Abstract
Objectives
Mindfulness-based cognitive therapy (MBCT) is an emerging psychological treatment that might be beneficial for people with bipolar disorder (BD). Neurocognitive studies suggest that MBCT may have important effects on mood regulation and broad attentional and frontal-executive control in BD. In this qualitative study, the process of change of MBCT in people with BD is explored.
Methods
The current qualitative study was part of a multicenter randomized controlled trial (RCT) on (cost-)effectiveness of MBCT for BD. Semi-structured interviews were conducted with a purposive sample of 16 participants who participated in an 8-week MBCT. For reasons of triangulation, teachers were interviewed as well.
Results
Three themes arose from the data: (1) awareness of thoughts, emotions, bodily sensations, and behavior and insight into their inter-relationship; (2) behavioral change; and (3) positive consequences following MBCT. A distinction was made between general aspects and aspects related specifically to BD. Themes were divided into subthemes. Process of change took place in a non-linear, iterative fashion.
Conclusions
Qualitative data support the notion that several cognitive and behavioral processes in BD could be potential targets for MBCT. We suggest that future mediation, neuroimaging, and cognitive experimental studies should explore MBCT as an adjunctive treatment strategy for BD by investigating possible working mechanisms of MBCT in BD.
Trial Registration
ClinicalTrials.gov, NCT03507647. Registered 25th of April 2018, https://clinicaltrials.gov/ct2/show/NCT03507647
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Bipolar disorder (BD) is a severe and chronic mental illness with high recurrence, morbidity, and mortality rates (Novick et al. 2010). Two main clinical subtypes of BD that are recognized include BD type I (e.g., occurrence of at least one manic episode, often accompanied by depressive episodes) and BD type II (e.g., occurrence of at least one hypomanic and at least one depressive episode) (American Psychiatric Association 2013). According to the World Health Organization (World Health Organization 2008), BD is one of the leading causes of disability, affecting approximately 2.4% of people worldwide (Merikangas et al. 2011). Treatment is mainly based on pharmacological interventions, but psychological treatments, such as cognitive behavioral and interpersonal therapy, have been shown to improve the course of BD as well (Reinares et al. 2014). In spite of prophylactic medication and psychological interventions, about half of people with BD experience recurrence within a year (Rush et al. 2006) and three quarters relapse within 5 years (Gitlin et al. 1995; Perry et al. 1999). Furthermore, studies show that people with BD often experience residual mood symptoms in between episodes (Judd et al. 2008; Perlis et al. 2006).
Mindfulness-based cognitive therapy (MBCT) was originally developed to prevent relapse in remitted patients with recurrent major depressive disorder (MDD; Segal et al. 2012). Mindfulness can be described as intentional, present-moment, nonjudgmental awareness (Kabat-Zinn 1990). MBCT integrates mindfulness-based practices with elements of cognitive therapy and encourages patients to adopt a more accepting and non-reactive way to relate to thoughts and emotions (Segal et al. 2012). MBCT has been effective in a broad range of psychiatric disorders, including MDD, substance use disorders, and anxiety disorders (Goldberg et al. 2018; Kuyken et al. 2016).
There are neuropsychological reasons to assume that MBCT could be helpful in the treatment of BD. In a review of existing neurocognitive models for BD, six main processes were identified: (1) increased rumination; (2) dysfunctional use of reappraisal strategies, which refers to the ability to challenge negative automatic thoughts and replace them with more realistic thoughts; (3) reduced activity in the attention control network; (4) dysfunctions in mood regulation; (5) reward processing; and (6) response inhibition/impulsivity (Malhi et al. 2015). Processes of MBCT that contribute to positive changes, i.e., possible working mechanisms, include enhanced self-regulation, attention control, emotion regulation, and self-awareness (Tang et al. 2015). It is suggested that MBCT for MDD results in a reduction of recurrence by enhancing recognition, decentering and disengaging from ruminative thought patterns, developing meta-awareness, and fostering self-compassion (Segal et al. 2012). These mechanisms seem to be important for BD as well but need further evaluation in future studies (Stange et al. 2011).
Published data on efficacy of MBCT in people with BD, with only three underpowered RCTs and four open-label trials, are scarce (Lovas and Schuman-Olivier 2018). However, these studies show that MBCT holds promise in the treatment of BD and appears to be well tolerated. To date, only one qualitative study in 12 people with BD focused on the experience and the process of change of MBCT (Chadwick et al. 2011). Results revealed seven main themes: being able to focus on what is present, clearer awareness of mood state and mood change, increased acceptance of mood changes, benefits of adapting mindfulness practice to different mood states, being able to reduce/stabilize negative affect, relating differently to negative thoughts, and being able to reduce the impact of mood states. Clinical implications derived from that study include more flexible use of homework and additional support for depressive patients. However, the MBCT offered in the Chadwick study was substantially adapted: the sessions were much shorter (weekly sessions of 90 rather than 150 minutes) and meditations briefer (10 rather than 45-min homework practices). In addition, little was reported about the influence of manic symptoms on MBCT and vice versa.
The current qualitative study aims to examine the process of change with MBCT in people with BD, both regarding general aspects (e.g., general changes relating to themselves and their lives) and aspects of BD itself (e.g., more specific changes relating to their illness) and hereby generate a data driven description on the process of change.
Method
Participants
A purposive sample of 19 patients with BD who followed MBCT were invited to participate in the current qualitative study, 16 of whom agreed to be interviewed and 3 refused because of having too many other obligations. The majority of participants were diagnosed with BD type I (n = 10). The mean duration of illness was 25 years (range 3–47). Most participants attended at least seven MBCT sessions, with a mean of 6.9 sessions attended. All participants in the current study used mood stabilizing medication. Sociodemographic and clinical characteristics of the participants are provided in Table 1.
Procedure
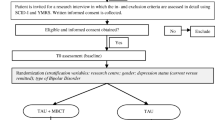
The current study is part of an ongoing RCT comparing MBCT in addition to treatment as usual (TAU) versus TAU alone in people with BD (Hanssen et al. 2019). Within 3 months after completing the MBCT training, eligible participants were invited by telephone to take part in an individual face-to-face interview for the current qualitative study. Participants of the current study were selected by means of purposive sampling, which means that participants were selected based on certain criteria in order to achieve a diverse study sample as possible. This way, information is gathered from different perspectives and will give insight in multiple angles and experiences on the process of change (Denzin and Lincoln 2018). We selected participants on terms of gender, age, diagnosis (BD type I or II), study site (Pro Persona, Altrecht, and Dimence), and dropout. Two female residents in psychiatry (MB and NH), experienced in treating people with BD, interviewed the participants. Both interviewers had participated in an MBCT training themselves. One of them was experienced in meditation. The interviewers had not been involved in either the clinical care or the MBCT training of the participants. During the interview, one of the interviewers was in the lead, and the other interviewer made notes and asked additional questions. All interviews had a duration of 45 to 90 min. Most interviews were conducted at the study sites; one interview was conducted at the participants’ home because of the travelling distance. After interviewing 16 participants, no new data emerged from the data, and data saturation was reached. By achieving data saturation, there is conceptual concordance within the data set, which provides certainty with the analysis (Denzin and Lincoln 2018).
The intervention was an adapted version of MBCT, a group skills-training program originally designed as a relapse prevention program for people with recurrent depression by Segal et al. (2012). The training consisted of eight weekly sessions of 2.5 h and one silent day. In addition, participants were instructed to practice 45 min every day with online-guided mindfulness exercises. The training was adapted to people with BD by including psychoeducation about manic and depressive symptoms, introducing the 3-min breathing space earlier and more often in the program and applying movement exercises more frequently (Hanssen et al. 2019). The training was taught by pairs of qualified mindfulness teachers and nurses specialized in the care of people with BD. The mindfulness teachers met the advanced criteria of the Association of Mindfulness-Based Teachers in the Netherlands and Flanders and the internationally agreed good practice guidelines of the UK Network for Mindfulness-Based Teachers (Crane et al. 2013; Hanssen et al. 2019). Each group consisted of eight to ten participants.
Measures
Before starting the interviews, the Quick-Inventory of Depressive Symptomology–Self Rated (QIDS; Rush et al. 2003) and the Altman Self-Rating Mania Scale (ASRM; Altman et al. 1997) Altman et al. 1997) were administered to assess the presence of depressive and (hypo)manic symptoms. The semi-structured interview consisted of a topic list, starting with two open-ended questions: “How did you experience the mindfulness training?” and “what has the training brought you?” Furthermore, the topic list included prompts that specifically asked about the process in general or related to bipolar disorder and to ensure that topics that were still underexposed were discussed. See Table 2 for an overview of the topic list used during the semi-structured interviews. During the interview, the interviewers would probe for more detail when deemed necessary. All interviews were recorded with a dictaphone, transcribed verbatim and sent to the participants for verification.
Data Analyses
The coding and analyzing were done in a multistage process, following the guidelines of Boeije (2014). The research team consisted of six people: three psychiatrists (MLvB, ER, AS), one psychologist researcher (IH), and two interviewers (MB, NH). Two psychiatrists of the team had special expertise in diagnosing and treating adult BD (MLvB, ER), one in the application of mindfulness-based interventions (AS), and two members of the team were familiar with qualitative research (AS, ER).
The coding and analysis consisted of three coding phases: open coding, axial coding, and selective coding (Boeije 2014). In this way, coding was data driven instead of theory driven. A repeating cycle was entered, consisting of transcribing and analyzing five interviews before conducting the next five interviews. The cycle was repeated until saturation of the data was reached. By discussion in the research team, the strategy of interviewing was adapted to the data that emerged in every phase. Open coding consisted of reading and re-reading the interviews while coding the text, during which a code list was developed. To ensure reliability, the transcripts were coded independently by the two interviewers and the found codes were compared and discussed until agreement was reached. The list of codes was used during the coding of the next interviews, and new codes were created if existing codes did not match the data. This phase was followed by the phase of axial coding in which the interviewers aggregated codes into broader categories and (sub)themes. This was done by consensus with the research team. In this way, a data-driven description of the process of change of MBCT in people with BD came forward. During the whole process, the program ATLAS.ti (2019) was used, software for analyzing and classifying of qualitative data.
For reasons of triangulation, the six teachers and nurses who provided the training were interviewed as well, by means of a focus group. During the focus group, the interviewers used a topic list which contained the same topics as discussed in the interviews with patients but took into account the view of the trainer. The focus group was transcribed and coded by the psychologist researcher (IH) of the research team.
Results
Process of Change
Three overarching key themes emerged from the data: awareness and insight, behavioral change, and positive consequences. A distinction was made between general aspects and aspects related specifically to BD. Change did not typically occur in a linear fashion but rather appeared to be an iterative process. Participants mentioned that by gaining more awareness, they changed their behavior. By changing their behavior, they gained more insight, which in turn created more awareness of behavioral patterns, and so on. An illustrative example of this iterative process comes from participant #6 who reported that he had always been violating his boundaries when feeling depressed. After the MBCT training, he paid more attention to his current mood state (behavior), as a result of which he was able to notice subtle depressive symptoms sooner (awareness and insight). Therefore, he was able to set appropriate boundaries and ask for help earlier (behavior). As a consequence, others were more understanding towards him and stressful assignments at work and at home were reduced (consequences). This created more space for the participant to notice what he presently needed (awareness and insight) and to take better care of that (behavior), for example, by cancelling stressful meetings and taking more rest. This resulted in an increased sense of control over his depressive state (consequences). The key themes and subthemes identified in the analysis are presented in Table 3. Examples are added to allow for appraisal of the fit between the data and the authors’ understanding, in accordance with good practice guidelines. Each theme and subtheme are described below.
Awareness and Insight
The first theme was further subdivided into four subthemes: (1) awareness; (2) allowing; (3) decentering; and (4) insight. Insight appeared on three levels, namely, on inter-relatedness between dimensions, automatic responses, and change in attitudes.
Awareness
The process of change was generally experienced by participants to start with an increase in awareness of both their internal state and their environment. This included thoughts, bodily sensations, emotions, and sensory information as they appeared in the present moment. In general, one participants stated: “I learned to be more aware of ‘hey, that train passes by’, taking in the sounds you hear, feeling the warmth of the sun on your skin or the rain drops on your face, the wind in your hair. That kind of things.” (P#10) Specifically to BD, participants described an increased awareness of mood changes and behavior that they labeled as (hypo)manic or depressive. Being more aware of the subtler changes allowed them to recognize prodromal signs of their mood destabilizing at an earlier stage. Specifically to BD, one participant stated: “I always thought that I did have depression but that it was not that bad with the manic symptoms. Now I find out that I do .. not really get manic... but I do often have moments like ‘oh, I feel better than I normally do’. I was not really aware of that before.” (P#3) The teachers confirmed that participants became more aware of the subtle mood changes. In addition, the teachers mentioned that participants learned to recognize whether their mood changes were still within the normal range or not.
Allowing
Participants described allowing their experiences more. Especially unpleasant emotions or bodily sensations were better tolerated, which resulted in a more accepting and welcoming stance towards them. In general, one participant stated: “When I am going to have a difficult conversation, I can now say to myself: ‘it is hard for you to talk to that person now, you are scared of what will happen, that it will be too intense, but that is alright’.”(P#9) While some participants tended to avoid difficult feelings before, they now started to be able to direct their attention towards them. Specifically to BD, one participant stated: “I now try to acknowledge the depressive feelings sooner […] and try not to think ‘go away, go away, go away’, you know, so running away from it, but more like ‘let it happen, because it will come anyway’.” (P#11)
Decentering
Several participants described they acquired an ability to view their inner and outer experiences from a different perspective. They could observe their thoughts and behavior without coinciding with them, with acceptance and nonjudgmentally. In general, one participant stated: “When I look at my work and it is sometimes really hectic, at that moment I can take some distance from it by doing really simple practices.” (P#3) This decentering enabled participants to also step back from depressive or (hypo)manic thoughts and behaviors, putting them more into perspective. Specifically to BD, one participant stated: “I am an artist, so I start my own projects. Therefore, I have to be careful with the hypomanic episodes not to start too big or too complicated things. Because then it gets out of hand. I think meditation is a way […] to take a step back. Being aware of what you are doing and if that is getting too much, or if you should in fact do more.” (P#13) Teachers confirmed that participants acquired the ability to decenter from intrusive thoughts.
Insight
Through the course of the program, many participants were able to gain insight, facilitated by enhanced awareness, allowing, and decentering. The insight they described typically appeared on three different levels. The first level was insight regarding the inter-relatedness between bodily sensations, thoughts, and emotions. Participants described they started seeing the influence of thoughts on mood state and vice versa. In general, one participant stated: “An effect of the meditation for me is that I sense I can put things in order, things that happen and things I feel in my body. Now, for instance, I am feeling a bit tense, here (points at stomach). A bit hard and sore, it seems. If I start breathing towards it, which you do of course while meditating, then it eventually disappears.” (P#8) By understanding the inter-relatedness of different dimensions of experience, both self-knowledge and understanding of BD improved. Specifically to BD, one participant stated: “I recognize that is how it works, also in other people, that you have certain thoughts and that the thoughts somehow reinforce each other. Like, if you think ‘I am on top of the world’, that is also how you are going to feel.” (P#8) The second level was insight regarding automatic behavioral patterns. Participants reported they learned to recognize certain behavioral patterns that were not helpful and even led to exhaustion. In general, one participant stated: “Many things you just do, you keep going until at a certain moment you notice ‘now I have reached a limit’. However, between the start and the limit there has also been a trajectory. The good thing is that in that moments that you need it, you can say ‘listen, I notice something, what am I doing now?’” (P#6) Some participants gained insight in their avoidance of negative emotions or not accepting their diagnosis of BD. Insight in automatic behavioral patterns also facilitated recognition of patterns linked to mood episodes, such as certain types of behavior when becoming (hypo)manic or depressed. Specifically to BD, one participant stated: “When I suddenly tap into a source of energy, then there must be something going on. I then get very energetic, want to undertake many things and become very social. That is the moment that I have to be on guard.” (P#3) The third level of insight can be described as change in attitude. Participants reported to have become more aware of their needs and wishes, their boundaries, and their physical and mental limitations. They recognized their own influence on certain aspects of their life and started to reflect on their values. In general, one participant stated: “You are more aware of ‘what is important to me’, ‘what do I want and what is the complete opposite of what I want’, to eventually reach what I do want. And just because of the moments you incorporate that, through mindfulness, I have given myself and those thoughts more space and made choices accordingly.” (P#10) Teachers confirmed that gaining insight in the inter-relatedness between bodily sensation, thoughts and emotions, and habitual behavioral patterns was an important aspect, especially in relation to mood changes. This helped participants to gain insight in the way they were inclined to respond to mood symptoms and how to act on this differently. Specifically to BD, one participant stated: “I try to give more attention to what it is I really want and what a feeling stands for. Is it pure or am I a bit on the hypomanic side? And if it is not pure and you are on the hypomanic side, you should particularly not get personally involved with someone and start broadcasting how beautiful that person is, or anything. Then something is wrong.” (P#9)
Behavioral Change
The second theme was further subdivided into two themes: (1) intrapersonal (e.g., within the self), which was further divided into directing attention, planning, and self-care; and (2) interpersonal (e.g., between the self and others).
Intrapersonal
The first intrapersonal aspect that emerged from the data was the intentional direction of attention. This encompassed having the choice to direct the attention to a chosen object and whenever distracted, being able to return and sustain the attention. Participants described they more often directed their attention to the here and now (of: the present). In general, one participant stated: “While you are doing a meditation or a breathing exercise you notice ‘oh, here are those thoughts again’. So you notice the thoughts and then it is the question what you do with them. Do you follow them or can you decide to go back to the body? Like ‘those thoughts can be there, I’ll get to them later’. You have a bit more ability to direct your attention.” (P#9) Being able to direct the attention helped participants to choose not to give as much attention to depressive thoughts as they did before. Specifically to BD, one participant stated: “It seems to me that I am more aware of repeating worried or depressed thoughts. I sooner think ‘what am I doing?’ and then think ‘go focus on something else’.” (P#9) A second aspect was a change in planning. Participants mentioned they started prioritizing in their agendas and taking more time for themselves. They tried not to do too many things at the same time, like they did before. In general, one participant stated: “At work especially, you have to do a lot of things at once. Now I can sort things out and organize that in a better way […] Like, first this and then that, not wanting to do all things at the same time.” (P#12) Some participants mentioned they now downsized their agendas when they noticed prodromal signs of their mood destabilizing, as a preventive method to avoid worsening. Specifically to BD, one participant stated: “I now notice that I start being a bit more agitated, but that’s because I have a lot of projects running simultaneously at the moment. […] I am aware of that and I think ‘I must do some meditation shortly and then I must see if I can structure things or if I can skip stuff.” (P#13) Furthermore, improvement of executive control was often mentioned and for some participants this led to less reactivity to both internal and external stimuli. Sometimes facilitated by decentering, this helped participants to not act on (hypo)manic thoughts or ideas immediately. For instance, a participant who was inclined to impulsively reconnect to his ex-partner only in manic phases was able not to do that anymore. The third reported aspect of intrapersonal behavior was self-care. Several participants tended to be more caring towards themselves. They mentioned taking more rest, creating a more peaceful environment and stop violating their boundaries. In general, one participant stated: “Thanks to mindfulness now I can think ‘It’s enough, so be it.’ Again that phone, that thing goes to silent mode for a while. In fact, I switch off the voicemail and you people will have to call me back. Not now, because I want to finish up here and then do nothing for about an hour. And that feels good.” (P#10) This also applied to creating optimal conditions for a good night’s rest, which was mentioned to be important to diminish the risk of their mood destabilizing. Specifically to BD, one participant stated: “Now it is easier for me to eliminate stimuli during the day and at work that would normally have had an effect on my mood.” (P#5) Participants also mentioned a more compassionate attitude towards themselves. They had become milder when they encountered shortcomings in themselves and they experienced less self-directed anger. Some participants mentioned to put less pressure on themselves.
Interpersonal
Several changes were mentioned in the behavior towards others. Various participants described to have become better listeners, being able not to interrupt the person they were having a conversation with. Some participants also experienced they less often needed other people to help regulate their emotions, because they were more capable to regulate emotions by themselves. In general, one participant stated: “Normally I would call my parents, but now I do that a lot less frequently. I am really learning that. To really feel it and letting it sink in, so to speak.” (P#7) Besides this, participants described expressing emotions to others more often, in an adaptive way. Some participants involved other people more frequently, also in dealing with their BD. Specifically to BD, one participant stated: “At a certain point I told my supervisor ‘listen, this is the case, I have bipolar disorder and it doesn’t mean I have to go on sick leave right away’. But in retrospect I do notice that it was the right moment to share it with them, so they understand. Now they know what is going on and they will get it if I say ‘listen, I had a bad night, I start two or three hours later’ or ‘I work from home today’.”(P#6) It also allowed others to take part in detecting subtle symptoms of mood dysregulation and then help participants to act on them adaptively. Teachers confirmed that it was helpful for participants to involve others more often, because this made it easier for other people to help participants when they were experiencing difficulties with their mood regulation. Furthermore, teachers mentioned that it became easier for participants to ask for help from others when needed.
Positive Consequences
The third theme was subdivided into four subthemes: (1) cognitive; (2) emotional; (3) physical; and (4) interpersonal.
Cognitive
Several cognitive consequences emerged from the data. Participants reported a reduction in distractive and ruminative thoughts. In general, many participants mentioned they had experienced a decrease in number of thoughts, both positive and negative, leading to an increased sense of mental calmness. Some participants reported they had a wider range of thoughts and less tunnel vision after MBCT. In some participants, this resulted in more space for new thoughts and more creative thinking. Concentration was experienced by a number of participants to be enhanced, allowing them to stay focused on a task and to keep an overview. In general, one participant stated: “My ability to focus in conversations improved. That is something that it brought me, I can discern primary from secondary issues again.” (P#5) In (hypo)manic phases, this allowed a participant not to get dragged along by big plans he made. Specifically to BD, one participant stated: “I notice my ability to focus improved so I have more of an overview. For instance, I am now writing a grant application. Two or four years ago if I was doing that, I would be making big plans and I would be dragged along by all the plans for the future that I had. […] Now there is more structure. I notice this in terms of content, linguistically, and I now have a better overview and more calmness.” (P#13) Teachers confirmed that participants had a reduction of intrusive thoughts.
Emotional
Emotions were better tolerated and participants were able to be more in touch with their feelings. Because of this, some participants mentioned they felt more authentic. In general, one participant stated: “Sometimes I can hear a piece of music and suddenly become very emotional. I also have the impression that is the result of mindfulness, that you move closer to your emotions. […] I can just start crying.” (P#12) One participant mentioned being more autonomous, as a consequence of an enhanced ability to regulate her emotions and make choices on her own. They experienced an increased sense of control over their emotions, which in some led to a decrease of fear for their emotional fluctuations and in return a decrease of avoiding emotions. A reduction of anxiety in general was observed, as well as a decrease of other negative affect, including worry, shame, and self-directed anger. This led to an increase in positive mood states, as experienced by participants. Teachers confirmed that participants experienced decreases of negative affect and anxiety during the training. A decrease in severity as well as duration of depressive episodes was pointed out by several participants and in general a stabilization of mood. Some noticed an increased sense of having a grip on the symptoms of BD and some experienced more hope for the future during a depressive episode. Furthermore, participants reported a more accepting attitude towards circumstances that could not be changed. A number of participants reported acknowledging symptoms of BD earlier as such, while they usually tended to deny them. Specifically to BD, one participant stated: “I am not very good at dealing with my emotions. At a certain moment they fall inwards if that goes on for too long and […] I start feeling dark and become depressed. With the mindfulness I notice that I manage to get closer to my feelings.” (P#3) A more compassionate attitude led to an increased acceptance of having BD and the entailing consequences in a number of participants. Teachers confirmed that they recognized a more accepting attitude from participants towards themselves and their BD.
Physical
Participants experienced more physical relaxation as a result of MBCT and one participant experienced a decrease in physical pain. In general, one participant stated: “That relaxation, first it is about your body and then the rest follows automatically.” (P#4) Some also reported that their breathing had become calmer. A number of participants mentioned they could fall asleep at night more easily. Specifically to BD, one participant stated: “When I am stressed out and I wake up at night I do a mindfulness exercise of about fifteen minutes. Then the chances are that I fall asleep again. [..] In the past I would have been awake for two hours.” (P#3)
Interpersonal
Some participants reported an increased trust and compassionate attitude towards others. An increased trust in others led them to better tolerate and take advice from others, also during (hypo)manic or depressive episodes. In general, one participant stated: “I can discuss things and accept advices from others now. I did not used to. I always wanted to decided everything alone and that was what I always did.” (P#5) By involving others in the management of their illness and its consequences, participants were met with greater understanding from their social environment. Specifically to BD, one participant stated: “I never used to talk about my bipolar disorder. But now, when I am feeling down and not in the mood to go out and meet others, I can explain and they understand.” (P#12) Teachers confirmed that participants more often expressed their feelings and boundaries towards others, leading to more understanding from their environment.
Discussion
The current study aimed at exploring the experiences of people with BD with adapted MBCT regarding the process of change. Three overarching themes were found: awareness and insight, behavioral changes, and positive consequences. The described components of the process of change are probably highly interrelated and mutually facilitate each other.
The identified themes in the current study are in line with the qualitative study of Chadwick et al. (2011). However, the current data showed many additional aspects of the process of change, particularly those being more specific to BD. As in the Chadwick study, a clearer awareness of mood change was mentioned by participants. However, in the current study, decentering from not only depressive but also (hypo)manic thoughts and behavior were pointed out. Combined with an improvement of impulse control, this helped participants not to act on (hypo)manic thoughts or ideas immediately. In addition to learning to focus on what is present, which was a theme that emerged in the Chadwick study, the current study found that participants became more capable of directing their attention in general. This allowed them, for example, to direct their attention away from depressive thought content. Furthermore, as in the Chadwick study, the current study found a reduction in the frequency and intensity of negative affect. In addition, the current study also found a reduction in the frequency of distracting and ruminative thoughts, both positive and negative, resulting in a sense of mental calmness.
A recent systematic review of clinical and neurocognitive findings of MBCT for BD reported that there is preliminary evidence to support a positive effect on anxiety, residual depression, mood regulation, and broad attentional and frontal-executive control (Lovas and Schuman-Olivier 2018). Furthermore, they describe several neurocognitive processes in BD that could be potential targets for MBCT, including attention control, reappraisal and emotion regulation, response inhibition, and rumination. The findings of the current study support this notion, as participants subjectively mentioned improvements in these domains after following MBCT.
Limitations and Future Research Directions
A limitation of the current study is the time frame during which the interviews took place. All interviews were conducted about three months after finishing MBCT, which is a relatively short time period. It would be interesting to investigate whether the process of change as mentioned by the participants is an ongoing process at the long-term.
It is important to notice that, although the current study finds some subjective symptomatic benefits of MBCT for BD, the qualitative methodology does not allow us to draw any conclusions on the effectiveness of MBCT for BD. As such, an important research implication drawn from the current study is the need for an adequately powered, randomized controlled trial in order to test the hypothesis that MBCT could be helpful in the treatment for BD.
The current study supports the notion that several neuropsychological processes in BD could be potential targets for MBCT, including attention control, reappraisal and emotion regulation, response inhibition, and rumination. This implicates that future moderation, mediation, neuroimaging, and cognitive experimental studies should explore MBCT as an adjunctive treatment strategy for BD by investigating possible working mechanisms. Specifically, it is of importance to investigate whether these mechanisms are dependent on individual variations among people with BD in type, stages, and other characteristics of the disorder. This might be important to further tailor MBCT to the needs of people with BD. Finally, data of the current study suggest that attention for (hypo)mania is an important aspect in MBCT for BD, in order to ensure participants gain more insight on this part of the mood spectrum.
The current qualitative data provide several possible targets and working mechanisms for MBCT in BD that need further investigation and add to the preliminary evidence suggesting that MBCT holds promise as an adjunctive treatment option for people with BD.
Data Availability
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
References
Altman, G., Hedeker, D., Peterson, J. L., & Davis, J. M. (1997). The Altman Self-Rating Mania Scale. Society of Biological Psychiatry, 42, 948–955. https://doi.org/10.1016/S0006-3223(96)00548-3.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (DSM-5®) (fifth ed.). American Psychiatric Association.
ATLAS.ti. (2019). Scientic Software Development GmbH
Boeije, H. (2014). Analysis in qualitative research. Sage Publications.
Chadwick, P., Kaur, H., Swelam, M., Ross, S., & Ellett, L. (2011). Experience of mindfulness in people with bipolar disorder: a qualitative study. Psychothery Research, 21(3), 277–285. https://doi.org/10.1080/10503307.2011.565487.
Crane, R. S., Eames, C., Kuyken, W., Hastings, R. P., Williams, J. M. G., Bartley, T., Evans, A., Silverton, S., Soulsby, J. G., & Surawy, C. (2013). Development and validation of the Mindfulness-Based Interventions–Teaching Assessment Criteria (MBI:TAC). Assessment, 20(6), 681–688. https://doi.org/10.1177/1073191113490790.
Denzin, N. K., & Lincoln, Y. S. (2018). The SAGE Handbook of qualitative research (5th ed.). SAGE publications.
Gitlin, M. J., Swendsen, J., Heller, T. L., & Hammen, C. (1995). Relapse and impairment in bipolar disorder. The American Journal of Psychiatry, 152(11), 1635–1640. https://doi.org/10.1176/ajp.152.11.1635.
Goldberg, S. B., Tucker, R. P., Greene, P. A., Davidson, R. J., Wampold, B. E., Kearney, D. J., & Simpson, T. L. (2018). Mindfulness-based interventions for psychiatric disorders: a systematic review and meta-analysis. Clinical Psychology Review, 59, 52–60. https://doi.org/10.1016/j.cpr.2017.10.011.
Hanssen, I., Huijbers, M. J., Lochmann-van Bennekom, M., Regeer, E., Stevens, A., Evers, S., Wensing, M., Kupka, R., & Speckens, A. (2019). Study protocol of a multicenter randomized controlled trial of mindfulness-based cognitive therapy and treatment as usual in bipolar disorder. BMC Psychiatry, 19(130), 1–10. https://doi.org/10.1186/s12888-019-2115-6.
Judd, L. L., Schettler, P. J., Akiskal, H. S., Coryell, W., Leon, A. C., Maser, J. D., & Solomon, D. A. (2008). Residual symptom recovery from major affective episodes in bipolar disorders and rapid episode relapse/recurrence. Archives of General Psychiatry, 65(4), 386–394. https://doi.org/10.1001/archpsyc.65.4.386.
Kabat-Zinn, J. (1990). Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. Delacorte Press.
Kuyken, W., Warren, F., Taylor, R. S., Whalley, B., Crane, C., Bondolfi, G., Hayes, R., Huijbers, M. J., Ma, H., Schweizer, S., Segal, Z., Speckens, A. E. M., Teasdale, J. D., Van Heeringen, K., Williams, J. M. G., Byford, S., Byng, R., & Dalgleish, T. (2016). Efficacy of mindfulness-based cognitive therapy (MBCT) in prevention of depressive relapse: an individual patient data meta-analysis from randomized trials. JAMA Psychiatry, 73(6), 565–574. https://doi.org/10.1001/jamapsychiatry.2016.0076.
Lovas, D. A., & Schuman-Olivier, Z. (2018). Mindfulness-based cognitive therapy for bipolar disorder: a systematic review. Journal of Affective Disorders, 240, 247–261. https://doi.org/10.1016/j.jad.2018.06.017.
Malhi, G. S., Byrow, Y., Fritz, K., Das, P., Baune, B. T., Porter, R. J., & Outhred, T. (2015). Mood disorders: neurocognitive models. Bipolar Disorders, 17, 3–20. https://doi.org/10.1111/bdi.12353.
Merikangas, K. R., Jin, R., He, J., Kessler, R. C., Lee, S., Sampson, N. A., Viana, M. C., Andrade, L. H., Hu, C., & Karam, E. G. (2011). Prevalence and correlates of bipolar spectrum disorder in the world mental health survey initiative. Archives of General Psychiatry, 68(3), 241–251. https://doi.org/10.1001/archgenpsychiatry.2011.12.
Novick, D. M., Swartz, H. A., & Frank, E. (2010). Suicide attempts in bipolar I and bipolar II disorder: a review and meta-analysis of the evidence. Bipolar Disorders, 12(1), 1–9. https://doi.org/10.1111/j.1399-5618.2009.00786.x.
Perlis, R. H., Ostacher, M. J., Patel, J. K., Marangell, L. B., Zhang, H., Wisniewski, S. R., Ketter, T. A., Miklowitz, D. J., Otto, M. W., & Gyulai, L. (2006). Predictors of recurrence in bipolar disorder: primary outcomes from the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD). American Journal of Psychiatry, 163(2), 217–224. https://doi.org/10.1176/appi.ajp.163.2.217.
Perry, A., Tarrier, N., Morriss, R., McCarthy, E., & Limb, K. (1999). Randomised controlled trial of efficacy of teaching patients with bipolar disorder to identify early symptoms of relapse and obtain treatment. British Medical Journal, 318(7177), 149–153. https://doi.org/10.1136/bmj.318.7177.149.
Reinares, M., Sanchez-Moreno, J., & Fountoulakis, K. N. (2014). Psychosocial interventions in bipolar disorder: what, for whom, and when. Journal of Affective Disorders, 156, 46–55. https://doi.org/10.1016/j.jad.2013.12.017.
Rush, A. J., Trivedi, M. H., Ibrahim, H. M., Carmody, T. J., Arnow, B., Klein, D. N., Markowitz, J. C., Ninan, P. T., Kornstein, S., Manber, R., Thase, M. E., Kocsis, J. H., & Keller, M. B. (2003). The 16-Item Quick Inventory of Depressive Symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): a psychometric evaluation in patients with chronic major depression. Biological Psychiatry, 54(5), 573–583. https://doi.org/10.1016/s0006-3223(02)01866-8.
Rush, A. J., Trivedi, M. H., Wisniewski, S. R., Nierenberg, A. A., Stewart, J. W., Warden, D., Niederehe, G., Thase, M. E., Lavori, P. W., & Lebowitz, B. D. (2006). Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: a STAR* D report. American Journal of Psychiatry, 163(11), 1905–1917. https://doi.org/10.1176/ajp.2006.163.11.1905.
Segal, Z. V., Williams, J. M. G., & Teasdale, J. D. (2012). Mindfulness-Based Cognitive Therapy for Depression (2nd ed.). Guilford Press.
Stange, J. P., Eisner, L. R., Holzel, B. K., Peckham, A. D., Dougherty, D. D., Rauch, S. L., Nierenberg, A. A., Lazar, S., & Deckersbach, T. (2011). Mindfulness-based cognitive therapy for bipolar disorder: effects on cognitive functioning. Journal of Psychiatric Practice, 17(6), 410–419. https://doi.org/10.1097/01.pra.0000407964.34604.03.
Tang, Y.-Y., Hölzel, B. K., & Posner, M. I. (2015). The neuroscience of mindfulness meditation. Nature Reviews Neuroscience, 16(4), 213. https://doi.org/10.1038/nrn3916.
World Health Organization. (2008). The global burden of disease: 2004 update. Geneva, Switzerland: WHO.
Acknowledgments
The authors would like to thank the participants for sharing their story. Furthermore, we would like to thank the MBCT teachers, without whom this study would not have been possible.
Funding
The RCT that this qualitative study is part of is externally funded by a grant from ZonMw, the Netherlands Organization for Health Research and Development (Grant Number: 843002803) awarded to Prof. Dr. A. E. M. Speckens and dr. M. J. Huijbers. The funding agency will have no role in data collection, management, analysis, interpretation of data; writing of the report; or the decision to submit the report for publication.
Author information
Authors and Affiliations
Contributions
IH and MB contributed equally to this manuscript and should be considered joint first author.
All authors contributed to this manuscript. IH was responsible the logistics of the large RCT. AS is the principal investigator. NH and MB contacted participants for participation in the current qualitative study. Furthermore, they were responsible for conducting the interviews, and for transcribing and coding the interviews. IH, NH, MB, AS, ER, and MLvB all were involved with the data analysis. IH and MB drafted this manuscript, which was supplemented by all other authors. All authors have read and approved the final paper.
Corresponding author
Ethics declarations
Conflict of Interest
IH and AS both work at the Radboudumc Centre for Mindfulness, as a PhD student and professor, respectively. MB and NH were residents in psychiatry at the Radboudumc Centre for Mindfulness when conducting this study.
Ethics Approval
The study protocol has been approved by the ethical review board CMO Arnhem – Nijmegen and is registered under number NL63319.091.17. The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hanssen, I., Boele, M., van der Horst, N. et al. The Process of Change of Mindfulness-Based Cognitive Therapy for People with Bipolar Disorder: a Qualitative Study. Mindfulness 12, 863–872 (2021). https://doi.org/10.1007/s12671-020-01551-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12671-020-01551-y