). Obsessive–compulsive symptoms are frequently grouped into six categories: washing (excessive cleaning and washing in reaction to obsessions about contamination), obsessing (difficulties in controlling intrusive thoughts), neutralizing (using ritualistic behaviors in order to neutralize fears resulting from obsessions), ordering (keeping order, symmetry, avoiding disarrangement of things), checking (repetitive reassuring oneself that doors, windows, gas are closed, etc.), and hoarding, that is, difficulty getting rid of unnecessary things (Foa et al., 2002). Although OCD presentations are heterogeneous, their central mechanisms are common and include a cycle of dysfunctional beliefs that produce distress and compulsive behaviors that are intended to lower the distress resulting from dysfunctional beliefs (Abramowitz et al., 2009).
The most effective intervention for OCD or OCD patients with symptoms below the clinical threshold is cognitive-behavioral therapy (Olatunji et al., 2013). However, a considerable number of patients drop out of the therapy prematurely due to the difficulty of dealing with distressing emotions associated with modification of dysfunctional beliefs (Eichholz et al., 2020). These dysfunctional beliefs include an inflated sense of responsibility, over-importance of thoughts, the need to control thoughts, perfectionism, overestimation of threats, and intolerance of uncertainty (OCCWG, 1997). Previous studies have shown that higher mindfulness or self-compassion are associated with lowering similar dysfunctional beliefs, manifesting in perfectionism (Keng et al., 2016), for example, and with developing higher distress tolerance (Basharpoor et al., 2021). Moreover, self-compassion was associated with lowered levels of automatic negative thoughts (Arimitsu & Hofmann, 2015) and of anxiety (Marshall & Brockman, 2016) and rumination (Smeets et al., 2014) which frequently accompany OCD symptoms (Wahl et al., 2019). These results suggest that mindfulness or self-compassion-based interventions could be particularly helpful for patients suffering from obsession and compulsions as an additional strategy during cognitive-behavioral therapy.
Initial studies of associations between OCD symptoms and self-compassion showed that individuals with obsessive–compulsive disorder reported less mindfulness and self-compassion compared to anxious/depressive patients and healthy controls (Leeuwerik et al., 2020). There was a negative association between self-compassion and obsessive–compulsive symptomatology (Wetterneck et al., 2013). Despite the high comorbidity between OCD and depression (Fineberg et al., 2013), self-compassion explained OCD over and beyond depression (Leeuwerik et al., 2020). Initial experimental research has already shown the effectiveness of compassion-focused therapy for OCD (CFT-OCD) in the reduction of OCD symptoms and improvements as far as fear of guilt, self-criticism, and self-reassurance are concerned (Petrocchi et al., 2021). Another possible mechanism responsible for associations between self-compassion and OCD is emotion dysregulation (Eichholz et al., 2020). Firstly, self-compassion is associated with adaptive emotion dysregulation (Neff, 2003a). Secondly, research by Chase et al. (2019), conducted on attendees who reported a diagnosis of OCD, showed that self-compassion and emotion regulation difficulties were associated with overall OCD severity. Moreover, emotion regulation difficulties mediated relationships between self-compassion and overall OCD severity, as well as the severity of two OCD symptom dimensions: responsibility for harm and unacceptable thoughts (Chase et al., 2019). Although previous research has exposed important characteristics and mechanisms of the OCD and self-compassion association, most of it measures these constructs only unidimensionally (e.g. Leeuwerik et al., 2020; Wetterneck et al., 2013). This unidimensional approach may be questionable due to the ambiguity of the internal structure of self-compassion.
Due to the multifaceted nature of both self-compassion (Neff, 2003a) and OCD (Foa et al., 2002), associations between self-compassion and OCD are likely complex. Self-compassion correlated negatively with responsibility and unacceptable thoughts sub-scales of the Dimensional Obsessive–Compulsive Scale but did not correlate with the contamination and symmetry sub-scales (Chase et al., 2019). Similarly, the observing, non-judging, and non-reacting sub-scales of mindfulness measures correlated negatively with overall scores of OCD, while the other sub-scales were not associated with OCD symptoms (Leeuwerik et al., 2020). There is a scarcity of studies investigating the complex associations between various sub-dimensions of self-compassion and OCD presentations. Moreover, focusing on the dimensions of the constructs may result in underestimation of symptom-level associations and shared variance between manifestations of constructs on a lower level (e.g., symptom-to-symptom associations between dimensions of psychopathological syndrome; Christensen et al., 2019a, 2019b) and a higher level (construct-to-construct associations, e.g., the association between psychopathological syndromes; Blanken et al., 2018). Thus, analytic techniques investigating dynamic mutual associations between the measured manifestations of the studied constructs could add new insights to the findings from studies focused on the associations between the dimensions of the studied constructs.
The goal of the present study was to investigate the complex associations between dimensions of self-compassion according to Neff’s model (Neff, 2003a): self-kindness, mindfulness, common humanity, over-identification, isolation and self-judgment, and OCD symptomatology, including washing, obsessing, neutralizing, ordering, checking, and hoarding (Foa et al., 2002). Based on previous findings (Eichholz et al., 2020; Leeuwerik et al., 2020), we expected negative associations between positive aspects of self-compassion (self-kindness, common humanity, and mindfulness) and OCD symptoms (Hypothesis 1), and positive associations between OCD symptoms and self-judgment, isolation, and over-identification (Hypothesis 2).
We used two multivariate techniques of examination of complex associations between sets of variables: canonical correlation analysis (CCA; Sherry & Henson, 2005) and network analysis (Borsboom & Cramer, 2013). CCA is a method used for the discovery and quantification of associations between two sets of variables (Härdle & Simar, 2012; Thompson, 1991). Since both self-compassion and OCD are multidimensional, CCA can help detect canonical functions which represent projections of both sets of variables in an interpretable way (Härdle & Simar, 2012).
Network analysis treats psychiatric syndromes or personality traits as dynamic structures of the associations between symptoms and variables (referred to as “nodes”; Borsboom & Cramer, 2013). Network analysis, thus, makes it possible to discover the symptoms which are most influential and could be responsible for the activation of other symptoms (Borsboom, 2017; Epskamp et al., 2018). It could also help in understanding which symptoms group into communities and which processes bridge between communities of symptoms (Robinaugh et al., 2016). This property of network analysis could be particularly useful for addressing the ongoing debate regarding the internal structure of compassionate and uncompassionate self-reference (Muris & Petrocchi, 2017; Neff, 2020) by showing how manifestations of positive and negative aspects of self-compassion are related to OCD symptoms in a common network. Exploratory graph analysis (EGA) is a recently developed network analysis method designed particularly for the detection of communities of nodes (symptoms or manifestations of a studied construct) which make it possible to study item-level associations within and between communities of symptoms (Golino & Epskamp, 2017). It performs similarly to principal components analysis, factor analysis, and parallel analysis (Golino et al., 2020), replicating the findings of these methods (Bell & O’Driscoll, 2018) but also helping to discover new dimensions of constructs (Christensen et al., 2019a, 2019b). The residual network model (RNM) could investigate the fit of the latent structure of symptoms detected in EGA and simultaneously model the network of residuals of symptoms which are not explained by the latent variable (here: adherence to a community; Epskamp et al., 2017). This technique could help to investigate the associations between the dimensions of symptoms detected in EGA.
Using both CCA and network analysis could help distinguish the potential mechanisms of associations between self-compassion and OCD symptoms (CCA), and detect the boundaries between variables denoting compassionate self-reference, uncompassionate self-reference, and psychopathological symptoms (Christensen & Golino, 2021). Moreover, network analysis can also help to detect the most influential dimensions of self-compassion and the bridge symptom between (un)compassionate self-reference and OCD. These symptoms could be addressed in clinical practice by focusing on the deactivation of obsessive–compulsive symptoms through the strengthening of compassionate self-reference or reducing uncompassionate self-reference.
Method
Participants
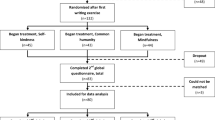
The following inclusion criteria were used: (1) age 18 or older; (2) fluent in Polish since the study was conducted in Polish. The exclusion criterion was having a clinical diagnosis of OCD. We recruited 447 individuals (286 women) ranging in age from 18 to 83 (M = 40.5; SD = 14.5). Due to their previous OCD diagnosis, a number of participants were excluded (n = 23); the final sample included 424 individuals (273 women) ranging in age from 18 to 83 (M = 41.0; SD = 14.5). Regarding socioeconomic status (SES), 45 individuals reported low SES (10.6%), while 77 reported high SES (18.2%). The majority of the participants reported having received a secondary (n = 110) or higher education (n = 282), while only 11 individuals had received only a primary education and 21 individuals had received a vocational education.
Procedure
All data were gathered using the snowball sampling method among Polish residents. The invitations to the online study were disseminated by posting on social media. The participants were informed of the study’s purpose and the conditions of participation. They participated voluntarily and without remuneration. First, demographic data were collected. Then, the participants were directed to questionnaires which were presented in randomized order. After completing the measures, the participants were thanked and informed again about the goals of the study, provided with contact with the principal investigator and with information about possible access to psychological aid in case it was necessary after the study.
Measures
Self-Compassion Scale
Self-compassion was measured using the 26-item Self-Compassion Scale (SCS; Neff, 2003a). This tool consists of 6 sub-scales referring to the components of the studied variable: Self-kindness (e.g., “I try to be loving towards myself when I’m feeling emotional pain”), Self-judgment (e.g., “I’m disapproving and judgmental about my own flaws and inadequacies”), Common humanity (e.g., “When things are going badly for me, I see the difficulties as part of life that everyone goes through”), Isolation (e.g., “When I think about my inadequacies, it tends to make me feel more separate and cut off from the rest of the world”), Mindfulness (e.g., “When something upsets me I try to keep my emotions in balance”), and Over-identification (e.g., “When I’m feeling down I tend to obsess and fixate on everything that’s wrong”). Each item is measured using a scale from 1 (Almost never) to 5 (Almost always). In the present study, we used the Polish version of the SCS (Kocur et al., 2022) which has high internal consistency (0.66 ≤ α ≤ 0.80) and convergent and divergent validity confirmed in previous studies in Polish samples (Paruzel-Czachura & Kocur, 2023). Cronbach’s α of the scale in the current study ranged between 0.73 (common humanity sub-scale and mindfulness sub-scale) and 0.83 (self-kindness).
The Obsessive–Compulsive Inventory—Revised
The Obsessive–Compulsive Inventory—Revised (Foa et al., 2002) includes 18 items measuring OCD symptoms: (a) Washing (e.g., “I find it difficult to touch an object when I know it has been touched by strangers or certain people”): 3 items; (b) Obsessing (e.g., “I find it difficult to control my own thoughts”): 3 items; (c) Hoarding (e.g., “I have saved up so many things that they get in the way”): 3 items; (d) Ordering (e.g., “I get upset if objects are not arranged properly”): 3 items; (e) Checking (e.g., “I check things more often than necessary”): 3 items, and (f) Neutralizing (e.g., “I feel compelled to count while I am doing things”): 3 items. Participants assess the items on a scale ranging from 0 (Not at all) to 4 (Extremely). In the present study, we used the Polish version of the OCI–R (Jeśka, 2012), which has been shown to have high internal consistency for the full scale and sub-scales (0.62 ≤ α ≤ 0.85) and satisfactory convergent and divergent validity (Brytek-Matera et al., 2020; Mojsa-Kaja et al., 2016). The reliability of OCI-R sub-scales in the present study ranged from 0.56 (hoarding) to 0.83 (neutralizing).
Data Analyses
The sample size was determined to be large enough to ensure stable estimates of correlation coefficients (n = 250) (Schönbrodt & Perugini, 2013). Having more than 250 participants was deemed appropriate for canonical correlation analysis given the expected rather moderate or large canonical correlations between self-compassion and obsessive–compulsive symptomatology (Lee, 2007).
First, we investigated descriptive statistics and bivariate correlations between all of the variables we studied. Second, we used CCA to detect canonical functions which represent coefficients of variables included in both sets (namely dimensions of self-compassion and OCD symptoms) on linear combinations (synthetic variables) for the observed variables. These functions are obtained so as to maximize the canonical correlation coefficient, namely the Pearson r relationship between the two synthetic variables on a given canonical function (Härdle & Simar, 2012). Canonical function coefficients represent the coefficients in linear combinations for variables in each set which were used to obtain the highest canonical correlation coefficients. The significance of the full CCA model and each correlation function was estimated using Wilk’s lambda and F statistics (Sherry & Henson, 2005). Inspection of standardized canonical function coefficients helps us interpret the meaning of the canonical correlation between self-compassion and OCD symptoms.
To detect communities of nodes in the network and investigate the associations between nodes, we used Exploratory Graph Analysis (EGA) based on a graphical Gaussian model (GGM; Golino & Epskamp, 2017) regularized via the graphical LASSO (Least Absolute Shrinkage and Selection Operator; glasso) algorithm which penalizes the lowest partial correlations (shrinking them to zero; Epskamp et al., 2018). Edges were estimated as partial correlations between nodes controlling for the effects of all the other nodes included in the network. Because of the large number of parameters (e.g., edge weights) to estimate, the regularization techniques are used to maintain a reasonable ratio of parameter and sample size. Glasso is one of the most frequently used methods of regularization in network psychometrics (Isvoranu and Epskamp, 2023). The level of penalization of partial correlations in the network is determined by the best fit of the model measured by the Extended Bayesian Information Criterion (EBIS; Chen & Chen, 2008) and controlled by the gamma hyperparameter. High levels of the hyperparameter (e.g., > 0.5) result in the selection of models which include only the strongest edges (penalizing spurious correlations between nodes), while values closer to zero retain less significant edges in the network (Epskamp et al., 2018). In the present study, we used 0.5 which is a default value in network analysis (Epskamp et al., 2012).
We estimated the stability of edges and centrality indices using the case-dropping procedure which quantifies how many participants could be dropped from the initial sample to maintain the correlation between the estimated networks as 0.7 or higher (Epskamp et al., 2018). We expected to achieve a correlation stability coefficient (CS) of 0.5 and higher to warrant the stability of the obtained networks (Epskamp et al., 2018). This value informs that after dropping 50% of the sample, the network computed in the smallest sub-sample is highly similar to the one estimated in the full sample.
The goals of network analysis were to (a) inspect whether items measuring self-compassion and obsessive–compulsive symptoms formed different communities of symptoms; (b) investigate the most central symptoms in the network of self-compassion and OCD symptoms; and (c) compare the centrality of all variables included in the network and distinguish the strongest edges (Epskamp et al., 2018). The communities of variables were investigated using the Louvain algorithm (Blondel et al., 2008) which performs better when detecting a higher number of communities in the network (Christensen & Golino, 2021). The centrality of the nodes was conceptualized in terms of (1) strength (the sum of the absolute value of connections with other nodes in the network); (2) closeness (the average shortest path between a given node and the remaining nodes in the network); and (3) expected influence (the summed weight of edges shared by a node with the remaining nodes in the network including positive and negative associations; Robinaugh et al., 2016). After detecting communities, we also investigated bridge expected influence centrality which does not reflect the absolute connections of a node with other nodes (strength), but signifies an overall increase of activation in other nodes connected to a given node (Jones et al., 2021). To compare the centrality of nodes in the network, we used bootstrap procedures based on resampling 1000 datasets from the data (Epskamp et al., 2018).
Lastly, we investigated the associations between the dimensions of self-compassion and OCD detected in EGA. We used confirmatory GGM and residual network modelling (Espkamp et al., 2017). Communities detected in EGA are statistically equivalent to latent factors (Golino et al., 2020), thus we used residual network analysis which makes it possible to investigate the fit of latent variables structure (adherence to a community) with simultaneous examination of the associations between residuals of items indicating latent variables (Epskamp et al., 2017). In the present study, we used the residual network model implemented in the psychonetrics package in R to investigate and visualize the latent structure of OCD symptoms and self-compassion manifestations. We were mostly interested in the associations within the network of latent variables, but also provisionally assessed the fit of the EGA-based community detection. We used variance–covariance matrices in estimating the residual network model. All analyses were conducted in R using the following packages: EGAnet (Christensen & Golino, 2021), bootnet (Epskamp et al., 2018), igraph (Csárdi and Nepusz, 2006), qgraph (Epskamp et al., 2012), and psychonetrics (Epskamp, 2023).
Results
Descriptive Statistics
Table 1 illustrates the mean, standard deviation, and correlations between dimensions of self-compassion and OCD. Study variables have skewness and kurtosis in the range between − 0.63 and 0.97, which could suggest a lacking violation of the normal distribution of data assumption (Hair et al., 2010).
Inspection of bivariate correlation suggested that Self-judgment, Isolation, and Over-identification were moderately positively associated with OCD symptoms (r = [0.10; 0.40]; p < 0.03; 95% CI = [0.01; 0.47]), while Self-kindness and Mindfulness were negatively, but to a relatively weak extent, associated with Obsessing, Hoarding, and Ordering (r = [− 0.11; − 0.25]; p < 0.02; 95% CI = [− 0.01; − 0.34]). Common humanity had positive associations with Washing (r = 0.12; p = 0.02; 95% CI = [0.02; 0.21]) and Neutralizing (r = 0.12; p = 0.02; 95% CI = [0.02; 0.21]). Both sets of variables were highly intercorrelated (Supplementary Material: Fig. S1 and S2).
Canonical Correlation Analysis
Canonical correlations and statistical significance of canonical functions are given in Table 2. Three canonical functions were significant and their canonical correlations explained 23.04%, 5.76%, and 4.41%, respectively, of shared variance between two sets of variables. Table 3 presents standardized canonical coefficients of all studied variables on the three significant canonical functions.
Standardized canonical function coefficients are analogous to beta weights in regression (Sherry & Henson, 2005). Thus, according to the inspection of canonical function coefficients, we can interpret the first canonical function as representing a higher risk of Obsessing and Hoarding among individuals with lower Self-kindness, higher Isolation, and higher Over-identification. The second function seems to reflect that higher Self-judgment and Over-identification, in combination with less Isolation, could be predictive of more Ordering and Checking. The last significant function reflects that less Self-kindness, less Self-judgment, less Isolation, but higher levels of Over-identification were associated with more Obsessing but less Neutralizing.
Network Analysis
There were no missing values in the network analysis, thus, the sample size used to compute networks was n = 424. Skewness and kurtosis of the SCS and OCI-R items ranged from − 0.33 to 1.20 and from − 1.02 to 0.58, respectively. These values indicate that the distributions of the items were close to normal (Byrne, 2010).
The initial EGA network was tested for the number and stability of detected communities and item allocation. The median number of detected communities was 4 (95% CI = 3.32–4.68), and the four-communities solution appeared in 87.8% of resampled data, whereas in 10.8% the five-communities solution appeared. Two out of four communities consisted of items reflecting compassionate self-reference and uncompassionate self-reference. The next two represent OCD symptoms and one community reflected mostly obsessing symptoms. However, three items from OCI-R had unstable allocations to communities (Table S1 in Supplementary Materials): the Hoarding item OCI-R 1 (“I have saved up so many things that they get in the way”) was allocated in 52% of the resampled data to OCD symptoms, similarly to the Hoarding item OCI-R 13 (“I avoid throwing things away because I am afraid I might need them later”), whereas Ordering item OCI-R 15 (“I need things to be arranged in a particular order”) was allocated in 66% of resampled data to obsessing community. Thus, we deleted these ambiguous items from the dataset and reran the EGA.
Variables included in the final EGA network formed four stable dimensions (median of dimensions = 4; 95% Me = [3.66; 4.40]): compassionate self-reference (items representing the SCS sub-scales: Self-kindness, Common humanity, and Mindfulness), uncompassionate self-reference (items representing the SCS sub-scales: Isolation, Over-identification, and Self-judgement), obsessing symptoms (consisting of three items from OCI-R measuring Obsessing and one measuring Hoarding), and symptoms of OCD (including Washing, Neutralizing, Ordering, and Checking items). Four dimensions were detected in 95.8% of iterations of community detection analysis (we performed all these analyses using the Walktrap algorithm and obtained exactly the same results regarding items dropped and further item allocations). All items had a stable allocation to a respective community (Fig. S3 in the Supplementary Materials). The estimates of edges (CSedges = 0.70) and centrality indices (CSstrength = 0.70; CScloseness = 0.70; CSexpectedInfluence = 0.70) stability enabled the analysis of the network (Fig. S4 in Supplementary materials). Results of the exploratory graph analysis (EGA) are given in Fig. 1 and in Fig. S5 in Supplementary materials.
Centrality of variables are given in Fig. 2 and in Table S2 in the Supplementary Materials. In terms of strength, Over-identification item SCS 2 (“When I’m feeling down I tend to obsess and fixate on everything that’s wrong,” strength = 1.69) and Self-kindness item SCS 19 (“I’m kind to myself when I’m experiencing suffering,” strength = 1.58) had a relatively central position in the network; however, Neutralizing item OCI-R 10 (“I feel I have to repeat certain numbers,” strength = 3.41) was the most central symptom of the network. Obsessing item OCI-R 6 (“I find it difficult to control my own thoughts,” closeness = 1.25), Hoarding item OCI-R 7 (“I collect things I don’t need,” closeness = 1.32), and Over-identification item SCS 2 (closeness = 1.55) were the most central symptoms in terms of closeness. Neutralizing item OCI-R 10 (expected influence = 3.05) and Obsessing item OCI-R 12 (“I am upset by unpleasant thoughts that come into my mind against my will,” expected influence = 1.07) were the most central ones regarding expected influence. The differences in centrality indices are given in Fig. S5 and Table S2 in the Supplementary Materials.
The significant associations between items belonging to the detected communities appeared between Over-identification item SCS2 and Obsessing item OCI-R 6 (pr = 0.12, p = 0.01) as well as between Mindfulness item SCS 22 (“When I’m feeling down I try to approach my feelings with curiosity and openness”) and Neutralizing item OCI-R 10 (pr = 0.10, p = 0.05). The majority of significant edges linked the items within the same community. The exact edge weights are given in the osf repository. The Obsessing items (OCI-R 6, 12, and 18) had the highest bridge expected influence centrality (0.31, 0.26, and 0.31, respectively), whereas Neutralizing symptom OCI-R 10 also had a high bridge expected influence (0.26; Fig. S6 in the Supplementary Materials).
To investigate the associations between the dimensions of compassionate self-reference, uncompassionate self-reference, obsessing, and other OCD symptoms, we used the residual network model in the psychonetrics package. We assessed the associations between latent variables representing four communities detected in EGA. The fit of the EGA-based latent network model was satisfactory (χ2 = 962.12, df = 707, p < 0.001, CFI = 0.97, TLI = 0.96, RMSEA = 0.03, 95% CI for RMSEA = [0.02–0.03]; Fig. S7 and S8 in the Supplementary Materials). The associations between the dimensions of self-compassion and OCD symptoms derived from the EGA are given in Fig. 3.
Diagram of the EGA-based confirmatory latent network model. The figure represents the central part of the confirmatory residual network model diagram: circles represent latent variables (symptom communities); edges represent their bidirectional interactions. Comp = compassionate self-reference, UnComp = uncompassionate self-reference, Obs = obsessing, OCD = OCD symptoms. All edges are significant at p < 0.001
The residual network model given in Supplementary Fig. S8 showed that after accounting for the latent structure of SC and OCD, residuals which were not explained by the latent variables (syndromes) were also associated. Although the goal of RNM was to investigate correlations between latent variables, analyzing the residual network was not within the scope of the manuscript. However, we can observe that manifestations of uncompassionate self-reference and OCD symptoms were additionally positively correlated at the item level (over and beyond the associations due to the latent structure of the nodes), whereas compassionate self-reference items were mostly correlated with uncompassionate self-reference items.
Discussion
The present study investigated associations between self-compassion and OCD symptoms using two multivariate analytical techniques: canonical correlation analysis (Sherry & Henson, 2005) and network psychometrics (Epskamp et al., 2018). In contrast to previous studies, in the current study, we were focused on the complex associations between dimensions of self-compassion (Neff, 2003a) and groups of symptoms of OCD (Foa et al., 2002). Based on previous studies, we expected negative associations between Self-kindness, Common humanity, Mindfulness, and OCD symptoms, and positive associations between Self-judgment, Isolation, Over-identification, and OCD symptoms (Leeuwerik et al., 2020). Using CCA, we expected to detect interpretable linear combinations of established dimensions of self-compassion (Neff, 2003a) and OCD (Foa et al., 1998) which might show the possible mechanisms responsible for previously observed associations between these two constructs (Eichholz et al., 2020). However, we also used network psychometrics to investigate the dimensionality of the studied constructs, particularly because of the ongoing debate on the internal structure of self-compassion and the nature of its association with psychopathological symptoms. We addressed this goal by using network psychometrics to investigate multilevel (item- and dimension-level) associations between self-compassion and OCD.
The correlational analysis only partially supported Hypothesis 1, while we found better support for Hypothesis 2. Thus, so-called negative dimensions of self-compassion (self-judgment, isolation, and over-identification) were positively associated with all groups of OCD symptoms. Self-kindness and mindfulness were negatively associated with obsessing and hoarding, while common humanity was not correlated with any OCD symptoms. The obtained results were generally consistent with previous meta-analytical findings about the higher importance of negative dimensions of self-compassion for psychopathological symptoms (Muris & Petrocchi, 2017). Wong and Mak (2013) showed that Self-kindness and Mindfulness had stronger associations with depression compared to Common humanity. Additionally, the results of the present study show that the protective role of self-kindness and mindfulness could be limited to particular types of OCD symptoms, namely obsessing and hoarding. Self-compassion was strongly negatively associated with thoughts-action fusion (Gillanders et al., 2015), which is one of the mechanisms that generate obsessions in OCD (Berle & Starcevic, 2005). Thus, self-kindness and mindfulness might foster an ability to let thoughts and things go and to avoid giving them too much emphasis.
Associations between Self-judgment, Isolation, and, even more importantly, Over-identification and OCD symptoms were more stable across various OCD symptoms. These associations could be interpreted with regard to common dysfunctional beliefs in OCD (Obsessive–Compulsive Cognitions Working Group [OCCWG], 1997) which are similar or homogeneous to beliefs present in self-judgment, over-identification, and isolation. For example, the inflated sense of responsibility underlying obsessions (OCCWG, 1997) is also present among individuals who score high on over-identification (Neff, 2003a). On the other hand, washing and neutralizing seem to be the OCD symptoms that are the least associated with the negative dimensions of self-compassion. This result could inform future studies on self-compassion-based interventions addressed to individuals suffering from OCD symptoms. It should be tested whether interventions focusing on reducing uncompassionate self-reference will be more effective for those OCD patients whose symptoms are obsessing and hoarding, but less effective for those who present mainly with washing or neutralizing symptoms. The results of such studies will be essential, because washing is a very common compulsion (Hunt, 2020), and self-compassion-based interventions could be less effective for a large group of patients who present with a predominance of this compulsion.
In the present study, we used multivariate analyses to investigate complex associations between self-compassion and OCD. First, we used CCA to detect canonical functions which could be interpreted as the particular mechanisms responsible for the general associations between self-compassion and OCD symptoms. The present study identified three such mechanisms. First, it showed that higher Self-kindness, lower Isolation, and lower Over-identification scores were associated with less Obsessing. This function explained the highest proportion of the variance shared by self-compassion and OCD. Thus, links between isolation, over-identification, and obsessing could be regarded as the major process responsible for associations between self-compassion and OCD. The second function exposed the unique associations between a combination of Self-judgment and Over-identification and OCD symptoms: Ordering and Checking, even when the Isolation was lower. This result could suggest that compulsions that include ordering and checking are mainly associated with excessive identification with responsibilities and a lack of kind self-reference. The last function combined high Over-identification and Obsessing, as well as high Self-judgment, with Neutralizing. These results are in line with previous research that used latent profile analysis and showed that different profiles of self-compassion traits have different associations with psychopathology (Phillips, 2021).
It is worth noting that the study showed more significant correlations between OCD symptoms and negative self-compassion components, compared to positive components of self-compassion. In the three distinct canonical functions, Common humanity and Mindfulness turned out to be irrelevant. This may add to the debate around the questionable legitimacy of analyzing SCS total score results and including the non-compassionate features (i.e., self-judgment, isolation, and over-identification) in the scale’s total score (Muris et al., 2018, 2019). According to the CCA results, dimensions representing compassionate self-reference were less important for OCD symptomatology, at least in the non-clinical group of the participants.
The network psychometrics approach, however, challenges the results of CCA. First, EGA did not confirm the six-dimensional structure of self-compassion (Neff, 2003a), but rather suggested two dimensions of compassionate self-reference and uncompassionate self-reference (Muris & Petrocchi, 2017) This finding reflects the reservations about treating reduced uncompassionate self-reference as a part of self-compassion and aggregating it with compassionate self-reference to form a single indicator of self-compassion (Muris & Otgaar, 2022).
Second, in the network consisting of manifestations of uncompassionate and compassionate self-reference and psychopathological symptoms, the most central symptoms were obsessing and neutralizing ones. Regarding the role of the central symptoms in the network (Robinaugh et al., 2016), the findings suggest that the presence of heightened obsessing or neutralizing symptoms could deactivate compassionate self-reference, but mostly activate uncompassionate self-reference. This result may be particularly important given that the study was conducted in a non-clinical sample. Based on the network theory of psychopathology (Borsboom, 2017), the appearance of a psychopathological symptom (such as obsessing) may strongly affect self-reference. However, the network consists of bidirectional associations, so we may also suggest that uncompassionate self-reference fosters obsessing and other OCD symptoms. This could be suggested because the over-identification symptoms (representing uncompassionate self-reference) were also central to the network in terms of strength and closeness, while the protective role of compassionate self-reference was less pronounced (self-kindness manifestation was relatively central only in terms of strength). These results are in line with previous findings showing that uncompassionate self-reference could be perceived as closer to psychopathology than to self-compassion (Muris et al., 2019). The lower centrality of (un)compassionate self-reference in the network, however, indicates that the appearance of psychopathological symptoms could hinder protective self-reference and foster uncompassionate self-reference.
Exploratory graph analysis showed that OCD symptoms were also grouped differently compared to the originally proposed six groups of symptoms (Foa et al., 1998). The present investigation showed two clusters of OCD symptoms: obsessing (including one hoarding symptom) and other OCD symptoms (including washing, neutralizing, checking, and ordering symptoms). Exclusion of hoarding resulting in a better fit of the OCI-R structures appeared in previous studies (Abramovitch et al., 2022; Angelakis et al., 2017). Studies on the higher-order structure of OCI-R also revealed that obsessing was less loaded by the total factor of OCD symptoms compared to the other symptoms (Abramovitch et al., 2020). The obtained grouping of OCD symptoms in the network including self-compassion symptoms may suggest that obsessing symptoms are a bridge between OCD symptoms and uncompassionate self-reference or a certain predisposition to develop other obsessive–compulsive symptomatology.
Results of network analysis support the expected association between over-identification symptoms and OCD symptoms, particularly with obsessing. Over-identification is defined as “being caught up in an exaggerated storyline about negative aspects of oneself or one’s life experience” (Neff, 2016, p. 265). At the item level, difficulties with controlling one’s thoughts when feeling down (Over-identification item SCS2) correlated with an Obsessing symptom of a very similar content (“I find it difficult to control my own thoughts”) bridging between the uncompassionate self-reference community and the obsessing community. This suggests a partial overlap between psychopathological symptoms and uncompassionate self-reference (Muris et al., 2016). However, we also found that a Self-kindness item (SCS22; trying to approach feelings with curiosity and openness when feeling down) correlated positively with a Neutralizing symptom (OCI-R10; repeating a certain number). This could indicate that some self-compassionate activities could have a neutralizing function, e.g., helping to improve lowered mood. Previous studies showed that neutralizing includes covert strategies, such as searching for “good” words, images, or thoughts, repeating certain words or sentences, and counting (Belloch et al., 2015). Thus, individuals aiming to neutralize their anxiety or bad feelings could use their ability to reinterpret internal experiences in a positive way to regulate mood.
Network analysis on a latent dimension level indicated that uncompassionate self-reference had a positive association with obsessing, whereas the associations between compassionate self-reference and obsessing or other OCD symptoms were non-significant. This result also supports the different roles of compassionate and uncompassionate self-reference for psychopathological symptoms showing that developing self-compassion may be regarded as insufficient to prevent psychopathological symptoms; the reduction of a lack of self-compassion appeared as a primary goal in psychopathology prevention.
The obtained results may add new insights to the methodology of studies on the links between self-compassion and psychopathology. First, the present study showed other arguments against highlighting six dimensions in the SCS, now from the network psychometrics point of view. EGA supports previous suggestions that the SCS captures two dimensions of compassionate self-reference as well as the correlated but independent dimension of uncompassionate self-reference (Muris et al, 2016). Despite theoretical claims about the legitimacy of distinguishing six dimensions of self-compassion (Neff, 2019), the present study is another one that confirms the two-dimensional model of the SCS. Second, we showed that the analysis of the associations between self-compassion and psychopathological symptoms should not use a single score of self-compassion computed as the sum of compassionate and reduced uncompassionate dimensions. EGA and the latent network model showed the different roles of compassionate and uncompassionate self-reference for psychopathological symptoms, stressing the importance of uncompassionate self-reference (similar observations had been previously made by Muris & Otgaar, 2022; Wong & Mak, 2013, for example). Third, the present study showed that the associations between manifestations of (un)compassionate self-reference and OCD symptoms should be studied on various levels. The latent network model showed that the EGA-based structure considerably fitted the data and indicated significant associations between uncompassionate self-reference and obsessing. However, in the residual network model at the item level, there were more nuanced associations between the manifestation of (un)compassionate self-reference and OCD symptoms after accounting for the latent structure. This means that beyond the associations due to the links between the constructs (of self-compassion or psychopathological syndromes), there are more sources of connections between particular psychopathological symptoms and manifestations of (un)compassionate self-reference (e.g., references to feeling down or similar phrasing of the items). Investigating and controlling these sources could reduce the measurement error in the networks of psychopathological symptoms and risk factors or preventive resources, but also suggest other interventions that can deactivate the development of OCD symptoms.
The results may be also important for future clinical studies. The findings about positive associations between obsessing and uncompassionate self-reference could result in examining the tailoring interventions for OCD patients with a dominant presentation of obsessive symptoms focusing on reducing over-identification. In this case, present interventions, including 8-week courses such as Mindfulness-Based Stress Reduction (MBSR) (Kabat-Zinn, 1990) or, more specifically, Mindfulness-Based Living Course (MBLC) (Choden & Regan-Addis, 2018), could benefit from a stronger focus on lowering over-identification.
Limitations and Future Directions
Although the study was one of the first which investigated associations between self-compassion and OCD symptoms multidimensionally, its limitation is that it underestimates a variety of obsessions and compulsions which may be present in OCD symptomatology (Hunt, 2020). Thus, future studies should use more comprehensive symptom checklists when measuring OCD symptoms (e.g., the Yale-Brown Obsessive–Compulsive Scale; Goodman et al., 1991). Second, the cross-sectional design of the study forbids any causal interpretations of the obtained results. Thus, future studies should investigate interventions targeting the development of particular dimensions of self-compassion (e.g., by introducing modules focused on replacing self-judgement with self-kindness to self-compassion therapeutic protocols) controlling for possible resulting changes in other dimensions (e.g., isolation or over-identification) in order to verify theirs impact on obsessive–compulsive symptoms. Future studies can also use longitudinal measurement to establish the temporal structure of mutual activations and deactivations of the uncompassionate self-reference, compassionate self-reference, and psychopathological symptoms. Third, future studies could also investigate the potential role of dysfunctional beliefs in mediating between self-compassion and OCD symptoms (Abramowitz, 2006).
Both analytic methods used, namely CCA and network analysis, also had their limitations. The main limitation of CCA in the present study was that it was conducted on the original dimensions of self-compassion and OCD. Given that EGA did not replicate the original structures of the SCS and the OCI-R, the results of CCA may disregard the doubts concerning the internal structure of both constructs. Relatively high correlations between some dimensions of the SCS and the OCI-R could also result in heightened collinearity in CCA. The limitation of network analysis in the present study involved the relatively low sample size regarding the number of variables included at the item level (Burger et al., 2023). However, the network was stable in terms of edges and centrality estimates (Epskamp et al., 2018). Other network analysis techniques, such as Bayesian GGM (Williams & Mulder, 2020), which require fewer assumptions (e.g., normal distributions of data) could be used in future studies. A significant limitation of network analysis is the lack of a separate sample for confirmatory GGM and the residual network model. Thus, the findings from the present study should be treated as preliminary. Moreover, other community detection techniques may be applied, such as spin glass. However, we prefer the Louvain algorithm because of its better performance in comparison to the Walktrap algorithm (Christensen & Golino, 2021), which was better than spin glass (de Sousa & Zhao, 2014).
Despite these limitations, the present study presents the differential associations between dimensions of self-compassion and symptoms of OCD. Additionally, based on CCA, we suggested three possible processes which might be responsible for the associations between self-compassion and OCD symptoms, which were the linear combination of dimensions of both constructs. This could supplement the results of network analysis, focused on partial correlations between variables rather than on complex linear associations between groups of variables. Regarding both analyses, we can draw similar conclusions, namely that OCD symptoms (mostly obsessing) were associated primarily with uncompassionate self-reference manifested by over-identification. However, we showed that the dimensions used in CCA should be previously verified as stable and valid indicators of the constructs tested. In the present study, we showed that three dimensions of compassionate self-reference and uncompassionate self-reference could be deemed to constitute two dimensions, whereas OCD symptoms could also be pooled into obsessing and OCD symptoms.
Data Availability
The data for current studies are publicly available at Open Science Framework: https://osf.io/kg8ua/?view_only=e66df288302042cfb9ed4ff1f983efd7.
Change history
22 December 2023
A Correction to this paper has been published: https://doi.org/10.1007/s12671-023-02284-4
References
Abramovitch, A., Abramowitz, J. S., Riemann, R. C., & McKay, D. (2020). Severity benchmarks and contemporary clinical norms for the Obsessive-Compulsive Inventory-Revised (OCI-R). Journal of Obsessive-Compulsive and Related Disorders, 27, 100557. https://doi.org/10.1016/j.jocrd.2020.100557
Abramovitch, A., Abramowitz, J. S., McKay, D., Cham, H., Anderson, K. S., Farrell, L., Geller, D. A., Hanna, G. L., Mathieu, S., McGuire, J. F., Rosenberg, D. R., Stewart, S. E., Storch, E. A., & Wilhelm, S. (2022). The OCI-CV-R: A revision of the Obsessive-Compulsive Inventory - Child Version. Journal of Anxiety Disorders, 86, 102532. https://doi.org/10.1016/j.janxdis.2022.102532
Abramowitz, J. S. (2006). The psychological treatment of obsessive-compulsive disorder. Canadian Journal of Psychiatry. Revue Canadienne de Psychiatrie, 51(7), 407–416. https://doi.org/10.1177/070674370605100702
Abramowitz, J. S., Franklin, M. E., Schwartz, S. A., & Furr, J. M. (2003). Symptom presentation and outcome of cognitive-behavioral therapy for obsessive-compulsive disorder. Journal of Consulting and Clinical Psychology, 71(6), 1049–1057. https://doi.org/10.1037/0022-006X.71.6.1049
Abramowitz, J. S., Taylor, S., & McKay, D. (2009). Obsessive-compulsive disorder. The Lancet, 374(9688), 491–499. https://doi.org/10.1016/S0140-6736(09)60240-3
Angelakis, I., Gooding, P., Tarrier, N., & Panagioti, M. (2015). Suicidality in obsessive compulsive disorder (OCD): A systematic review and meta-analysis. Clinical Psychology Review, 39, 1–15. https://doi.org/10.1016/j.cpr.2015.03.002
Angelakis, I., Panagioti, M., & Austin, J. L. (2017). Factor structure and validation of the Obsessive Compulsive Inventory-Revised (OCI-R) in a Greek non-clinical sample. Journal of Psychopathology and Behavioral Assessment, 39(1), 164–175. https://doi.org/10.1007/s10862-016-9575-5
Arimitsu, K., & Hofmann, S. G. (2015). Cognitions as mediators in the relationship between self-compassion and affect. Personality and Individual Differences, 74, 41–48. https://doi.org/10.1016/j.paid.2014.10.008
Basharpoor, S., Mowlaie, M., & Sarafrazi, L. (2021). The relationships of distress tolerance, self-compassion to posttraumatic growth, the mediating role of cognitive fusion. Journal of Aggression, Maltreatment & Trauma, 30(1), 70–81. https://doi.org/10.1080/10926771.2019.1711279
Bell, V., & O’Driscoll, C. (2018). The network structure of paranoia in the general population. Social Psychiatry and Psychiatric Epidemiology, 53(7), 737–744. https://doi.org/10.1007/s00127-018-1487-0
Belloch, A., Carrió, C., Cabedo, E., & García-Soriano, G. (2015). Discovering what is hidden: The role of non-ritualized covert neutralizing strategies in Obsessive-Compulsive Disorder. Journal of Behavior Therapy and Experimental Psychiatry, 49(Pt B), 180–187. https://doi.org/10.1016/j.jbtep.2015.02.006
Benatti, B., Dell’Osso, B., Shen, H., Filippou-Frye, M., Varias, A., Sanchez, C., Booil, J., Hollander, E., Fineberg, N. A., Stein, D. J., Nicolini, H., Lanzagorta, N., Marazziti, D., Pallanti, S., Van Ameringen, M., Lochner, C., Karamustafalioglu, O., Hranov, L., Figee, M., Drummond, L., … Rodriguez, C. I. (2021). Prevalence and correlates of current suicide risk in an international sample of OCD adults: A report from the International College of Obsessive-Compulsive Spectrum Disorders (ICOCS) network and Obsessive Compulsive and Related Disorders Network (OCRN) of the European College of Neuropsychopharmacology. Journal of Psychiatric Research, 140, 357–363. https://doi.org/10.1016/j.jpsychires.2021.05.054
Berle, D., & Starcevic, V. (2005). Thought-action fusion: Review of the literature and future directions. Clinical Psychology Review, 25(3), 263–284. https://doi.org/10.1016/j.cpr.2004.12.001
Blanken, T. F., Deserno, M. K., Dalege, J., Borsboom, D., Blanken, P., Kerkhof, G. A., & Cramer, A. O. J. (2018). The role of stabilizing and communicating symptoms given overlapping communities in psychopathology networks. Scientific Reports, 8(1), 5854. https://doi.org/10.1038/s41598-018-24224-2
Blondel, V. D., Guillaume, J. L., Lambiotte, R., & Lefebvre, E. (2008). Fast unfolding of communities in large networks. Journal of Statistical Mechanics: Theory and Experiment, 10, 1–12. https://doi.org/10.1088/1742-5468/2008/10/P10008
Borsboom, D. (2017). A network theory of mental disorders. World Psychiatry, 16(1), 5–13. https://doi.org/10.1002/wps.20375
Borsboom, D., & Cramer, A. O. (2013). Network analysis: An integrative approach to the structure of psychopathology. Annual Review of Clinical Psychology, 9, 91–121. https://doi.org/10.1146/annurev-clinpsy-050212-185608
Brytek-Matera, A., Staniszewska, A., & Hallit, S. (2020). Identifying the profile of orthorexic behavior and “normal” eating behavior with cluster analysis: A cross-sectional study among Polish adults. Nutrients, 12(11), 3490. https://doi.org/10.3390/nu12113490
Burger, J., Isvoranu, A. M., Lunansky, G., Haslbeck, J. M. B., Epskamp, S., Hoekstra, R. H. A., Fried, E. I., Borsboom, D., & Blanken, T. F. (2023). Reporting standards for psychological network analyses in cross-sectional data. Psychological Methods, 28(4), 806–824. https://doi.org/10.1037/met0000471
Byrne, B. M. (2010). Structural equation modeling with AMOS: Basic concepts, applications, and programming. Routledge.
Chase, T. E., Chasson, G. S., Hamilton, C. E., Wetterneck, C. T., Smith, A. H., & Hart, J. M. (2019). The mediating role of emotion regulation difficulties in the relationship between self-compassion and OCD severity in a non-referred sample. Journal of Cognitive Psychotherapy, 33(2), 157–168. https://doi.org/10.1891/0889-8391.33.2.157
Chen, J., & Chen, Z. (2008). Extended Bayesian information criteria for model selectionwith large model spaces. Biometrika, 95(3), 759–771. https://doi.org/10.1093/biomet/asn034
Choden, & Regan-Addis, H. (2018). Mindfulness based living course. O-Books.
Christensen, A. P., & Golino, H. (2021). Estimating the stability of psychological dimensions via bootstrap exploratory graph analysis: A Monte Carlo simulation and tutorial. Psych, 3(3), 479–500. https://doi.org/10.3390/psych3030032
Christensen, A. P., Cotter, K. N., & Silvia, P. J. (2019a). Reopening openness to experience: A network analysis of four openness to experience inventories. Journal of Personality Assessment, 101(6), 574–588. https://doi.org/10.1080/00223891.2018.1467428
Christensen, A. P., Gross, G. M., Golino, H. F., Silvia, P. J., & Kwapil, T. R. (2019b). Exploratory graph analysis of the Multidimensional Schizotypy Scale. Schizophrenia Research, 206, 43–51. https://doi.org/10.1016/j.schres.2018.12.018
Csárdi, G., & Nepusz, T. (2006). The igraph software package for complex network research. InterJournal Complex Systems, 1695, 1–9. http://igraph.sf
de Sousa, F.B., & Zhao, L. (2014). Evaluating and comparing the igraph community detection algorithms. 2014 Brazilian Conference on Intelligent Systems (pp. 408–413). https://doi.org/10.1109/BRACIS.2014.79
Eichholz, A., Schwartz, C., Meule, A., Heese, J., Neumüller, J., & Voderholzer, U. (2020). Self-compassion and emotion regulation difficulties in obsessive-compulsive disorder. Clinical Psychology & Psychotherapy, 27(5), 630–639. https://doi.org/10.1002/cpp.2451
Epskamp, S. (2023). Psychonetrics: Structural Equation Modeling and Confirmatory Network Analysis. R package version 0.12. http://psychonetrics.org/
Epskamp, S., Cramer, A. O., Waldorp, L. J., Schmittmann, V. D., & Borsboom, D. (2012). qgraph: Network visualizations of relationships in psychometric data. Journal of Statistical Software, 48(4), 1–18. https://doi.org/10.18637/jss.v048.i04
Epskamp, S., Rhemtulla, M., & Borsboom, D. (2017). Generalized network psychometrics: Combining network and latent variable models. Psychometrika, 82, 904–927. https://doi.org/10.1007/s11336-017-9557-x
Epskamp, S., Borsboom, D., & Fried, E. I. (2018). Estimating psychological networks and their accuracy: A tutorial paper. Behavior Research Methods, 50(1), 195–212. https://doi.org/10.3758/s13428-017-0862-1
Ewert, C., Vater, A., & Schröder-Abé, M. (2021). Self-Compassion and Coping: A Meta-Analysis. Mindfulness, 12(5), 1063–1077. https://doi.org/10.1007/s12671-020-01563-8
Ferrari, M., Hunt, C., Harrysunker, A., Abbott, M. J., Beath, A. P., & Einstein, D. A. (2019). Self-compassion interventions and psychosocial outcomes: A meta-analysis of RCTs. Mindfulness, 10(8), 1455–1473. https://doi.org/10.1007/s12671-019-01134-6
Fineberg, N. A., Hengartner, M. P., Bergbaum, C., Gale, T., Roessler, W., & Angst, J. (2013). Lifetime comorbidity of obsessive-compulsive disorder and sub-threshold obsessive-compulsive symptomatology in the community: Impact, prevalence, socio-demographic and clinical characteristics. International Journal of Psychiatry in Clinical Practice, 17(3), 188–196. https://doi.org/10.3109/13651501.2013.777745
Foa, E. B., Kozak, M. J., Salkovskis, P. M., Coles, M. E., & Amir, N. (1998). The validation of anew obsessive–compulsive disorder scale: The Obsessive-Compulsive Inventory. Psychological Assessment, 10(3), 206–214. https://doi.org/10.1037/1040-3590.10.3.206
Foa, E. B., Huppert, J. D., Leiberg, S., Langner, R., Kichic, R., Hajcak, G., & Salkovskis, P. M. (2002). The Obsessive-Compulsive Inventory: Development and validation of a short version. Psychological Assessment, 14(4), 485–496. https://doi.org/10.1037/1040-3590.14.4.485
Gillanders, D. T., Sinclair, A. K., MacLean, M., & Jardine, K. (2015). Illness cognitions, cognitive fusion, avoidance and self-compassion as predictors of distress and quality of life in a heterogeneous sample of adults, after cancer. Journal of Contextual Behavioral Science, 4(4), 300–311. https://doi.org/10.1016/j.jcbs.2015.07.003
Golino, H. F., & Epskamp, S. (2017). Exploratory graph analysis: A new approach for estimating the number of dimensions in psychological research. PLoS ONE, 12(6), e0174035. https://doi.org/10.1371/journal.pone.0174035
Golino, H., Shi, D., Christensen, A. P., Garrido, L. E., Nieto, M. D., Sadana, R., Thiyagarajan, J. A., & Martinez-Molina, A. (2020). Investigating the performance of exploratory graph analysis and traditional techniques to identify the number of latent factors: A simulation and tutorial. Psychological Methods, 25(3), 292–320. https://doi.org/10.1037/met0000255
Goodman, W., Rasmussen, S., Price, L., Mazure, L., Heninger, G., & Charney, D. (1991). Yale-Brown Obsessive Compulsive Scale (Y-BOCS). Verhaltenstherapie, 1(3), 226–233. https://doi.org/10.1159/000257973
Hair, J., Black, W. C., Babin, B. J., & Anderson, R. E. (2010). Multivariate data analysis (7th ed.). Pearson Educational International.
Härdle, W. K., & Simar, L. (2012). Canonical correlation analysis. In W. K. Härdle & L. Simar (Eds.), Applied multivariate statistical analysis (pp. 385–395). Springer. https://doi.org/10.1007/978-3-642-17229-8_15
Hunt, C. P. (2020). Differences in OCD symptom presentations across age, culture, and gender: A quantitative review of studies using the Y-BOCS symptom checklist. Journal of Obsessive-Compulsive and Related Disorders, 26, 100533. https://doi.org/10.1016/j.jocrd.2020.100533
Isvoranu, A.-M., & Epskamp, S. (2023). Which estimation method to choose in network psychometrics? Deriving guidelines for applied researchers. Psychological Methods, 28(4), 925–946. https://doi.org/10.1037/met0000439
Jeśka, M. (2012). Tools for measuring the symptoms of obsessive-compulsive disorder (application, properties, advantages and disadvantages). Neuropsychiatria. Przegląd Kliniczny, 9, 137–142.
Jones, P. J., Ma, R., & McNally, R. J. (2021). Bridge centrality: A network approach to understanding comorbidity. Multivariate Behavioral Research, 56(2), 353–367. https://doi.org/10.1080/00273171.2019.1614898
Kabat-Zinn, J. (1990). Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. Bantam.
Keng, S. L., Seah, S. T., Tong, E. M., & Smoski, M. (2016). Effects of brief mindful acceptance induction on implicit dysfunctional attitudes and concordance between implicit and explicit dysfunctional attitudes. Behaviour Research and Therapy, 83, 1–10. https://doi.org/10.1016/j.brat.2016.05.004
Kocur, D., Flakus, M., & Fopka-Kowalczyk, M. (2022). Validity and reliability of the Polish version of the Self-Compassion Scale and its correlates. PLoS ONE, 17, e0267637. https://doi.org/10.1371/journal.pone.0267637
Lee, H. S. (2007). Canonical correlation analysis using small number of samples. Communications in Statistics – Simulation and Computation, 36(5), 973–985. https://doi.org/10.1080/03610910701539443
Leeuwerik, T., Cavanagh, K., & Strauss, C. (2020). The association of trait mindfulness and self-compassion with obsessive-compulsive disorder symptoms: Results from a large survey with treatment-seeking adults. Cognitive Therapy and Research, 44, 120–135. https://doi.org/10.1007/s10608-019-10049-4
MacBeth, A., & Gumley, A. (2012). Exploring compassion: A meta-analysis of the association between self-compassion and psychopathology. Clinical Psychology Review, 32(6), 545–552. https://doi.org/10.1016/j.cpr.2012.06.003
Marsh, I. C., Chan, S. W. Y., & MacBeth, A. (2018). Self-compassion and psychological distress in adolescents – a meta-analysis. Mindfulness, 9(4), 1011–1027. https://doi.org/10.1007/s12671-017-0850-7
Marshall, E. J., & Brockman, R. N. (2016). The relationships between psychological flexibility, self-compassion, and emotional well-being. Journal of Cognitive Psychotherapy, 30, 60–72. https://doi.org/10.1891/0889-8391.30.1.60
Mojsa-Kaja, J., Golonka, K., & Gawłowska, M. (2016). Preliminary analyses of psychometric characteristics of the Polish version of the Obsessive-Compulsive Inventory-Revised (OCI-R) in a non-clinical sample. International Journal of Occupational Medicine and Environmental Health, 29(6), 1011–1021. https://doi.org/10.13075/ijomeh.1896.00792
Muris, P., & Otgaar, H. (2022). Deconstructing self-compassion: How the continued use of the total score of the Self-Compassion Scale hinders studying a protective construct within the context of psychopathology and stress. Mindfulness, 13(6), 1403–1409. https://doi.org/10.1007/s12671-022-01898-4
Muris, P., & Petrocchi, N. (2017). Protection or vulnerability? A meta-analysis of the relations between the positive and negative components of self-compassion and psychopathology. Clinical Psychology and Psychotherapy, 24(2), 373–383. https://doi.org/10.1002/cpp.2005
Muris, P., van den Broek, M., Otgaar, H., Oudenhoven, I., & Lennartz, J. (2018). Good and bad sides of self-compassion: A face validity check of the Self-Compassion Scale and an investigation of its relations to coping and emotional symptoms in non-clinical adolescents. Journal of Child and Family Studies, 27, 2411–2421. https://doi.org/10.1007/s10826-018-1099-z
Muris, P., Otgaar, H., & Pfattheicher, S. (2019). Stripping the forest from the rotten trees: Compassionate self-responding is a way of coping, but reduced uncompassionate self-responding mainly reflects psychopathology. Mindfulness, 10(1), 196–199. https://doi.org/10.1007/s12671-018-1030-0
Neff, K. (2003a). The development and validation of a scale to measure self-compassion. Self and Identity, 2(3), 223–250. https://doi.org/10.1080/15298860309027
Neff, K. (2003b). Self-compassion: An alternative conceptualisation of a healthy attitude toward oneself. Self and Identity, 2(2), 85–101. https://doi.org/10.1080/15298860309032
Neff, K. D. (2016). “The Self-Compassion Scale is a valid and theoretically coherent measure of self-compassion”: Erratum. Mindfulness, 7(4), 1009. https://doi.org/10.1007/s12671-016-0560-6
Neff, K. D. (2019). Setting the record straight about the Self-Compassion Scale. Mindfulness, 10(1), 200–202. https://doi.org/10.1007/s12671-018-1061-6
Neff, K. D. (2020). Commentary on Muris and Otgaar (2020): Let the empirical evidence speak on the Self-Compassion Scale. Mindfulness, 11(8), 1900–1909. https://doi.org/10.1007/s12671-020-01411-9
Obsessive Compulsive Cognitions Working Group. (1997). Cognitive assessment of obsessive-compulsive disorder. Behaviour Research and Therapy, 35(7), 667–681. https://doi.org/10.1016/S0005-7967(97)00017-X
Olatunji, B. O., Davis, M. L., Powers, M. B., & Smits, J. A. (2013). Cognitive-behavioral therapy for obsessive-compulsive disorder: A meta-analysis of treatment outcome and moderators. Journal of Psychiatric Research, 47(1), 33–41. https://doi.org/10.1016/j.jpsychires.2012.08.020
Paruzel-Czachura, M., & Kocur, D. (2023). Do meditation, mindfulness, and self-compassion impact utilitarian moral judgment? Mindfulness, 14(7), 1650–1661. https://doi.org/10.1007/s12671-023-02161-0
Petrocchi, N., Cosentino, T., Pellegrini, V., Femia, G., D’Innocenzo, A., & Mancini, F. (2021). Compassion-focused group therapy for treatment-resistant OCD: Initial evaluation using a multiple baseline design. Frontiers in Psychology, 11, 594277. https://doi.org/10.3389/fpsyg.2020.594277
Phillips, W. J. (2021). Self-compassion mindsets: The components of the self-compassion scale operate as a balanced system within individuals. Current Psychology, 40, 5040–5053. https://doi.org/10.1007/s12144-019-00452-1
Phillips, W. J., & Hine, D. W. (2021). Self-compassion, physical health, and health behaviour: A meta-analysis. Health Psychology Review, 15(1), 113–139. https://doi.org/10.1080/17437199.2019.1705872
Quinlan, K. (2021). The self-compassion workbook for OCD. Lean into your fear, manage difficult emotions, and focus on recovery. New Harbinger Publications.
Robinaugh, D. J., Millner, A. J., & McNally, R. J. (2016). Identifying highly influential nodes in the complicated grief network. Journal of Abnormal Psychology, 125(6), 747–757. https://doi.org/10.1037/abn0000181
Schönbrodt, F. D., & Perugini, M. (2013). At what sample size do correlations stabilise? Journal of Research in Personality, 47(5), 609–612. https://doi.org/10.1016/j.jrp.2013.05.009
Sherry, A., & Henson, R. K. (2005). Conducting and interpreting canonical correlation analysis in personality research: A user-friendly primer. Journal of Personality Assessment, 84(1), 37–48. https://doi.org/10.1207/s15327752jpa8401_09
Skapinakis, P., Politis, S., Karampas, A., Petrikis, P., & Mavreas, V. (2019). Prevalence, comorbidity, quality of life and use of services of obsessive-compulsive disorder and subthreshold obsessive-compulsive symptoms in the general adult population of Greece. International Journal of Psychiatry in Clinical Practice, 23(3), 215–224. https://doi.org/10.1080/13651501.2019.1588327
Smeets, E., Neff, K., Alberts, H., & Peters, M. (2014). Meeting suffering with kindness: Effects of a brief self-compassion intervention for female college students. Journal of Clinical Psychology, 70(9), 794–807. https://doi.org/10.1002/jclp.22076
Suh, H., & Jeong, J. (2021). Association of self-compassion with suicidal thoughts and behaviors and non-suicidal self injury: A meta-analysis. Frontiers in Psychology, 12, 633482. https://doi.org/10.3389/fpsyg.2021.633482
Thompson, B. (1991). A primer on the logic and use of canonical correlation analysis. Measurement and Evaluation in Counseling and Development, 24(2), 80–95.
Turk, F., & Waller, G. (2020). Is self-compassion relevant to the pathology and treatment of eating and body image concerns? A systematic review and meta-analysis. Clinical Psychology Review, 79, 101856. https://doi.org/10.1016/j.cpr.2020.101856
Wadsworth, L. P., Forgeard, M., Hsu, K. J., Kertz, S., Treadway, M., & Björgvinsson, T. (2018). Examining the role of repetitive negative thinking in relations between positive and negative aspects of self-compassion and symptom improvement during intensive treatment. Cognitive Therapy and Research, 42, 236–249. https://doi.org/10.1007/s10608-017-9887-0
Wahl, K., Ehring, T., Kley, H., Lieb, R., Meyer, A., Kordon, A., Heinzel, C. V., Mazanec, M., & Schönfeld, S. (2019). Is repetitive negative thinking a transdiagnostic process? A comparison of key processes of RNT in depression, generaliszed anxiety disorder, obsessive-compulsive disorder, and community controls. Journal of Behavior Therapy and Experimental Psychiatry, 64, 45–53. https://doi.org/10.1016/j.jbtep.2019.02.006
Wakelin, K. E., Perman, G., & Simonds, L. M. (2022). Effectiveness of self-compassion-related interventions for reducing self-criticism: A systematic review and meta-analysis. Clinical Psychology & Psychotherapy, 29(1), 1–25. https://doi.org/10.1002/cpp.2586
Wetterneck, C. T., Lee, E. B., Smith, A. H., & Hart, J. M. (2013). Courage, self-compassion, and values in obsessive-compulsive disorder. Journal of Contextual Behavioral Science, 2(3–4), 68–73. https://doi.org/10.1016/j.jcbs.2013.09.002
Williams, D. R., & Mulder, J. (2020). BGGM: Bayesian Gaussian graphical models in R. Journal of Open Source Software, 5(51), 2111. https://doi.org/10.21105/joss.02111
Wilson, A. C., Mackintosh, K., Power, K., & Chan, S. W. Y. (2019). Effectiveness of self-compassion related therapies: A systematic review and meta-analysis. Mindfulness, 10(6), 979–995. https://doi.org/10.1007/s12671-018-1037-6
Wong, C. C., & Mak, W. W. (2013). Differentiating the role of three self-compassion components in buffering cognitive-personality vulnerability to depression among Chinese in Hong Kong. Journal of Counseling Psychology, 60(1), 162–169. https://doi.org/10.1037/a0030451
Zessin, U., Dickhäuser, O., & Garbade, S. (2015). The relationship between self-compassion and well-being: A meta-analysis. Applied Psychology: Health and Well-Being, 7(3), 340–364. https://doi.org/10.1111/aphw.12051
Acknowledgements
We are grateful for the voluntary effort of all our participants, without whom this project could not have happened.
Author information
Authors and Affiliations
Contributions
Conceptualization; data curation; methodology; formal analysis; writing: original draft preparation; writing: review and editing—Marcin Moroń.
Writing: original draft preparation; review and editing—Dagna Kocur.
Corresponding author
Ethics declarations
Ethics Approval
The study was approved by the Ethics Committee of the University of Silesia. The consent was given in written form (number of decision: KEUS 244/04.2022).
Informed Consent
Written informed consent was obtained from all participants prior to participation.
Conflict of Interest
The authors declare no competing interests.
Use of Artificial Intelligence
We did not use AI tools in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised as Dr Moroń should also be affiliated to affiliation 2.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Moroń, M., Kocur, D. Self-Compassion and Obsessive–Compulsive Symptoms in a Non-Clinical Sample: Insights from Network Analysis and Canonical Correlation Analysis. Mindfulness 14, 3052–3068 (2023). https://doi.org/10.1007/s12671-023-02256-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12671-023-02256-8