Abstract
Objectives
This nonrandomized trial investigated the feasibility and mental health outcomes associated with a mindfulness family caregiver (MFC) training program delivered online.
Method
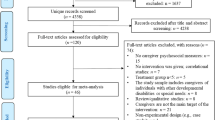
The study included 216 family caregivers (85.2% female; mean age = 57.34, SD = 12.87; 83.4% White, 2.8% Black, 12% Asian, 8.1% Hispanic, 1.8% American Indian/Alaska Native) who enrolled in the weekly, 4-session MFC training and completed self-report assessments at baseline, 1-month later at pre-training, and immediately after the MFC training. Feasibility was assessed in six domains (acceptability, demand, implementation, practicality, expansion, and limited efficacy) using self-reports and program attendance.
Results
The program was feasible in six domains. For feasibility, 70% of participants completed ≥ 75% of the training, with high rates of endorsement of training facets. For mental health outcomes, MFC was associated with significant improvement in depression (Hedges’ g = 0.49), anxiety (g = 0.64), caregiver burden (g = 0.51), and positive affect/well-being (g = 0.56). There was also evidence of increased physical (g = 0.19) and emotional (g = 0.19) health in caregivers.
Conclusions
A brief, 4-week, online group mindfulness training may be feasible and effective in reducing caregiver burden and enhancing psychological well-being in family caregivers.
Preregistration
The study is preregistered at Open Science Framework (https://osf.io/twz58/).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The burden of caregiving has fallen disproportionately on family members and friends as societies face a demographic shift toward an aging population (King et al., 2013). Research suggests that nearly one in five US adults provides unpaid care for an adult with health or functional disabilities (AARP & National Alliance for Caregiving, 2020). Increasingly, these care recipients have more comorbidities including long-term physical conditions, mental health issues, memory problems, and dementia that require extensive care. Not only will more adults find themselves in the role of caregiver, but they will also provide care for adults with increasingly complex needs, with many conducting care tasks in the home that were previously in the purview of medical or nursing professionals. The demands of this role exert an increasing toll on the physical (Marks et al., 2008), psychological (Carruth et al., 1997; Kang, 2006), psychosocial (AARP, 2020), and the financial well-being of caregivers (Bertrand et al., 2006; Gwyther & George, 1986) and might ultimately compromise the quality of care that they are providing to their care recipients (Zarit & Whitlatch, 1992). These concerning trends in declining caregiver and care recipient health underscore the importance of providing additional support to caregivers—and especially to those involved in complex care—as these problems may exacerbate with age.
Multiple factors are theorized to influence caregiver burden, including the frequency of unpredictable behaviors, lack of support, sense of disconnection, and the unpredictability of the care recipient (Clyburn et al., 2000; Haley et al., 1987). A growing body of evidence supports a model linking caregiver burden to individual appraisal of the burden (Pearson et al., 1993; Song et al., 1997). This underscores the importance of training that promotes coping skills and stress management techniques of the caregiver (Stones et al., 1997).
Mindfulness-based interventions (MBIs) have been shown to successfully promote resiliency for caregivers by reducing stress, anxiety, and nurturing a sense of interpersonal connection (Jaffray et al., 2016). A systematic review of Mindfulness-Based Stress Reduction (MBSR) for family caregivers suggests it is effective for promoting psychological well-being in a variety of caregivers, including those caring for individuals with dementia, chronic conditions, or children with disabilities (Shrank et al., 2011). Research on other MBIs suggests that an adapted 7-week Mindfulness-Based Cognitive Therapy for family caregivers for individuals with dementia was as effective at reducing stress as a standard educational training (Jaffray et al., 2016). Thus, there is converging evidence for the use of mindfulness skills training to help caregivers to sustain their psychological well-being.
Nevertheless, caregivers report barriers to engaging in in-person trainings including cost, lack of time (Lee et al., 2003; Shrank et al., 2011), distance, and lack of transportation (Kubo et al., 2019). Therefore, it is critically important to identify training that is accessible, cost-effective, and sensitive to the needs of caregivers. Evidence suggests that 60% of caregivers in the USA report already using the internet to support themselves in providing caregiving (AARP, 2020). Online delivery of MBIs is feasible and effective at supporting informal caregivers and helping them circumvent these multiple barriers to engagement (Li et al., 2016). One non-standardized 8-week online mindfulness meditation training with home practice reduced caregiver burden, perceived stress, anxiety, and loneliness and improved mental well-being for caregivers in the community (Tkatch et al., 2017). Online MBIs hint at scalability, feasibility, and cost-effectiveness of internet-delivered training for informal caregivers.
The goals of the present study were to examine the feasibility of conducting mindful family caregiving (MFC) training—a once-weekly 4-session online mindfulness-based training for family caregivers and to investigate the effects of MFC on caregiver mental health and well-being. To assess feasibility of the training, we assessed attendance and participants’ experience with the training immediately and 1-month post-training. We expected that at least 80% participants would attend ≥ 75% (three of four sessions) of the training (Hypothesis 1). We also expected that MFC would be associated with significant decreases in self-reported symptoms of depression, anxiety, and caregiver burden, as well as significant increases in positive affect and well-being (Hypothesis 2).
Method
Participants
Participants had to self-identify as current informal caregivers for a family member or friend, be at least 21 years of age, be able to join the training sessions online with video, and be willing to attend all four sessions. We used no other inclusion/exclusion criteria. Eligibility was kept broad as the skills taught in the MFC program are relevant to all family caregivers and the course is designed purposely to support caregivers to apply approaches in their own specific circumstances. Furthermore, family caregivers have found shared emotional ground despite numerous differences in their situations and who they care for. In contrast, a noticeable difference in caregiving experience arises between family caregivers and those who are caring for a recipient in a professional capacity (home health aide, medical practitioner). Consequently, we excluded all formal or professional caregivers from the study.
As shown in Table 1, caregivers were generally female, older, and well-educated. More than 90% of participants were family-related caregivers with approximately equivalent proportions of parents, partners, or adult offspring. Only 54.5% of caregivers were currently working full- or part-time. More than 76% of participants already used mindfulness practices regularly or occasionally.
Procedure
We recruited community-dwelling participants via community and national caregivers’ organizations, social media, and community outreach during the spring (Wave 1: March) and fall (Wave 2: September) of 2021. Each participant was given a unique identification number and link to access the online baseline assessment of self-reported psychological functioning delivered using Survey Monkey software on a secure computer server. All data were collected online. Responses were linked to the identification number and not to name or other identifying information. Only the research team had access to participant responses.
Participants completed self-report measures that assessed depression, anxiety, caregiving burden, positive affect/well-being, and current physical and emotional health at baseline (Time 1), 1-month later at pre-training (Time 2), and immediately post-training (Time 3). After completing the Time 2 assessments, participants began the once-weekly, 4-session group MFC training delivered online via Zoom. The MFC training was offered at no cost to participants. Participants had the option to provide course ratings at post-training (Time 4). Participants completed the follow-up assessment during the spring (Wave 1: May) and fall (Wave 2: November) of 2021.
Mindful Family Caregiving Training
The online Mindful Family Caregiving program is a group intervention developed specifically for people caring for friends or family members by the non-profit Zen Caregiving Project (ZCP; https://zencaregiving.org/). The course is focused on training mindfulness-based practices in each of the four sessions to enhance emotional resilience and reduce stress and anxiety in caregivers. The course teaches mindful awareness in the context of family caregiving, drawn from traditional Zen and Vipassana Buddhist practices, with an emphasis on self-kindness and compassion. MFC consists of four, once-weekly 2-hr sessions, for a total of 8 hr of training. At the end of each session, participants were emailed a handout recapping the material and detailing the session homework. Each session followed a lesson plan that includes instructional teaching, guided meditation, interactive activities, and group discussion.
The first session introduces mindfulness and the subsequent sessions cover compassion, loss, and healthy boundaries. Mindfulness is the foundation of all of the teachings. All sessions begin with a mindfulness meditation with space for participants to comment on their meditation experience and for instructors to address barriers to the practice of cultivating mindful awareness. Throughout the sessions, instructors emphasize how mindful awareness is not only relevant but the foundation of compassion, processing loss, and maintaining healthy boundaries. For instance, in the compassion session, participants are taught that the first stage of experiencing compassion is mindful awareness and that the most important piece of overcoming barriers to compassion is to be aware of how barriers are showing up in emotions, physical sensations, and thoughts. Each additional topic builds on the initial mindfulness module deepening an understanding of the principles of mindfulness practice. Further information on the MFC course is available here: https://zencaregiving.org/mindful-caregiving-education-explained/.
The sessions were conducted live via Zoom by one of two highly experienced instructors, each of whom has taught the ZCP’s Mindful Caregiving Education curriculum > 100 times. Each cohort consisted of groups of less than 30 participants based on schedule availability. At the end of the MFC training, participants were given the opportunity to share contact information with other group participants. Participants were offered a US$25 Amazon gift card voucher if they attended at least 3 of the 4 course sessions and completed the three assessment time points. We used an adherence checklist that identified specific content to be taught in each of the four sessions of MFC and used this tool to assess instructor adherence to the MFC protocol.
Measures
Feasibility
We assessed the feasibility of this program using the framework developed by Bowen et al. (2009). Of the eight domains in the framework, we assessed six domains. Acceptability was assessed by the participants’ overall training experience and if they would have a more positive view of healthcare providers who offered this program. Demand was operationalized as whether participants would recommend the program to other caregivers. Implementation was assessed by participant attendance. Program completion was defined as attending three out of four sessions. Practicality was assessed by the ability of participants to use mindfulness in caregiving activities, cope with caregiving challenges, improve the care they provide, and take better care of themselves. Expansion of the program to an online format was assessed by overall training experience rating. Limited efficacy was operationalized by the effect sizes of the program on primary and secondary outcome measures, including caregiver burden, general anxiety, life satisfaction, and depression.
Primary Outcome Measures
All participants completed self-report measures at each of the three time points (baseline, pre-training, and post-training). We used the Short-Form Zarit Burden Interview (ZBI-12) (Bédard et al., 2001) to assess the severity of caregiver burden. The original 29-item was published in 1980 to evaluate the impact of caregiving on the caregiver’s health, personal and social life, financial situation, emotional well-being, and interpersonal relationships (Zarit et al., 1980). Subsequent reductions have resulted in the ZBI-12 which is scored on a 5-point scale (0 to 4; Never, rarely, sometimes, quite frequently, nearly always). Items are summed to generate a total score with a range from 0 to 48. The suggested guidelines for scoring are as follows: 0–10: no to mild burden, 10–20: mild to moderate burden, and > 20: high burden. The ZBI-12 has shown good internal consistency and validity in older caregivers (Gratão et al., 2019). In our study, Cronbach’s alpha at baseline was excellent (Cronbach’s alpha (α) = 0.92; McDonald’s omega (ω) = 0.92).
Secondary Outcome Measures
To measure anxiety symptoms, we used the Generalized Anxiety Disorder 7-item (GAD-7) (Spitzer et al., 2006). The total score is calculated by assigning scores of 0, 1, 2, and 3 to the response categories, respectively, to four response options: not at all, several days, more than half the days, and nearly every day. GAD-7 total score for the seven items ranges from 0 to 21. In our study, internal reliability at baseline was excellent (α = 0.90; ω = 0.90).
Positive Affect and Well-Being—Short-Form 9 items (PAW-9) (Salsman et al., 2013) from the neurology quality of life (Neuro-QOL) measurement system consists of 9 items scored on a 5-point scale: 1 to 5. It measures aspects of a person’s life that relate to a sense of well-being, life satisfaction, or an overall sense of purpose and meaning. Cronbach’s alpha at baseline was excellent (α = 0.90; ⍵ = 0.90).
We used the Patient Health Questionnaire‐2 (PHQ‐2) (Kroenke et al., 2003) as a brief screener for depression disorders. It consists of a 4-point scale (0 to 3) to assess the presence over the last two weeks of two distinct depression symptoms: not at all, several days, more than half the days, nearly every day. Scores range from 0 to 6. The recommended cut point is a score of 3 or greater for symptoms consistent with major depression. Cronbach’s alpha at baseline was very good (α = 0.86). The PHQ‐2 consists of the first 2 questions of the PHQ‐9. The PHQ-2 is used as a screening instrument alone and an elevated score on the PHQ-2 would not be sufficient to initiate treatment or make a full diagnosis. The PHQ-9 would be the preferred instrument to follow up for a definitive diagnosis of a depressive disorder.
We collected one-item ratings from caregivers at post-training to assess current self-rated emotional and physical health based on a 5-point Likert scale: Excellent, Very Good, Good, Fair, Poor (Hays et al., 2015). Additionally, to better understand the impact of the MFC training experience, participants were invited to rate the MFC program on a 1 to 5 Likert scale (very likely to very unlikely) upon completion with respect to the following questions: “The training will help me take better care of myself”; “The training will likely improve the care that I provide to others”; “The training made me feel more connected to other caregivers”; “The training helped me recognize how to use mindfulness in my caregiving activities”; “The training helped me learn more about mindfulness”; “The training made me feel better able to cope with caregiving challenges that may arise”; “How likely is it that you would recommend this training to other caregivers?”; “If this course was offered to you by the health provider of the person you care for, would your view be more positive?”.
Data Analyses
We used SPSS v28 to conduct an analysis to identify missing data at pre-training (Time 2) and post-training (Time 3) relative to baseline (Time 1). We first used Little’s missing completely at random (MCAR) test (Little, 1988) to conduct a missing at random analysis for dependent variables at pre-training and post-training to determine which type of imputation of missing data to use.
Our analysis of missing data revealed that relative to 216 participants at baseline (Time 1), at pre-training (Time 2), there were 16 (7.4%) caregiver burden, 18 (8.3%) depression screener, 8 (3.7%) anxiety symptoms, and 18 (8.3%) positive affect and well-being missing responses. Overall, 8.3% of all participants had missing values and 6.9% of all values (i.e., all possible responses on questionnaires) were incomplete at pre-training. Little’s MCAR test confirmed that the data for each of these four dependent variables were missing at random, chi-square = 3.07, df = 3, p = 0.38, suggesting that there was no systematic bias in responders. There was no evidence of monotonicity in the missing data; therefore, we used the Markov chain Monte Carlo (MCMC) method. Thus, we used multiple imputation to impute values for missing responses for the four dependent variables at pre-training (Time 2).
Relative to 216 baseline (Time 1) participants, at post–MFC training (Time 3) there were 50 (23.1%) caregiver burden, 49 (22.7%) depression screener, 50 (23.1%) anxiety symptoms, and 50 (23.1%) positive affect and well-being missing responses. Little’s MCAR test confirmed that the data for each of these 4 dependent variables were missing at random, chi-square = 0.56, df = 1, p = 0.45, suggesting that there was no systematic bias in responders.
We used SPSS multiple imputation (regression method) to generate multiple simulations based on patterns in the available data to replace missing data with imputed values and thus create a full dataset. The data were missing at random (i.e., there was no evidence of monotonicity in the missing data). First, we used the fully conditional specification with 20 iterations with the 4 dependent variables (DVs) at Time 1 as predictors only, and 4 DVs at Time 2 as predictors and imputed variables. Then we used the fully conditional specification with 20 iterations with the 4 DVs at Time 2 as predictors only, and 4 DVs at Time 3 as predictors and imputed variables to obtain the pooled results of imputed data.
For the analysis of feasibility (Hypothesis 1), we examined rates of attendance of the four sessions of the MFC program. We also investigated responses about the MFC training program reported post-training completion, including overall rating of MFC, and whether participants would recommend MFC to other caregivers.
For the analysis of training outcome (Hypothesis 2), we used within-group paired t-tests to examine changes from baseline to pre-training, and pre- to post-training. We report Hedges’ g as an index of the size of the effect of MFC on changes in self-reported symptoms of depression, anxiety, caregiver burden, positive affect, and well-being. We also tested the robustness of our results using a linear mixed model (LMM) to examine pre- to post-training related change in the primary outcome variable, caregiver burden. Data analytic methods and results are reported in the “Supplementary Information” section.
We also conducted exploratory analyses to determine if any baseline characteristics of participants were associated with pre- to post-MFC changes in severity of caregiver burden, the primary outcome variable. We also investigated whether reduction in caregiver burden was associated with the Time 3 responses for any of the MFC program evaluation ratings.
Results
Preliminary Analyses
To determine whether we had an empirical basis for combining Wave 1 and 2 data, we conducted between-group analyses on the four self-report measures at baseline (Time 1) and on the pre- to post-MFC changes. There were no significant between-group differences at baseline (all p-values > 0.60) and in pre- to post-MFC change scores (all p-values > 0.25) for any of the four self-report measures. Furthermore, we tested whether there was a teacher effect by comparing the effect of teacher 1 vs 2 on the pre-to-post training changes on the four dependent variables. There were no significant between-teacher effects with all p-values > 0.50. Thus, we analyzed the data from all the participants as one group.
On average, participants reported a high caregiving burden as indicated by providing caregiving most days of the week (M = 5.35, SD = 2.15, range 1 to 7 days) for many hours per day (M = 6.87, SD = 6.38, range 1 to 24 hr). At baseline, there was a significant association between days per week of caregiving and caregiving burden on the ZBI, r(216) = 0.27, p < 0.001.
Caregivers in the study indicated that 67% of the care recipients had significant problems with physical health, 61% suffered from dementia or other cognitive impairment, and 37% had mental health challenges including depression, anxiety, or other psychological disorders. On the PHQ-2, 24% of caregivers scored 3 or higher, which is the cutoff for symptoms associated with major depression.
Days per week providing care (M = 5.35, SD = 2.15, range 1 to 7) was significantly associated with greater caregiver burden (ZBI), r(216) = 0.27, 95%CI[0.13, 0.39], and anxiety symptoms (GAD7), r(216) = 0.14, 95%CI[0.004, 0.27], but not with positive affect/well-being (PAW), r(216) = − 0.11, 95%CI[− 0.24, 0.02], and with depression screener score (PHQ2), r(216) = 0.09, 95%CI[− 0.05, 0.22]. In contrast, the number of hours of care provided on those days was not significantly related to any of the four dependent variables mentioned above (r-values: − 0.10 to 0.03). As shown in Table 2, caregivers rated their current physical health as better than their mental health in the excellent, very good, and good categories.
Feasibility of MFC training
Acceptability
As shown in Table 3, post-MFC training assessments indicated that participants’ overall experience of MFC was rated as good to excellent by more than 96% of caregivers. A majority of participants were very likely (68%) or likely (26%) to recommend the program to other caregivers and 89% had a more positive view of any healthcare provider who offers MFC.
Demand
The post-intervention assessment indicated that 96% of participants would feel this intervention could be useful for other caregivers.
Implementation
Participants attended on average 2.9 (SD = 1.54) of the four sessions. Using a cutoff of three sessions, 70% of participants were classified as training completers. There was no difference in the number of sessions attended by participants for the two instructors, 3.06 vs 3.02; t(192) = 0.19, p = 0.85. At baseline, we had complete responses from 216 participants. The number of respondents decreased to 198 (91.6%) at pre-training (Time 2) and to 166 (76.9%) at post-training (Time 3).
Practicality
As shown in Table 3, post-MFC training assessments indicated that a majority of participants could use mindfulness in caregiving practices (96%), were better able to cope with caregiving challenges (91%), could improve the care to others (90%), and would take better care of themselves (92%).
Expansion
Participants indicated that the overall experience of the MFC online format was rated as good to excellent by more than 96% of caregivers.
Limited Efficacy
As discussed below, primary and secondary outcomes trended in the expected direction.
Primary Outcome
After confirming no significant change in caregiver burden from baseline (mean = 22.78, SD = 9.54) to pre-training (M = 22.71, SD = 8.94), t(215) = 0.24, p = 0.81, we observed a significant reduction of 6.27% in caregiver burden from pre- to post–MFC (M = 19.76, SD = 7.76), t(215) = 7.98, p < 0.001, g = 0.35. As described in detail in the “Supplementary Information” section, the linear mixed model 2 with random intercept and six covariates, which were correlated with the four DVs at baseline and with pre- to post-training changes in the four DVs, was found to have a better fit to the data. This LMM confirmed a significant reduction in caregiver burden at post-training and that self-reported gender (female > male) and poorer caregiver emotional health (but not age and number of days per week that caregiver provided caregiving) were significantly related to greater caregiver burden.
Secondary Outcomes
MFC was also associated with a significant decrease from pre- (M = 7.58, SD = 4.89) to post-training (M = 5.14, SD = 3.85) of 23.57% in symptoms of anxiety on the GAD-7, t(215) = 10.19, p < 0.001, g = 0.54. For depression screener scores on the PHQ-2, there was a significant decrease of 27.56% from pre- (M = 1.56, SD = 1.46) to post-training (M = 1.13, SD = 1.44), t(215) = 4.95, p < 0.001, g = 0.29. The percentage of caregivers whose PHQ-2 score indicated likely major depression decreased from pre- (18.1%) to post-MFC training (12.5%). For positive affect and well-being (PAW-9), there was a significant increase of 9.99% from pre- (M = 31.46, SD = 5.90) to post-MFC training (M = 33.97, SD = 4.92), t(215) = 8.44, p < 0.001, g = 0.45. We found that from pre- to post-MFC, reduction in caregiving burden was significantly associated with decreases in anxiety, r(216) = 0.40, p < 0.001, and depression symptoms, r(216) = 0.21, p = 0.002, as well as with significant increases in positive affect/well-being, r(216) = 0.30, p < 0.001.
Exploratory Analyses
We found that male vs. female gender, age, education, number of days providing care, and identification as White vs underrepresented racial minority were not associated with improvement in any of the four dependent variables. Also, there was no effect of relationship of caregiver (spouse/partner, daughter/son, or parent/stepparent) on reduction of burden, F(3,175) = 2.00, p = 0.138, anxiety, F(3,175) = 0.95, p = 0.388, and depression screener score, F(3,175) = 0.23, p = 0.795, as well as increases in positive affect/well-being, F(3,175) = 0.032, p = 0.969. Furthermore, the number of MFC sessions attended was not associated with pre- to post-MFC changes in anxiety symptoms, r(210) = − 0.15, p = 0.029, 95%CI [− 0.280, − 0.015], depression screener scores, r(210) = − 0.15, p = 0.033, 95%CI [0.011, 0.277], burden, r(210) = − 0.047, p = 0.50, 95%CI [0.180, − 0.089], and positive affect/well-being, r(210) = 0.071, p = 0.305, 95%CI [− 0.065, 0.204]. Prior experience with mindfulness practice (use occasionally/regularly) vs. no prior use was not associated with pre- to post-ZCP-related improvement on anxiety, depression, and burden (all t-values < 1.21, p-values > 0.22).
We found that MFC-related changes in caregiver burden, anxiety, depression, and positive affect/well-being were not associated with caregiver post-training ratings of MFC program overall experience (all p-values > 0.10). However, poorer program experience was associated with poorer post-MFC caregiver self-rated emotional (r(164) = 0.26, p < 0.001) and physical health (r(165) = 0.20, p = 0.011), and a greater percentage experiencing symptoms consistent with major depression on the PHQ-2 (r(164) = 0.18, p < 0.019). Furthermore, poorer program experience was associated with baseline greater number of days a week providing care (r(165) = 0.16, p < 0.038), and poorer caregiver emotional health (r(163) = 0.21, p < 0.008).
Discussion
This study examined the feasibility of and effects on psychological functioning of a novel 4-week online-delivered mindfulness-based family caregiver training. Results suggested adequate levels of attendance to the 4-session online training and positive training outcomes, including improvement in caregiver burden, anxiety, depression, and positive affect/well-being in this community sample of informal caregivers.
Our first research question assessed the feasibility of a brief online training for informal caregivers. Treatment completion for this caregiver training was high (70%), which was comparable to a standard 8-week MBSR (83%) (Whitebird et al., 2013), an adapted 7-week MBCT (80%) (Oken et al., 2010), and superior to an 8-week online MBI for caregivers (55%) (Tkatch et al., 2017). Post-training assessment suggested that participants positively appraised the training, including enhanced ability to cope with challenges and to improve self-care and care for others, would recommend to other caregivers, and would favor healthcare providers offering this service. As compared to a standard 8-week MBI protocol that similarly teaches participants mindful awareness, self-kindness, and compassion, MFC consists of only four, once-weekly, 2-hr sessions, for a total of 8 hr of training. Although this brief training was not tested against a control group of similar duration or a standard 8-week course, preliminary findings suggest that this novel training might be as feasible as traditional in-person MBIs for caregivers, and more feasible than an 8-week MBI delivered online. Given that family caregivers have competing responsibilities that frequently prevent in-person training, the feasibility of the MFC program appears promising.
The second research question focused on the effects of the MFC training on caregiver burden, anxiety, depression, positive affect, and well-being. Our results indicated a significant improvement on caregiver burden, anxiety, depression, positive affect, and well-being, with moderate Hedges’ g effect sizes ranging from 0.49 to 0.64. These effect sizes are comparable to the effect sizes of a standard in-person MBSR for caregivers (Whitebird et al., 2013), with reductions in depression (d = 0.66), anxiety (d = 0.59), and burden (d = 0.25). Furthermore, the results from our 4-week training were comparable to an online 8-week MBI for caregivers (Whitebird et al., 2013) which reported significant reductions in caregiver burden and anxiety. Importantly, these comparable results highlight the potential of this brief online MBI to promote wellness in caregivers that lack time and access to standard in-person care.
The relationship the participant had to their care recipient had no impact on the change in scores in the four areas of mental health measured, supporting the program’s feasibility. There was also no relationship between the impact of the training and participants’ previous mindfulness experience. This could be explained by the difference between knowing about, and even formally practicing mindfulness, and using mindfulness in caregiving activities. The MFC course teaches mindfulness practices to those who are new to it and supports all participants, regardless of mindfulness familiarity, with the integration of mindfulness into caregiving activities.
The MFC is a group training program designed to bolster the emotional resilience of caregivers. Inspired by Zen Buddhist principles, MFC introduces techniques that prepare caregivers to better respond to stressors, enhance self-efficacy, and improve caregiver well-being. MFC focuses on introducing concepts and practices of mindfulness and compassion, reappraising the caregiver role, navigating loss and life transitions, and providing a community for family and friend caregivers to share similar experiences and offer support. An accumulating body of evidence supports that MBIs develop present-moment awareness and a nonjudgmental stance, which help reduce negative emotional states, including rumination, worry, and the appraisal of stress (Zhang et al., 2021). MBIs designed for caregivers have been shown to be effective to cope with caregiver stress (Oken et al., 2010), to reduce feelings of self-isolation (Tkatch et al., 2017), to improve psychological symptoms (Li et al., 2016), and to deliver in a group format (Tkatch et al., 2017).
To ground these potential benefits in psychology theory, we refer to a mindfulness-to-meaning theoretical framework Garland et al. (2015) that posits that approaching stressful challenges with the complementary processes of appraisal, decentering, and metacognition becomes a form of meaning-focused coping by seeing challenges as an opportunity rather than a threat. This can alleviate negative emotions and also generate positive emotions during stress appraisal. A caregiver facing the burden of caregiving might see how their caregiver role is transient, have less emotional reactivity to the stress, and then could shift their perspective to cherish the time together with a loved one. However, there remains a paucity of caregiver studies that directly test the underlying mechanism by which these MBIs help caregivers. Future research will have the opportunity to advance our understanding of the putative mechanisms of change in MBIs for caregivers.
Limitations and Future Research
The focus of this study was providing mindfulness-based training for family and friend caregivers. Thus, we did not recruit other types of caregivers. Although a large majority of the community sample reported prior mindfulness experience, there was no association with pre- to post-training. It will be important to examine the effects of the MFC training for other types of professional caregivers, including hospice nurses, social workers, and geriatric nursing staff. Our study did not compare MFC to other types of caregiver training and thus we do not currently know whether the outcomes we found are distinct from or common to other types of training programs with similar or different models of therapeutic change. Future studies would benefit from implementing random assignments to different types of caregiver training programs. Furthermore, we only used a brief set of self-report questionnaires to measure only four domains of psychological functioning. Future studies might be designed to assess a wider array of psychological (e.g., emotion regulation), genetic (e.g., telomeres), hormonal (e.g., cortisol), and brain (e.g., EEG coherence) variables to enhance our understanding of MFC on other important indices of well-being. Furthermore, although we used multiple imputation to impute values for missing responses for the four dependent variables in our study, we did not use a specific threshold for the amount of missing data. Because different thresholds and methods can produce different imputation results, outcomes could vary based on how missing data is handled. Finally, this study measured the impact of the course on caregiver emotional well-being. The course is also designed to enhance caregiver self-efficacy and support a healthier response to stressors. Future research should include measurement of changes in these areas as a result of the course.
Our study provided four weekly sessions and thus we do not know if the benefits of MFC would be more robust with longer doses of training or if a shorter program would be equally beneficial. Also, participants were offered the MFC training at no cost. Thus, we do not know if payment for training might enhance motivation and engagement with MFC. Approximately 84% of participants identified as White, non-Hispanic. Future studies will need to make a stronger effort to connect with communities of color and determine if components of MFC need to be modified in a culturally informed manner. Our study only assessed caregivers at three time points. Future studies need to investigate the longer-term effects of MFC, including the sustainability and integration of skills taught in MFC over a longer follow-up period. In our study, we had two very experienced instructors with extensive experience delivering MFC. It will be important to examine how effective MFC is when taught by instructors with less experience and expertise, and when taught online versus in-person.
Data Availability
The data that support the findings of this study are openly available in OSF at https://osf.io/twz58/.
References
AARP and National Alliance for Caregiving. (2020). Caregiving in the United States 2020. American Association of Retired Person. May 2020. https://doi.org/10.26419/ppi.00103.003
Bédard, M., Molloy, D. W., Squire, L., Dubois, S., Lever, J. A., & O’Donnell, M. (2001). The Zarit Burden Interview: A new short version and screening version. The Gerontologist, 41(5), 652–657. https://doi.org/10.1037/t35628-000
Bertrand, R. M., Fredman, L., & Saczynski, J. (2006). Are all caregivers created equal? Stress in caregivers to adults with and without dementia. Journal of Aging and Health, 18(4), 534–551. https://doi.org/10.1177/0898264306289620
Bowen, D. J., Kreuter, M., Spring, B., Cofta-Woerpel, L., Linnan, L., Weiner, D., Bakken, S., Kaplan, C. P., Squiers, L., Fabrizio, C., & Fernandez, M. (2009). How we design feasibility studies. American Journal of Preventive Medicine, 36(5), 452–457. https://doi.org/10.1016/j.amepre.2009.02.002
Carruth, A. K., Tate, U. S., Moffett, B. S., & Hill, K. (1997). Reciprocity, emotional well-being, and family functioning as determinants of family satisfaction in caregivers of elderly parents. Nursing Research, 46(2), 93–100. https://doi.org/10.1097/00006199-199703000-00006
Clyburn, L. D., Stones, M. J., Hadjistavropoulos, T., & Tuokko, H. (2000). Predicting caregiver burden and depression in Alzheimer’s disease. Journals of Gerontology: Series B, 55(1), S2–S13. https://doi.org/10.1093/geronb/55.1.s2
Garland, E. L., Farb, N. A., Goldin, P. R., & Fredrickson, B. L. (2015). Mindfulness broadens awareness and builds eudaimonic meaning: A process model of mindful positive emotion regulation. Psychological Inquiry, 26(4), 293–314.
Gratão, A. C. M., Brigola, A. G., Ottaviani, A. C., Luchesi, B. M., Souza, É. N., Rossetti, E. S., de Oliveira, N. A., Terassi, M., & Pavarini, S. C. I. (2019). Brief version of Zarit Burden Interview (ZBI) for burden assessment in older caregivers. Dementia & Neuropsychologia, 13, 122–129. https://doi.org/10.1590/1980-57642018dn13-010015
Gwyther, L. P., & George, L. K. (1986). Caregivers for dementia patients: Complex determinants of well-being and burden. The Gerontologist, 26(3), 245–266. https://doi.org/10.1093/geront/26.3.245
Haley, W. E., Brown, S. L., & Levine, E. G. (1987). Family caregiver appraisals of patient behavioral disturbance in senile dementia. Clinical Gerontologist, 6(4), 25–34. https://doi.org/10.1300/j018v06n04_04
Hays, R. D., Spritzer, K. L., Thompson, W. W., & Cella, D. (2015). US general population estimate for “excellent” to “poor” self-rated health item. Journal of General Internal Medicine, 30(10), 1511–1516. https://doi.org/10.1007/s11606-015-3290-x
Jaffray, L., Bridgman, H., Stephens, M., & Skinner, T. (2016). Evaluating the effects of mindfulness-based interventions for informal palliative caregivers: A systematic literature review. Palliative Medicine, 30(2), 117–131. https://doi.org/10.1177/0269216315600331
Kang, S. Y. (2006). Predictors of emotional strain among spouse and adult child caregivers. Journal of Gerontological Social Work, 47(1–2), 107–131. https://doi.org/10.1300/j083v47n01_08
King, D. E., Matheson, E., Chirina, S., Shankar, A., & Broman-Fulks, J. (2013). The status of baby boomers’ health in the United States: The healthiest generation? JAMA Internal Medicine, 173(5), 385–386. https://doi.org/10.1001/jamainternmed.2013.2006
Kroenke, K., Spitzer, R. L., & Williams, J. B. (2003). The Patient Health Questionnaire-2: validity of a two-item depression screener. Medical Care, 1284–1292. https://doi.org/10.1097/01.mlr.0000093487.78664.3c
Kubo, A., Kurtovich, E., McGinnis, M., Aghaee, S., Altschuler, A., Quesenberry, C., Kolevska, T., & Avins, A. L. (2019). A randomized controlled trial of mHealth mindfulness intervention for cancer patients and informal cancer caregivers: A feasibility study within an integrated health care delivery system. Integrative Cancer Therapies, 18, 153473541985063. https://doi.org/10.1177/1534735419850634
Lee, S., Colditz, G. A., Berkman, L. F., & Kawachi, I. (2003). Caregiving and risk of coronary heart disease in US women: A prospective study. American Journal of Preventive Medicine, 24(2), 113–119. https://doi.org/10.1016/s0749-3797(02)00582-2
Li, G., Yuan, H., & Zhang, W. (2016). The effects of mindfulness-based stress reduction for family caregivers: Systematic review. Archives of Psychiatric Nursing, 30(2), 292–299. https://doi.org/10.1016/j.apnu.2015.08.014
Little, R. J. A. (1988). A test of missing completely at random for multivariate data with missing values. Journal of the American Statistical Association, 83, 1198–1202. https://doi.org/10.1080/01621459.1988.10478722
Marks, N. F., Lambert, J. D., Jun, H., & Song, J. (2008). Psychosocial moderators of the effects of transitioning into filial caregiving on mental and physical health. Research on Aging, 30(3), 358–389. https://doi.org/10.1177/0164027507312998
Oken, B. S., Fonareva, I., Haas, M., Wahbeh, H., Lane, J. B., Zajdel, D., & Amen, A. (2010). Pilot controlled trial of mindfulness meditation and education for dementia caregivers. The Journal of Alternative and Complementary Medicine, 16(10), 1031–1038. https://doi.org/10.1089/acm.2009.0733
Pearson, J. L., Teri, L., Wagner, A., Truax, P., & Logsdon, R. G. (1993). The relationship of problem behaviors in dementia patients to the depression and burden of caregiving spouses. American Journal of Alzheimer’s Disease Care and Related Disorders & Research, 8(1), 15–22. https://doi.org/10.1177/153331759300800104
Salsman, J. M., Victorson, D., Choi, S. W., Peterman, A. H., Heinemann, A. W., Nowinski, C., & Cella, D. (2013). Development and validation of the positive affect and well-being scale for the neurology quality of life (Neuro-QOL) measurement system. Quality of Life Research, 22(9), 2569–2580. https://doi.org/10.1007/s11136-013-0382-0
Shrank, W. H., Liberman, J. N., Fischer, M. A., Kilabuk, E., Girdish, C., Cutrona, S., Brennan, T., & Choudhry, N. K. (2011). Are caregivers adherent to their own medications? Journal of the American Pharmacists Association, 51(4), 492–498. https://doi.org/10.1331/japha.2011.10006
Song, L. Y., Biegel, D. E., & Milligan, S. E. (1997). Predictors of depressive symptomatology among lower social class caregivers of persons with chronic mental illness. Community Mental Health Journal, 33(4), 269–286. https://doi.org/10.1007/bf02189064
Spitzer, R. L., Kroenke, K., Williams, J. B., & Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166(10), 1092–1097. https://doi.org/10.1001/archinte.166.10.1092
Stones, M., Ghent-Fuller, J., Bell, M., Malott, O., Clyburn, L., Stones, L., & Kalopack, P. (1997). Alzheimer disease and aggression: A guide for caregivers. Captus Press.
Tkatch, R., Bazarko, D., Musich, S., Wu, L., MacLeod, S., Keown, K., Hawkins, K., & Wicker, E. (2017). A pilot online mindfulness intervention to decrease caregiver burden and improve psychological well-being. Journal of Evidence-Based Complementary & Alternative Medicine, 22(4), 736–743. https://doi.org/10.1177/2156587217737204
Whitebird, R. R., Kreitzer, M., Crain, A. L., Lewis, B. A., Hanson, L. R., & Enstad, C. J. (2013). Mindfulness-based stress reduction for family caregivers: A randomized controlled trial. The Gerontologist, 53(4), 676–686. https://doi.org/10.1093/geront/gns126
Zarit, S. H., Reever, K. E., & Bach-Peterson, J. (1980). Relatives of the impaired elderly: correlates of feelings of burden. The gerontologist, 20(6), 649–655.
Zarit, S. H., & Whitlatch, C. J. (1992). Institutional placement: Phases of the transition. The Gerontologist, 32(5), 665–672. https://doi.org/10.1093/geront/32.5.665
Zhang, D., Lee, E. K., Mak, E. C., Ho, C. Y., & Wong, S. Y. (2021). Mindfulness-based interventions: An overall review. British Medical Bulletin, 138(1), 41–57. https://doi.org/10.1093/bmb/ldab005
Funding
Funding for this work by the Stupski Foundation is gratefully acknowledged. None of the four authors work for the Stupski Foundation. MJ does not have any financial relationship with the Stupski Foundation. NS worked for the Zen Caregiving Program and did not receive any salary from the Stupski Foundation. PG and JB are professors at the University of California Davis. They each received a small fee for consultation on the design, implementation, and statistical analysis.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, analysis, and the first draft were performed by all authors. All authors read and approved the final manuscript. Michael Juberg: conceptualization, methodology, project administration, writing—review and editing. Naomi Stoll: funding acquisition, conceptualization, project administration, writing—review and editing. Philippe Goldin: conceptualization, methodology, supervision, formal analysis, project administration, writing—review and editing. Janice Bell: conceptualization, methodology, supervision, project administration, writing—review and editing.
Corresponding author
Ethics declarations
Ethics Approval
Approval was obtained from the ethics committee of the University of California Davis. The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Informed Consent
All persons gave their informed consent prior to their inclusion in the study.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Juberg, M., Stoll, N., Goldin, P. et al. Investigating the Feasibility and Effects of an Online Mindfulness Family Caregiver Training Program. Mindfulness 14, 1531–1541 (2023). https://doi.org/10.1007/s12671-023-02126-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12671-023-02126-3