Abstract
Objectives
Anxiety and depression are common in chronic physical illness populations. Self-compassion, the motivation and the capacity to alleviate one’s own suffering, is associated with reduced anxiety and depression in mental health populations. This review aimed to collate available research showing links between self-compassion and anxiety and depression in chronic physical illness populations.
Methods
This study is a systematic review of English language studies investigating univariate and multivariate correlates of anxiety and depression by self-compassion constructs in adult chronic physical illness populations.
Results
Twenty papers, reporting data from 16 unique studies, were included. Half sampled cancer patients. Self-compassion scores consistently showed moderate to large inverse associations with anxiety and depression over both univariate (r = −.37 to −.53 and r = −.38 to −.66, respectively) and multivariate analyses (β =.01 to β = −.55 and β = −.17 to β = −.59, respectively). Worry and depressive brooding, and shame, mediated relationships between self-compassion and anxiety and depression.
Conclusions
Although findings suggest that self-compassion processes may have a role in alleviating anxiety and depression in chronic physical illness populations, methodological limitations limit confidence in this proposition. Prospective studies that identify theoretically plausible mediators and moderators are required before the development or modification of therapeutic interventions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Chronic physical illnesses are longstanding health conditions that require adaptation by those experiencing them (Bernell and Howard 2016). It is estimated that 30% of people live with one or more chronic physical illnesses (Department of Health 2008). Coping with chronic physical illness is often challenging, requiring adaption to pain, functional limitations, social changes and the fear of deterioration or illness progression (Department of Health 2008; Turner and Kelly 2000). Consequently, patients with chronic physical illness have higher rates of anxiety compared to age- and gender-matched counterparts (Clarke and Currie 2009) and are two to three times more likely to experience clinical depression than the general population (National Institute for Health and Care Excellence 2009). The lifetime prevalence of depression in those with multiple chronic physical illnesses is sevenfold compared to those who have none (Moussavi et al. 2007).
In turn, anxiety and depression are associated with physical illness progression in obstructive pulmonary disease (Ng et al. 2007), asthma (Walters et al. 2011), cardiovascular illness (Jünger et al. 2005; Katon 2003) and diabetes (Katon et al. 2004). Illness deterioration is possibly attributable to poorer self-management (DiMatteo et al. 2000; Felker et al. 2010) and treatment adherence (DiMatteo et al. 2000). Treating symptoms of anxiety and depression in people with chronic physical illness thus may both reduce psychological distress and improve general physical health.
The cognitive behavioural therapy (CBT) is a recommended treatment for anxiety and depression in adults with chronic physical illnesses (National Institute for Health and Care Excellence 2009, 2011). Studies demonstrate the effectiveness of CBT for anxiety and depression in patients with heart failure (Jeyanantham et al. 2017), diabetes (Zhi-da Wang et al. 2017), cancer (Xiao et al. 2017) and across mixed samples (Farrand and Woodford 2015). However, effect sizes have been modest at best and, in some cases, concerningly small (Noble et al. 2018; Temple et al. 2020). One plausible reason may be that a focus of CBT is to challenge the validity of negative thoughts about illness, which are seen to perpetuate distress. However, in the case of chronic physical illness, appraisals of illness-related adversity may be objective and, thus, less amendable to change using traditional CBT interventions (Cherry et al. 2019; Herschbach and Dinkel 2014; Humphris and Ozakinci 2008).
Process-focused CBT approaches aim to reduce the problem of objective adversity by focussing on the process rather than the content of cognition. In other words, they address cross-situational individual differences that are held to inhibit successful coping with immutable challenges (Normann et al. 2014). Compassion-based approaches are based on the premise that excessive self-criticism and self-blame cause anxiety, depression and other forms of psychopathology (Gilbert 2017; Neff 2003b). Self-compassion is a skilled response that allows coping with immutable adversity—not by challenging perceptions of adversity or facilitating fruitless efforts to overcome it—but by inhibiting self-blame and self-criticism through compassionate acceptance of both self and reality (Kirschner et al. 2019; Rockliff et al. 2011). Compassion-based interventions may therefore be particularly suited to the needs of chronic physical illness patients, who often live with realistic and immutable challenges and difficulties associated with their illness (Turner and Kelly 2000).
A range of therapeutic and self-help interventions aim to reduce emotional distress by cultivating self-compassion. Despite some commonalities in treatment approaches, compassion-based interventions vary in their therapeutic underpinnings, length, format, conceptualisation of self-compassion and clinical focus. The compassion-focused therapy (CFT), underpinned by social mentality theory (Gilbert 2017), is a widely used approach developed for clinically significant emotional distress. CFT aims to help patients to develop self-compassion through supervised practice of structured therapeutic exercises, including visualisation and breathing exercises, which are collectively referred to as ‘compassionate mind training’ (Gilbert 2009). Mindful self-compassion (MSC) is a less-intensive manualised, skills-based, 8-week group intervention, applicable to the general population and to some clinical populations. MSC is based on Neff’s (2003a, b, 2016) operationalisation of self-compassion as self-kindness (taking a gentle, warm and understanding approach towards oneself whilst accepting that difficulties are inevitable parts of life), mindfulness (an equilibrated stance to thoughts where individuals do not over-identify with thoughts, nor do they supress them) and common humanity (contextualising personal difficulties within a wider framework of shared human experience). MSC is designed primarily to help individuals to develop self-compassion, with mindfulness as a secondary emphasis, and combines psycho-education with interpersonal exercises, formal and informal mindfulness practice and meditation. Alternative programmes include compassion cultivation training (CCT; Jazaieri et al. 2012), an 8-week course for clinical and non-clinical populations designed to cultivate compassion, empathy and kindness towards all, and mindfulness-based compassionate living (MBCL; Van den Brink and Koster 2015), a sequential treatment designed explicitly to cultivate compassion in adults who have previously participated in mindfulness-based cognitive therapy (MBCT).
Therapeutic interventions that focus on cultivating self-compassion and its components have largely been evaluated in mental health samples. Interventions have been found to reduce shame and depression (Braehler et al. 2013; Judge et al. 2012; Lucre and Corten 2013; Schuling et al. 2020), although evidence from randomised controlled trials (RCTs) is currently limited (Leaviss and Uttley 2015). Two recent systematic reviews provide preliminary evidence that compassion-based interventions may reduce anxiety and depression in chronic physical illness patients (Austin et al. 2020; Kılıç et al. 2020). A mixture of qualitative, pre-post and small-sample randomised controlled trials suggest that brief and intensive interventions, drawing from a range of theoretical approaches, improve self-compassion, anxiety and depression in clinical and non-clinical populations (Austin et al. 2020; Kılıç et al. 2020) and are generally acceptable to patients (Austin et al. 2020).
Interventions for both mental and physical health samples must be underpinned by theoretically based investigations of links between self-compassion and anxiety and depression (MacBeth and Gumley 2012). In addition to simple correlations between self-compassion and anxiety and depression, it is theoretically and practically important to identify variability between differing populations and uncover moderating and mediating variables. In the mental health literature, reviews have found inverse relationships between self-compassion and anxiety and depression in adult (MacBeth and Gumley 2012) and adolescent (Marsh et al. 2018) samples. Although several studies have examined links between self-compassion and psychological distress in chronic physical illness populations, there are, as yet, no integrative analyses that provide an overview of this evidence. This systematic review therefore aims to address this need through the following review questions: (1) What is the strength and direction of any associations between self-compassion and anxiety and depression in chronic physical health populations? (2) What, if any, factors mediate or moderate these relationships?
Method
The conduct and reporting of the review are in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist (Liberati et al. 2009; Moher et al. 2009). A review protocol can be found at https://www.crd.york.ac.uk/PROSPERO (CRD42017079961).
Search Strategy
Four electronic databases (PsycINFO, MEDLINE, Web of Science and CINAHL Plus) were searched for relevant published literature from their inception until December 2017 using the following search terms: (self-compassion or self-kindness or compassion-focused or compassion*) and (anxiety or depression or psychopathology or distress or anxious or psychological functioning or Stress, psychological/ or Adaptation, psychological/). Search syntax was developed and finalised in MEDLINE and adapted for each electronic database. To ensure a comprehensive search for chronic physical illnesses and reduce the risk of overlooking potentially relevant papers, we did not search using specific terms for chronic physical illnesses but rather identified relevant papers via title/abstract and full-text screening. The reference lists of included papers and relevant review articles were subsequently hand-searched for additional studies. Searches were repeated in February 2020 to identify any new relevant publications.
Study Selection
Following de-duplication, titles and abstracts of identified citations were screened against the eligibility criteria, followed by the full text of potentially eligible studies. At both stages, studies which did not meet the inclusion criteria were excluded. Screening was completed independently by MH and SD; consensus was reached through discussion, with MGC and SB consulted where necessary. Studies were included if they (i) reported data from participants aged ≥ 18 years old with one or more diagnosed chronic illness(es); (ii) reported quantitative data regarding the association between self-compassion and anxiety and/or depression; and (iii) were written, or available, in English. With regard to criterion ii, studies were required to measure self-compassion and depression and/or anxiety using scales or subscales that had been publicly referenced for reliability and/or validity (minor adaptations of the scales were acceptable providing the authors’ objective was to measure the same construct). Studies using the two-factor structure of the Self-Compassion Scale were excluded, in line with Neff et al. (2019), who concluded that the constituent elements of self-compassion operate in tandem and therefore should be interpreted as an overall score. Studies reporting samples of people with neurological or developmental conditions were also excluded, because these diagnoses may result in additional challenges for patients, including differing functional, learning and communication needs.
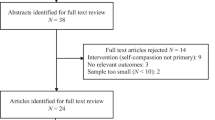
The initial search retrieved 4794 studies, resulting in 2462 unique citations after de-duplication and removal of non-peer-reviewed journal articles. In total, 2278 articles were eliminated after screening abstracts and titles. After screening the full text of the remaining 184 articles, 12 papers, reporting data from 10 studies, were deemed eligible for inclusion. A further 8 papers were included following the updated search, resulting in the inclusion of 20 papers, reporting data from 16 studies. The study selection process is summarised in Fig. 1.
Risk of Bias
Risk of bias was assessed across eight domains using an adapted tool from the Agency for Healthcare Research and Quality (Williams et al. 2010). We defined adequate sampling as a consecutive sample, or an attempt to recruit a representative sample from a defined population of patients (e.g. eligible patients currently under care by a health service), and inadequate sampling as purposive samples that did not attempt to represent the patient population. An adequate characterisation of the sample consisted of patient age, gender, time since diagnosis, whether diagnosed by trained professionals or self-identified, summary of past and current treatment and comorbidities. Adequate control variables were age and gender (where samples contained both genders). Assessment of risk of bias was not intended to exclude studies but to better interpret study findings.
Data Extraction and Analysis
Relevant demographic, clinical and outcome data were extracted by MH and checked for accuracy by SD using a standardised and piloted data extraction form. Discrepancies were resolved through discussion, with the views of MGC and SB sought where necessary. Authors were contacted regarding missing or unclear data. Where studies reported multiple analyses, only data from (i) univariate analyses reporting associations between self-compassion and anxiety and/or depression and (ii) multivariate analyses in which the effects of demographic and clinical characteristics were controlled for were extracted. Intervention studies were included only if they reported univariate or multivariate analyses of variables of interest pre-intervention; post-intervention data and retrospective data were excluded. Where studies reported linked data, data from the largest sample were reported, with linked studies listed. Data were tabulated, summarised and analysed narratively.
Results
Study Characteristics
The main characteristics of the 16 included studies are detailed in Table 1. Studies were conducted in eight countries with one multinational setting. Fifteen studies were cross-sectional. Studies reported data from a total of 6038 participants, with mean ages ranging from the lowest of 43.50 years to the highest of 70.84 years. Older patients were found in COPD (Harrison et al. 2017) and lung cancer (Schellekens et al. 2017) samples. Younger patients were found in papers derived from the two HIV datasets (Eller et al. 2014; Kemppainen et al. 2013a, b; Skinta et al. 2019; Williams et al. 2019).
Studies focused on a range of physical health conditions (Table 1). Five studies used breast cancer samples (Brown et al. 2020; Przezdziecki and Sherman 2016; Przezdziecki et al. 2013; Sherman et al. 2017; Todorov et al. 2019), three non-breast cancers (Gillanders et al. 2015; Schellekens et al. 2017; Zhu et al. 2019), three diabetes (Friis et al. 2015; Morrison et al. 2019; Ventura et al. 2019) and two HIV (Eller et al. 2014; Kemppainen et al. 2013a, b; Skinta et al. 2019; Williams et al. 2019; Zhu et al. 2019). Eleven studies (Eller et al. 2014; Kemppainen et al. 2013a, b; Friis et al. 2015; Gillanders et al. 2015; Harrison et al. 2017; Morrison et al. 2019; Przezdziecki et al. 2013; Schellekens et al. 2017; Sherman et al. 2017; Skinta et al. 2019; Williams et al. 2019; Ventura et al. 2019; Zhu et al. 2019) reported time since diagnosis, which ranged from less than 1 week to an average of 16.70 years. Samples were generally female only or predominantly female, with the exception of the two HIV studies (Eller et al. 2014; Kemppainen et al. 2013a, b; Skinta et al. 2019; Williams et al. 2019). Only one study used a prospective design (Zhu et al. 2019). The remainder of studies were cross-sectional which means that it was not possible to assign a temporal direction to correlations (e.g. that self-compassion precedes the development of anxiety or depression).
Assessment of Self-Compassion, Anxiety and Depression
As shown in Table 2, all studies used the Self-Compassion Scale (Neff 2003a). Eight (Brown et al. 2020; Costa and Pinto-Gouveia 2011, 2013; Edwards et al. 2019; Friis et al. 2015; Gillanders et al. 2015; Morrison et al. 2019; Przezdziecki et al. 2013; Przezdziecki and Sherman 2016) used the original 26-item version of this scale and eight (Eller et al. 2014; Kemppainen et al. 2013a, b; Harrison et al. 2017; Schellekens et al. 2017; Sherman et al. 2017; Skinta et al. 2019; Williams et al. 2019; Ventura et al. 2019; Zhu et al. 2019) the 12-item short form scale developed by Raes et al. (2011). All studies used total self-compassion scores, except one that analysed only subscale means for self-kindness, mindfulness and common humanity (Brown et al. 2020). The most commonly used measures of depression and/or anxiety were the Depression Anxiety Stress Scale (DASS; n = 5; Henry and Crawford 2005; Lovibond and Lovibond 1995), the Hospital Anxiety and Depression Scale (HADS; n = 4; Zigmond and Snaith 1983) and the Patient Health Questionnaire (PHQ; n = 4; Kroenke et al. 2001; Kroenke et al. 2009).
Risk of Bias Assessment
The results of the risk of bias assessment are in Table 3. Most studies showed some risk of bias. Only five used adequate sampling frames, and clinical and demographic details were often not fully characterised. Studies commonly did not include sample size calculations or report on the amount or importance of missing data. Measures used and analytic techniques were appropriate for the studies’ aims, although it is noteworthy that all studies used the Self-Compassion Scale (Neff 2003a) to assess self-compassion.
Univariate Analyses
The main findings for included studies are depicted in Table 2. Ten of the 16 studies used univariate analyses to examine associations between self-compassion and anxiety. All showed significant negative correlations, with r values ranging from − .37 to − .53. For subscale scores, Brown et al. (2020) found small to large effect sizes (r = − .27 to r = − .48) for self-kindness, mindfulness and common humanity. Twelve studies examined associations between self-compassion and depression. All showed significant negative associations, with r values ranging from − .38 to − .66. Brown et al. (2020) found medium to large effect sizes (r = − .38 to r = − .54) for subscales. One study examined associations between total distress (as measured by HADS total score) and self-compassion and found a significant negative association (r = − .55). Univariate correlations were remarkably stable across studies, occurring in a narrow band from − .37 to − .66, with little variance between differing chronic illness populations. Further, the one study that compared differing nationalities (Kemppainen et al. 2013a, b) found little divergence in correlations across Canadian, Chinese, Namibian, Puerto Rican and US populations (r = − .36 to − .44).
Multivariate Analyses
Six studies used multivariate analyses. As shown in Table 2, age, gender and illness duration were most frequently controlled, whilst two studies controlled coping styles (Costa and Pinto-Gouveia 2011, 2013; Gillanders et al. 2015). After controlling for potential covariates, five of these studies (Costa and Pinto-Gouveia 2011, 2013; Eller et al. 2014; Kemppainen et al. 2013a, b; Todorov et al. 2019; Ventura et al. 2019; Zhu et al. 2019) found significant, inverse associations between self-compassion and anxiety, with values ranging from β = −.21 to β = −.53. Six studies examined the relationship between depression and self-compassion using multivariate analyses. Of these, five studies (Costa and Pinto-Gouveia 2011, 2013; Friis et al. 2015; Todorov et al. 2019; Ventura et al. 2019; Zhu et al. 2019) found significant, inverse associations between self-compassion and depression after controlling for a range of covariates, with values ranging from β = −.35 to β = −.59.
Mediation and Moderation Analyses
Two papers used path analysis to identify mediators (Brown et al. 2020; Skinta et al. 2019), whilst one considered moderation (Schellekens et al. 2017). Brown et al. (2020) found worry and depressive brooding to mediate relationships between self-kindness and mindfulness and anxiety and depression, whilst Skinta et al. (2019) found shame to mediate the relationship between self-compassion and depression. Schellekens et al. (2017) showed that self-compassion was less strongly associated with the full-scale score of the HADS in lung cancer patients if they had a partner who scored more highly on self-compassion, suggesting that higher partner self-compassion might attenuate distress in lower self-compassion scorers.
Discussion
This systematic review identified the strengths and directions of univariate and multivariate relationships between self-compassion and anxiety and depression in individuals with chronic physical illnesses. We observed consistently similar univariate and multivariate inverse associations between self-compassion and both anxiety and depression, across a broad range of chronic health conditions. Mediators were worry and depressive brooding, and shame; moderators were partner self-compassion. Findings align with previous reviews showing that self-compassion is inversely associated with distress across a range of mental health populations (MacBeth and Gumley 2012; Marsh et al. 2018) and extends this evidence base to chronic physical health populations (Pinto-Gouveia et al. 2014).
The consistency of the associations between self-compassion and anxiety and depression in this review and their similarities with reviews of mental health literature (MacBeth and Gumley 2012; Marsh et al. 2018) provides some evidence of uniformity across illness populations. Further, one study provided evidence of cultural invariance through consistency across differing national populations. The two mediational studies showed that worry, depressive brooding and shame may mediate any effects of self-compassion on depression and anxiety. These are consistent with self-compassion theory, but more mediational work is required. In the clearest theoretical description, Gilbert (2009) viewed emotional regulation as activations or suppressions of specific mentalities and cognitive-motivational capacities and dispositions for specific behavioural responses, underpinned by discrete neurobiological subsystems. Optimal human functioning is a balance between a resting subsystem underpinning affiliative social mentalities, a drive system underpinning goal pursuit and a threat system facilitating aggressive responding. Threat and drive systems are characterised by focus on goals, threats or obstacles and facilitate problem-solving, self-improvement and persistence (Gilbert 2017). These are associated with sympathetic and adrenal arousal. Where problems are immutable and direct actions ineffective, as with chronic physical illness (Sprangers and Schwartz 2000), threat focus may lead to perseverance, self-criticism and shame (Gilbert 2017). The resting system allows detachment from individualistic striving and is characterised by affiliative and compassionate mentalities (Gilbert 2017). Linked to parasympathetic arousal, the resting system supports collective social functioning and is inimical to threat arousal (Kirschner et al. 2019; Rockliff et al. 2011). A self-compassion approach activates the resting system, thus defusing self-criticism (Broom and Whittacker 2004) and self-blame (Friedman et al. 2007).
Gilbert’s (2009, 2017) theory provides testable mediational hypotheses focussing on physiological and psychological variables that could form a basis for future research. The theory also provides an explicit mechanism whereby self-compassion-based interventions could help people cope with immutable physical illness. These interventions acknowledge the reality of patients’ experiences of illness, but aim to develop compassion-based skillsets that overlay and inhibit threat and drive responses in contexts where they may be harmful. Early indications suggest that self-compassion-based interventions might be efficacious (Austin et al. 2020; Kılıç et al. 2020).
Importantly, studies in this review recruited patients with a spectrum of anxiety and depression scores. Associations between self-compassion and anxiety and depression were largely linear (or detectable using linear tests of association). If links were causal, this would imply that increases in self-compassion from either lower or higher baselines might change anxiety and depression to a similar degree. Thus, most patients might benefit to some degree from self-compassion-focussed intervention. Preliminary evidence suggests that ‘comprehensive’ compassion- based interventions, such as CFT, MSC, CCT and MBCL, are effective interventions for depression and anxiety experienced by adults with chronic physical illness, regardless of the severity of these difficulties (Austin et al. 2020; Kılıç et al. 2020). Thus, a range of interventions varying in intensity, from self-help approaches (e.g. MSC) to structured therapies (e.g. CFT), could be offered to patients depending on their needs and wishes. Preliminary evidence indicates that these interventions also effectively target process outcomes by increasing self-compassion and reducing self-blame and criticism (Austin et al. 2020; Kılıç et al. 2020). However, large-scale mediational RCTs are needed to definitively establish any effects and mechanisms of these interventions for adults with chronic physical illness (Austin et al. 2020).
Limitations and Future Research
The studies that we reviewed had limitations. The cross-sectional nature of included studies means that causality cannot be inferred. Reverse causality is possible, where depression and anxiety cause reduced self-compassion. If so, self-compassion-based interventions may not be the most efficacious treatments for depression and anxiety. We do, however, note some small-scale RCT studies of self-compassion-based interventions, suggesting that relationships may be causal (Austin et al. 2020; Kılıç et al. 2020). In cross-sectional studies, it is not possible to rule out common method effects due to overlap of self-compassion items and distress measures and scale scoring formats. In particular, it has been argued that isolation and self-criticism subscales overlap with distress items, thus inflating correlations (Muris and Petrocchi 2017). We strongly recommend more prospective studies.
Concern has been raised over the instrument used in all studies—the Self-Compassion Scale—as three of the six subscales, self-judgement, isolation and over-identification, represent pathological states rather than inverse measures of compassion (Muris and Petrocchi 2017). However, where positive compassion scores (self-kindness, mindfulness and common humanity; Brown et al. 2020; Zhu et al. 2019) were analysed, we noted that findings were similar to full Self-Compassion Scale scores in other studies. A broader concern is that the Self-Compassion Scale represents a single theoretical perspective. Arguably, Gilbert’s (2017) social mentality theory provides the most detailed theoretical account of compassion and self-compassion, but the measure attuned to this account (Gilbert et al. 2017) has only recently been published and was not used in the studies in this review. Similarly, the basis for advocating CFT is weakened also because it is not attuned to the Self-Compassion Scale.
This review also has limitations. PRISMA guidelines focused on the reporting of data, aiding future replication of the review. With no rigorous or gold standard process for conducting grey literature searches (Bellefontaine and Lee 2014), the review was limited to the inclusion of published literature to further support replication. Publication bias is therefore acknowledged as a limitation (Benzies et al. 2016). Further, studies written in languages other than English were not included in this review. Language bias is therefore also acknowledged.
The outcome of this review is qualified support for an association between self-compassion and both anxiety and depression in adults with chronic physical illness. These data support the utility of a compassion-based approach to treating anxiety and depression experienced by adults with chronic physical illness (Austin et al. 2020; Kılıç et al. 2020). Three lines of evidence are needed to inform refinement of compassion-based approaches for this patient population, as identified by Austin et al. (2020). First, prospective studies are needed. Second, evidence is needed that a self-compassion-based approach either explains unique aspects of anxiety and depression in chronic physical illness or does so better than competing perspectives. Specifically, a self-compassion-based approach will need to be shown to be empirically independent of, or a better predictor than, acceptance and commitment (Hayes et al. 2016) or metacognitive (Wells 2009) approaches. A third objective in terms of theory testing is to better understand mediational (Brown et al. 2020) and moderating (Abdollahi et al. 2020) pathways by which self-compassion might influence anxiety and depression. These data would allow for greater confidence in a causal relationship between self-compassion and depression and anxiety in chronic physical illness and inform intervention development and evaluation.
Compassion, as envisaged by Gilbert et al. (2017), is an inherently social process (Sherman et al. 2017); thus, it may be important to think beyond the individual or group interventions discussed in this review. As such, findings also have clinical relevance for frontline staff such as nurses, surgeons, etc., who see patients for consultation along the disease trajectory, and more broadly in health service policy (Lilliehorn et al. 2010). In other words, clinicians may need to think more broadly about the clinical context and how practitioners use compassion and sensitively guide patients towards more positive, encouraging and forgiving self-talk (Allen and Leary 2010).
This systematic review examined the association between self-compassion and anxiety and depression in adults with chronic physical illnesses. Findings suggest higher levels of self-compassion are associated with lower levels of anxiety and depression. Further investigation of the theory underpinning self-compassion, using prospective designs with multivariate analyses, could increase the clinical utility of this model, complementing more traditional CBT approaches for treating psychological distress in these populations.
References
References marked with an * indicate studies included in this systematic review.
Abdollahi, A., Taheri, A., & Allen, K. A. (2020). Self-compassion moderates the perceived stress and self-care behaviours link in women with breast cancer. Psycho-oncology, 29, 927–933. https://doi.org/10.1002/pon.5369.
Allen, A. B., & Leary, M. R. (2010). Self-compassion, stress, and coping. Social and Personality Psychology Compass, 4(2), 107–118. https://doi.org/10.1111/j.1751-9004.2009.00246.x.
Austin, J., Drossaert, C., Schroevers, M., Sanderman, R., Kirby, J., & Bohlmeijer, E. (2020). Compassion-based interventions for people with long-term physical conditions: A mixed methods systematic review. Psychology & Health, 36(1), 16–42. https://doi.org/10.1080/08870446.2019.1699090.
Bellefontaine, S. P., & Lee, C. M. (2014). Between black and white: Examining grey literature in meta-analyses of psychological research. Journal of Child and Family Studies, 23(8), 1378–1388. https://doi.org/10.1007/s10826-013-9795-1.
Benzies, K. M., Premji, S., Hayden, K. A., & Serrett, K. (2016). State of the evidence reviews: Advantages and challenges of including grey literature. Worldviews on Evidence-Based Nursing, 3(2), 55–61. https://doi.org/10.1111/j.1741-6787.2006.00051.x.
Bernell, S., & Howard, S. (2016). Use your words carefully: What is a chronic disease? Frontiers in Public Health, 4, 159. https://doi.org/10.3389/fpubh.2016.00159.
Braehler, C., Gumley, A., Harper, J., Wallace, S., Norrie, J., & Gilbert, P. (2013). Exploring change processes in compassion focused therapy in psychosis: Results of a feasibility randomized controlled trial. British Journal of Clinical Psychology, 52(2), 199–241. https://doi.org/10.1111/bjc.12009.
Broom, D., & Whittacker, A. (2004). Controlling diabetes, controlling diabetics: Moral language in the management of diabetes type 2. Social Science & Medicine, 58(11), 2371–2382. https://doi.org/10.1016/j.socscimed.2003.09.002.
*Brown, S. L., Hughes, M., Campbell, S., & Cherry, M. G. (2020). Could worry and rumination mediate relationships between self-compassion and psychological distress in breast cancer survivors? Clinical Psychology and Psychotherapy, 27(1), 1-10. https://doi.org/10.1002/cpp.2399.
Cherry, M. G., Salmon, P., Byrne, A., Ullmer, H., Abbey, G., & Fisher, P. (2019). Qualitative evaluation of cancer survivors’ experiences of metacognitive therapy: A new perspective on psychotherapy in cancer care. Frontiers in Psychology, 10. https://doi.org/10.3389/fpsyg.2019.00949.
Clarke, D. M., & Currie, K. C. (2009). Depression, anxiety and their relationship with chronic diseases: A review of the epidemiology, risk and treatment evidence. The Medical Journal of Australia, 190(7), 54–60. https://doi.org/10.5694/j.1326-5377.2009.tb02471.x.
*Costa, J., & Pinto-Gouveia, J. (2011). Acceptance of pain, self-compassion and psychopathology: Using the chronic pain acceptance questionnaire to identify patients' subgroups. Clinical Psychology and Psychotherapy, 18(4), 292-302. https://doi.org/10.1002/cpp.718.
*Costa, J., & Pinto-Gouveia, J. (2013). Experiential avoidance and self-compassion in chronic pain. Journal of Applied Social Psychology, 43(8), 1578-1591. https://doi.org/10.1111/jasp.12107
Department of Health. (2008). Ten things you need to know about long term conditions. http://webarchive.nationalarchives.gov.uk/+/http://www.dh.gov.uk/en/Healthcare/Longtermconditions/DH_084294
DiMatteo, M., Lepper, H., & Croghan, T. (2000). Depression is a risk factor for noncompliance with medical treatment: Meta-analysis of the effects of anxiety and depression on patient adherence. Archives of Internal Medicine, 160(14), 2101–2107. https://doi.org/10.1001/archinte.160.14.2101.
*Edwards, K. A., Pielech, M., Hickman, J., Ashworth, J., Sowden, G., & Vowles, K. E. (2019). The relation of self-compassion to functioning among adults with chronic pain. European Journal of Pain, 23(8), 1538-1547. https://doi.org/10.1002/ejp.1429.
*Eller, L. S., Rivero-Mendez, M., Voss, J., Chen, W. T., Chaiphibalsarisdi, P., Iipinge, S., & Tyer-Viola, L. (2014). Depressive symptoms, self-esteem, HIV symptom management self-efficacy and self-compassion in people living with HIV. AIDS Care, 26(7), 795-803. https://doi.org/10.1080/09540121.2013.841842
Farrand, P., & Woodford, J. (2015). Effectiveness of cognitive behavioural self-help for the treatment of depression and anxiety in people with long-term physical health conditions: A systematic review and meta-analysis of randomised controlled trials. Annals of Behavioral Medicine, 49(4), 579–593. https://doi.org/10.1007/s12160-015-9689-0.
Felker, B., Bush, K. R., Harel, O., Shofer, J. B., Shores, M. M., & Au, D. H. (2010). Added burden of mental disorders on health status among patients with chronic obstructive pulmonary disease. Primary Care Companion to the Journal of Clinical Psychiatry, 12(4), 1–8. https://doi.org/10.4088/PCC.09m00858gry.
Friedman, L. C., Romero, C., Elledge, R., Chang, J., Kalidas, M., Dulay, M. F., Lynch, G. R., & Osborne, C. K. (2007). Attribution of blame, self-forgiving attitude and psychological adjustment in women with breast cancer. Journal of Behavioral Medicine, 30(4), 351–357. https://doi.org/10.1007/s10865-007-9108-5.
*Friis, A. M., Johnson, M. H., Cutfield, R. G., & Consedine, N. S. (2015). Does kindness matter? Self-compassion buffers the negative impact of diabetes-distress on HbA1c. Diabetic Medicine, 32(12), 1634-1640. https://doi.org/10.1111/dme.12774
Gilbert, P. (2009). Introducing compassion-focused therapy. Advances in Psychiatric Treatment, 15, 199–208. https://doi.org/10.1192/apt.bp.107.005264.
Gilbert, P. (2017). A brief outline of the evolutionary approach for compassion-focussed therapy. EC Psychology and Psychiatry, 3, 218–227.
Gilbert, P., Catarino, F., Duarte, C., Matos, M., Kolts, R., Stubbs, J., Ceresatto, L., Duarte, J., Pinto-Gouveia, J., & Basran, J. (2017). The development of compassionate engagement and action scales for self and others. Journal of Compassionate Health Care, 4(4). https://doi.org/10.1186/s40639-017-0033-3.
*Gillanders, D., Sinclair, A., MacLean, M., & Jardine, K. (2015). Illness cognitions, cognitive fusion, avoidance and self-compassion as predictors of distress and quality of life in a heterogeneous sample of adults, after cancer. Journal of Contextual Behavioral Science, 4, 300-311. https://doi.org/10.1016/j.jcbs.2015.07.003.
*Harrison, S. L., Robertson, N., Goldstein, R. S., & Brooks, D. (2017). Exploring self-conscious emotions in individuals with chronic obstructive pulmonary disease: A mixed-methods study. Chronic Respiratory Disease, 14(1), 22-32. https://doi.org/10.1177/1479972316654284
Hayes, S. C., Luoma, J. B., Bond, F. W., Masuda, A., & Lillis, J. (2016). Acceptance and commitment therapy, relational frame theory, and the third wave of behavioral and cognitive therapies. Behavior Therapy, 47(6), 869–885. https://doi.org/10.1016/j.beth.2016.11.006.
Henry, J. D., & Crawford, J. R. (2005). The 21-item version of the Depression Anxiety Stress Scales (DASS–21): Normative data and psychometric evaluation in a large non-clinical sample. British Journal of Clinical Psychology, 44(22), 227–239. https://doi.org/10.1348/014466505X29657.
Herschbach, P., & Dinkel, A. (2014). Fear of progression. In U. Goerling & A. Mehnert (Eds.), Psycho-oncology: recent results in cancer research (pp. 13–33). Berlin: Springer.
Humphris, G., & Ozakinci, G. (2008). The AFTER intervention: A structured psychological approach to reduce fears of recurrence in patients with head and neck cancer. British Journal of Health Psychology, 13(2), 223–230. https://doi.org/10.1348/135910708X283751.
Jazaieri, H., Jinpa, G., McGonigal, K., Rosenberg, E., Finkelstein, J., Simon-Thomas, E., Cullen, M., Doty, J. R., Gross, J. J., & Goldin, P. (2012). Enhancing compassion: a randomized controlled trial of a compassion cultivation training programme. Journal of Happiness Studies, 14, 1113–1126. https://doi.org/10.1007/s10902-012-9373-z.
Jeyanantham, K., Kotecha, D., Thanki, D., Dekker, R., & Lane, D. A. (2017). Effects of cognitive behavioural therapy for depression in heart failure patients: A systematic review and meta-analysis. Heart Failure Reviews, 22(6), 731–741. https://doi.org/10.1007/s10741-017-9640-5.
Judge, L., Cleghorn, A., McEwan, K., & Gilbert, P. (2012). An exploration of group-based compassion focused therapy for a heterogeneous range of clients presenting to a community mental health team. International Journal of Cognitive Therapy, 5(4), 420–429. https://doi.org/10.1521/ijct.2012.5.4.420.
Jünger, J., Schellberg, D., Müller-Tasch, T., Raupp, G., Zugck, C., Haunstetter, A., & Haass, M. (2005). Depression increasingly predicts mortality in the course of congestive heart failure. European Journal of Heart Failure, 7(2), 261–267. https://doi.org/10.1016/j.ejheart.2004.05.011.
Katon, W. J. (2003). Clinical and health services relationships between major depression, depressive symptoms, and general medical illness. Biological Psychiatry, 54(3), 216–226. https://doi.org/10.1016/S0006-3223(03)00273-7.
Katon, W. J., Von Korff, M., Lin, E. H., Simon, G., Ludman, E., Russo, J., & Bush, T. (2004). The pathways study: A randomized trial of collaborative care in patients with diabetes and depression. Archives of General Psychiatry, 61(10), 1042–1049. https://doi.org/10.1001/archpsyc.61.10.1042.
*Kemppainen, J., Johnson, M. O., Phillips, J. C., Sullivan, K. M., Corless, I. B., Reid, P., & Kirksey, K. (2013a). A multinational study of self-compassion and human immunodeficiency virus-related anxiety. International Nursing Review, 60(4), 477-486. https://doi.org/10.1111/inr.12056.
*Kemppainen, J. K., Brion, J. M., Leary, M., Wantland, D., Sullivan, K., Nokes, K., & Eller, L. S. (2013b). Use of a brief version of the self-compassion inventory with an international sample of people with HIV/AIDS. AIDS Care, 25(12), 1513-1519. https://doi.org/10.1080/09540121.2013.780119.
Kılıç, A., Hudson, J., McCracken, L., Ruparelia, R., Fawson, S., & Hughes, L. (2020). A systematic review of the effectiveness of self-compassion related interventions for individuals with chronic physical health conditions. Behavior Therapy. https://doi.org/10.1016/j.beth.2020.08.001.
Kirschner, H., Kuyken, W., Wright, K., Roberts, H., Brejcha, C., & Karl, A. (2019). Soothing your heart and feeling connected: A new experimental paradigm to study the benefits of self-compassion. Clinical Psychology Science, 7(3), 545–565. https://doi.org/10.1177/2167702618812438.
Kroenke, K., Spitzer, R. L., & Williams, J. B. (2001). The PHQ-9. Journal of General Internal Medicine, 16(9), 606–613. https://doi.org/10.1046/j.1525-1497.2001.016009606.x.
Kroenke, K., Strine, T. W., Spitzer, R. L., Williams, J. B., Berry, J. T., & Mokdad, A. H. (2009). The PHQ-8 as a measure of current depression in the general population. Journal of Affective Disorders, 114(1-3), 163–173. https://doi.org/10.1016/j.jad.2008.06.026.
Leaviss, J., & Uttley, L. (2015). Psychotherapeutic benefits of compassion-focused therapy: An early systematic review. Psychological Medicine, 45(5), 927–945. https://doi.org/10.1017/s0033291714002141.
Liberati, A., Altman, D. G., Tetzlaff, J., Mulrow, C., Gøtzsche, P. C., Ioannidis, J. P., Clarke, M., Devereaux, P. J., Kleijnen, J., & Moher, D. (2009). The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Medicine, 6(7), e1000100. https://doi.org/10.1136/bmj.b2700.
Lilliehorn, S., Hamberg, K., Kero, A., & Salander, P. (2010). Admission into a helping plan: A watershed between positive and negative experiences in breast cancer. Psycho-oncology, 19(8), 806–813. https://doi.org/10.1002/pon.1619.
Lovibond, P. F., & Lovibond, S. H. (1995). The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behavior Research and Therapy, 33(3), 335–343. https://doi.org/10.1016/0005-7967(94)00075-U.
Lucre, K. M., & Corten, N. (2013). An exploration of group compassion-focused therapy for personality disorder. Psychology and Psychotherapy: Theory, Research and Practice, 86(4), 387–400. https://doi.org/10.1111/j.2044-8341.2012.02068.x.
MacBeth, A., & Gumley, A. (2012). Exploring compassion: A meta-analysis of the association between self-compassion and psychopathology. Clinical Psychology Review, 32(6), 545–552. https://doi.org/10.1016/j.cpr.2012.06.003.
Marsh, I. C., Chan, S. W., & MacBeth, A. (2018). Self-compassion and psychological distress in adolescents—A meta-analysis. Mindfulness, 9(4), 1101–1027. https://doi.org/10.1007/s12671-017-0850-7.
Moher, D., Liberati, A., Tetzlaff, J., & Altman, D. G. (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Medicine, 6(7), e1000097. https://doi.org/10.1136/bmj.b2535.
*Morrison, A. E., Zaccardi, F., Chatterjee, S., Brady, E., Doherty, Y., Robertson, N., Hadjiconstantinou, M., Daniels, L., Hall, A., Khunti, K. & Davies, M. J. (2019). Self-compassion, metabolic control and health status in individuals with type 2 diabetes: A UK observational study. Experimental and Clinical Endocrinology & Diabetes. https://doi.org/10.1055/a-0897-3772
Moussavi, S., Chatterji, S., Verdes, E., Tandon, A., Patel, V., & Ustun, B. (2007). Depression, chronic diseases, and decrements in health: Results from the World Health Surveys. The Lancet, 370(9590). https://doi.org/10.1016/S0140-6736(07)61415-9.
Muris, P., & Petrocchi, N. (2017). Protection or vulnerability? A meta-analysis of the relations between the positive and negative components of self-compassion and psychopathology. Clinical Psychology & Psychotherapy, 24(2), 373–383. https://doi.org/10.1002/cpp.2005.
National Institute for Health and Care Excellence. (2009). Depression in adults with a chronic physical health problem: Recognition and management: CG91. https://www.nice.org.uk/guidance/cg91/chapter/1-Guidance
National Institute for Health and Care Excellence. (2011). Generalised anxiety disorder and panic disorder in adults: Management: CG113. https://www.nice.org.uk/guidance/cg113
Neff, K. (2003a). The development and validation of a scale to measure self-compassion. Self and Identity, 2(3), 223–250. https://doi.org/10.1080/15298860309027.
Neff, K. (2003b). Self-compassion: An alternative conceptualization of a healthy attitude toward oneself. Self and Identity, 2(2), 85–101. https://doi.org/10.1080/15298860309032.
Neff, K. (2016). The self-compassion scale is a valid and theoretically coherent measure of self-compassion. Mindfulness, 7(1), 264–274. https://doi.org/10.1007/s12671-016-0560-6.
Neff, K. D., Tóth-Király, I., Yarnell, L. M., Arimitsu, K., Castilho, P., Ghorbani, N., & Kotsou, I. (2019). Examining the factor structure of the Self-Compassion Scale in 20 diverse samples: Support for use of a total score and six subscale scores. Psychological Assessment, 31(1), 27. https://doi.org/10.1037/pas0000629.
Ng, T. P., Niti, M., Tan, W. C., Cao, Z., Ong, K. C., & Eng, P. (2007). Depressive symptoms and chronic obstructive pulmonary disease: Effect on mortality, hospital readmission, symptom burden, functional status, and quality of life. Archives of Internal Medicine, 167(1), 60–67. https://doi.org/10.1001/archinte.167.1.60.
Noble, A., Reilly, J., Temple, J., & Fisher, P. (2018). Cognitive-behavioural therapy does not meaningfully reduce depression in most people with epilepsy: A systematic review of clinically reliable improvement. Journal of Neurology, Neurosurgery, and Psychiatry, 89, 1129–1137. https://doi.org/10.1136/jnnp-2018-317997.
Normann, N., van Emmerik, A., & Morina, N. (2014). The efficacy of metacognitive therapy for anxiety and depression: A meta-analytic review. Depression and Anxiety, 31(5), 402–411. https://doi.org/10.1002/da.22273.
Pinto-Gouveia, J., Duarte, C., Matos, M., & Fráguas, S. (2014). The protective role of self-compassion in relation to psychopathology symptoms and quality of life in chronic and in cancer patients. Clinical Psychology & Psychotherapy, 21(4), 311–323. https://doi.org/10.1002/cpp.1838.
*Przezdziecki, A., & Sherman, K. A. (2016). Modifying affective and cognitive responses regarding body image difficulties in breast cancer survivors using a self-compassion-based writing intervention. Mindfulness, 7(5), 1142-1155. https://doi.org/10.1007/s12671-016-0557-1
*Przezdziecki, A., Sherman, K. A., Baillie, A., Taylor, A., Foley, E., & Stalgis-Bilinski, K. (2013). My changed body: Breast cancer, body image, distress and self-compassion. Psycho-oncology, 22(8), 1872-1879. https://doi.org/10.1002/pon.3230.
Raes, F., Pommier, E., Neff, K. D., & Van Gucht, D. (2011). Construction and factorial validation of a short form of the self-compassion scale. Clinical Psychology & Psychotherapy, 18(3), 250–255. https://doi.org/10.1002/cpp.702.
Rockliff, H., Karl, A., McEwan, K., Gilbert, J., Matos, M., & Gilbert, P. (2011). Effects of intranasal oxytocin on “compassion focused imagery”. Emotion, 11(6), 1388–1396. https://doi.org/10.1037/a0023861.
*Schellekens, M. P., Karremans, J. C., van der Drift, M. A., Molema, J., van den Hurk, D. G., Prins, J. B., & Speckens, A. E. (2017). Are mindfulness and self-compassion related to psychological distress and communication in couples facing lung cancer? A dyadic approach. Mindfulness, 8(2), 325-336. https://doi.org/10.1007/s12671-016-0602-0.
Schuling, R., Huijbers, M., van Ravesteijn, H., Donders, R., Cillessen, L., Kuyken, W., & Speckens, A. (2020). Recovery from recurrent depression: Randomized controlled trial of the efficacy of mindfulness-based compassionate living compared with treatment-as-usual on depressive symptoms and its consolidation at longer term follow-up. Journal of Affective Disorders, 273, 265–273. https://doi.org/10.1016/j.jad.2020.03.182.
*Sherman, K. A., Woon, S., French, J., & Elder, E. (2017). Body image and psychological distress in nipple-sparing mastectomy: The roles of self-compassion and appearance investment. Psycho-oncology, 26(3), 337-345. https://doi.org/10.1002/pon.4138.
*Skinta, M. D., Fekete, E. M., & Williams, S. L. (2019). HIV-stigma, self-compassion, and psychological well-being among gay men living with HIV. Stigma and Health, 4(2), 179. https://doi.org/10.1037/sah0000133.
Sprangers, C. E., & Schwartz, M. A. (2000). Adaptation to changing health: Response shifts in quality of life research. Washington DC: American Psychological Association.
Temple, J., Salmon, P., Tudor-Smith, C., Huntley, C., Byrne, A., & Fisher, P. (2020). The questionable efficacy of manusalised psychological treatments for breast cancer patients: An individual patient data meta-analysis. Clinical Psychology Review, 80, 101883. https://doi.org/10.1016/j.cpr.2020.101883.
*Todorov, N., Sherman, K. A., Kilby, C. J., & Breast Cancer Network Australia. (2019). Self-compassion and hope in the context of body image disturbance and distress in breast cancer survivors. Psycho-oncology, 28(10), 2025-2032. https://doi.org/10.1002/pon.5187.
Turner, J., & Kelly, B. (2000). Emotional dimensions of chronic disease. Western Journal of Medicine, 172, 124–128. https://doi.org/10.1136/ewjm.172.2.124.
Van den Brink, E., & Koster, F. (2015). Mindfulness-based compassionate living: a new training programme to deepen mindfulness with heartfulness. London: Routledge.
*Ventura, A. D., Nefs, G., Browne, J. L., Friis, A. M., Pouwer, F., & Speight, J. (2019). Is self-compassion related to behavioural, clinical and emotional outcomes in adults with diabetes? Results from the second diabetes MILES-Australia (MILES-2) study. Mindfulness, 10(7), 1222-1231. https://doi.org/10.1007/s12671-018-1067-0.
Walters, P., Schofield, P., Howard, L., Ashworth, M., & Tylee, A. (2011). The relationship between asthma and depression in primary care patients: A historical cohort and nested case control study. PLoS One, 6(6), e20750. https://doi.org/10.1371/journal.pone.0020750.
Wells, A. (2009). Metacognitive therapy for anxiety and depression. New York: Guildford.
Williams, J., Plassman, B., Burke, J., Holsinger, T., & Benjamin, S. (2010). Preventing Alzheimer's disease and cognitive decline: Evidence report/technology assessment no. 193 (Prepared by the Ducke Evidence-Based Practice Center under contract No. HHSA 290-2007-1006_I). http://archive.ahrq.gov/research/findings/evidence-based-reports/alzcogtp.html
*Williams, S., Fekete, E., & Skinta, M. (2019). Self-compassion in PLWH: Less internalized shame and negative psychosocial outcomes. Behavioral Medicine, 1-9. https://doi.org/10.1080/08964289.2019.1659749.
Xiao, F., Song, X., Chen, Q., Dai, Y., Xu, R., Qiu, C., & Guo, Q. (2017). Effectiveness of psychological interventions on depression in patients after breast cancer surgery: A meta-analysis of randomized controlled trials. Clinical Breast Cancer, 17(3), 171–179. https://doi.org/10.1016/j.clbc.2016.11.003.
Zhi-da Wang, Y. F. X., Zhao, Y., & Chen, L. M. (2017). Cognitive behavioural therapy on improving the depression symptoms in patients with diabetes: A meta-analysis of randomized control trials. Bioscience Reports, 37(2). https://doi.org/10.1042/BSR20160557.
*Zhu, L., Yao, J., Wang, J., Wu, L., Gao, Y., Xie, J., Liu, A., Ranchor, A. V. & Schroevers, M. J. (2019). The predictive role of self-compassion in cancer patients’ symptoms of depression, anxiety, and fatigue: A longitudinal study. Psycho-oncology, 28(9), 1918-1925. https://doi.org/10.1002/pon.5174.
Zigmond, A., & Snaith, R. (1983). The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica, 67(6), 361–370. https://doi.org/10.1111/j.1600-0447.1983.tb09716.x.
Author information
Authors and Affiliations
Contributions
MH conducted searches, screened papers, extracted data, assessed risk of bias, contributed to data analysis and wrote the first draft of the manuscript. SLB and MGC designed and supervised the conduct of the review and contributed to writing and editing. SC supervised the conduct of the review and contributed to writing and editing. SD screened papers and cross-checked data extraction and assessment of risk of bias.
Corresponding author
Ethics declarations
Conflict of Interest
The authors report no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hughes, M., Brown, S.L., Campbell, S. et al. Self-Compassion and Anxiety and Depression in Chronic Physical Illness Populations: a Systematic Review. Mindfulness 12, 1597–1610 (2021). https://doi.org/10.1007/s12671-021-01602-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12671-021-01602-y