Abstract
Background
Functional dyspepsia (FD) is a commonly encountered entity worldwide and is difficult to treat. Most of the treatment modalities have low-quality evidence for use, except for proton pump inhibitors. Aerobic exercise has been shown to improve the symptoms, but its direct effect on symptoms has never been studied. The objective was to study the effects of moderate aerobic exercise on symptoms of FD and to compare the effect of conventional treatment alone vs. exercise plus conventional treatment.
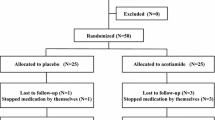
Methods
Out of 112 patients, 72 were randomly divided into controls (conventional treatment; n=36) and experimental (aerobic exercise for 30 min per session, 5 times a week for 6 weeks with conventional treatment; n=36) groups. Both the groups were assessed on day 1 and at the end of 6 weeks, using Glasgow Dyspepsia Severity Score (GDSS), Depression Anxiety Stress Scales-42 (DASS-42), and visual analogue scale (VAS).
Results
Pre-treatment GDSS, DASS-42, and VAS in the experimental group were significantly different as compared to the post-treatment scores (p=0.00019, p=0.0002, p=0.00019, respectively). Even in the control group, pre- and post-treatment GDSS, DASS-42, and VAS scores were significantly different (p=0.00019, p=0.0002, p=0.00019, respectively). However, on the head-to-head comparison of the 2 groups, scores at the end of 6 weeks were significantly different (p< 0.05), in favor of the experimental group.
Conclusion
Aerobic exercise as an auxiliary therapy to conventional treatment has better outcomes in the functional well-being of dyspepsia.

Similar content being viewed by others
References
Garber CE, Blissmer B, Deschenes MR, et al. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43:1334–59.
Simrén M. Physical activity and the gastrointestinal tract. Eur J Gastroenterol Hepatol. 2002;14:1053–6.
Stanghellini V, Chan FK, Hasler WL, et al. Gastroduodenal disorders. Gastroenterology. 2016;150:1380–92.
Tack J, Bisschops R, Sarnelli G. Pathophysiology and treatment of functional dyspepsia. Gastroenterology. 2004;127:1239–55.
Koduru P, Irani M, Quigley EMM. Definition, pathogenesis, and management of that cursed dyspepsia. Clin Gastroenterol Hepatol. 2018;16:467–79.
Van Oudenhove L, Vandenberghe J, Demyttenaere K, Tack J. Psychosocial factors, psychiatric illness and functional gastrointestinal disorders: a historical perspective. Digestion. 2010;82:201–10.
Bakkali-Kassemi L, El Ouezzani S, Magoul R, et al. Effects of cannabinoids on neuropeptide Y and β-endorphin expression in the rat hypothalamic arcuate nucleus. Br J Nutr. 2011;105:654–60.
Wahid A, Manek N, Nichols M, et al. Quantifying the association between physical activity and cardiovascular disease and diabetes: a systematic review and meta-analysis. J Am Heart Assoc. 2016;5:e002495.
Bae JY. Aerobic exercise increases meteorin-like protein in muscle and adipose tissue of chronic high-fat diet-induced obese mice. Biomed Res Int. 2018;2018:6283932.
Scribbans TD, Vecsey S, Hankinson PB, et al. The effect of training intensity on VO2max in young healthy adults: a meta-regression and meta-analysis. Int J Exerc Sci. 2016;9:230–47.
Gundersen J, Levine BD. Maximal oxygen uptake as a parametric measure of cardiorespiratory capacity. Med Sci Sports Exerc. 2007; 39:103-7. Erratum in: Med Sci Sports Exerc. 2007; 39:574.
World Health Organization. Global strategy on diet, physical activity and health. Title of document: what is moderate intensity and vigorous intensity physical activity? Available via https://www.who.int/dietphysicalactivity/physical_activity_intensity/en/. Accessed 8 September 2020.
Jetté M, Sidney K, Blümchen G. Metabolic equivalents (METS) in exercise testing, exercise prescription, and evaluation of functional capacity. Clin Cardiol. 1990;13:555–65.
Shahsavarani AM, Ashayeri H, Lotfian M, et al. The effects of stress on visual selective attention: the moderating role of personality factors. J Am Sci. 2013;9:1–16.
El-Omar EM, Banerjee S, Wirz A, McColl KE. The Glasgow Dyspepsia Severity Score--a tool for the global measurement of dyspepsia. Eur J Gastroenterol Hepatol. 1996;8:967–71.
Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck depression and anxiety inventories. Behav Res Ther. 1995;33:335–43.
Misra A, Chowbey P, Makkar BM, et al. Consensus statement for diagnosis of obesity, abdominal obesity and the metabolic syndrome for Asian Indians and recommendations for physical activity, medical and surgical management. J Assoc Physicians India. 2009;57:163–70.
Wani RT. Socioeconomic status scales-modified Kuppuswamy and Udai Pareekh’s scale updated for. J Family Med Prim Care. 2019;2019:8,1846–9.
Kumar A, Pate J, Sawant P. Epidemiology of functional dyspepsia. J Assoc Physicians India. 2012;60:9–12.
Talley NJ, Weaver AL, Zinsmeister AR. Impact of functional dyspepsia on quality of life. Dig Dis Sci. 1995;40:584–9.
Monés J, Adan A, Segú JL. Quality of life in functional dyspepsia. Dig Dis Sci. 2002;47:20–6.
Wiklund I, Glise H, Jerndal P, et al. Does endoscopy have a positive impact on quality of life in dyspepsia? Gastrointest Endosc. 1998;47:449–54.
Mahadeva S, Yadav H, Rampal S, Goh KL. Risk factors associated with dyspepsia in a rural Asian population and its impact on quality of life. Am J Gastroenterol. 2010;105:904–12.
Mahadeva S, Yadav H, Rampal S, et al. Ethnic variation, epidemiological factors and quality of life impairment associated with dyspepsia in urban Malaysia. Aliment Pharmacol Ther. 2010;31:1141–51.
Mahadeva S, Wee HL, Goh KL, Thumboo J. The EQ-5D (Euroqol) is a valid generic instrument for measuring quality of life in patients with dyspepsia. BMC Gastroenterol. 2009;9:20.
Black CJ, Houghton LA, Ford AC. Insights into the evaluation and management of dyspepsia: recent developments and new guidelines. Ther Adv Gastroenterol. 2018;11:1–17.
Matsuzaki J, Suzuki H, Masaoka T, et al. Influence of regular exercise on gastric emptying in healthy men: a pilot study. J Clin Biochem Nutr. 2016;59:130–3.
Strid H, Simrén M, Störsrud S, et al. Effect of heavy exercise on gastrointestinal transit in endurance athletes. Scand J Gastroenterol. 2011;46:673–7.
Welén K, Faresjö A, Faresjö T. Functional dyspepsia affects women more than men in daily life: a case-control study in primary care. Gend Med. 2008;5:62–73.
Gontar AS, Halim S, Sitepu RR. Dyspepsia and Depression, Anxiety, Stress Scales (DASS) Score. Indones J Gastroenterol Hepatol Dig Endosc. 2016;17:28–31.
Göktaş Z, Köklü S, Dikmen D, et al. Nutritional habits in functional dyspepsia and its subgroups: a comparative study. Scand J Gastroenterol. 2016;51:903–7.
Ho KY, Kang JY. SeowA. Prevalence of gastrointestinal symptoms in a multiracial Asian population, with particular reference to reflux-type symptoms. Am J Gastroenterol. 1998;93:1816–22.
Hu WH, Wong WM, Lam CL, et al. Anxiety but not depression determines health care-seeking behaviour in Chinese patients with dyspepsia and irritable bowel syndrome: a population-based study. Aliment Pharmacol Ther. 2002;16:2081–8.
Yang SY, Lee OY, Bak YT, et al. Prevalence of gastroesophageal reflux disease symptoms and uninvestigated dyspepsia in Korea: a population-based study. Dig Dis Sci. 2008;53:188–93.
Rabeneck L, Cook KF, Wristers K, et al. SODA (severity of dyspepsia assessment): a new effective outcome measure for dyspepsia-related health. J Clin Epidemiol. 2001;54:755–65.
Talley NJ, Phillips SF, Melton J 3rd, et al. A patient questionnaire to identify bowel disease. Ann Intern Med. 1989;111:671–4.
Junghard O, Lauritsen K, Talley NJ, Wiklund IK. Validation of seven graded diary cards for severity of dyspeptic symptoms in patients with non-ulcer dyspepsia. Eur J Surg Suppl. 1998;583:106–11.
Talley NJ, Haque M, Wyeth JW, et al. Development of a new dyspepsia impact scale: the Nepean Dyspepsia Index. Aliment Pharmacol Ther. 1999;13:225–35.
Sander GB, Mazzoleni LE, Francesconi CF, et al. Development and validation of a cross-cultural questionnaire to evaluate non ulcer dyspepsia: the Porto Alegre Dyspeptic Symptoms Questionnaire (PADYQ). Dig Dis Sci. 2004;49:1822–9.
Calvet X, Bustamante E, Montserrat A, et al. Validation of phone interview for follow-up in clinical trials on dyspepsia: evaluation of the Glasgow Dyspepsia Severity Score and a Likert-scale symptoms test. Eur J Gastroenterol Hepatol. 2000;12:949–53.
Crawford JR, Henry JD. The Depression Anxiety Stress Scales (DASS): normative data and latent structure in a large non-clinical sample. Br J Clin Psychol. 2003;42:111–31.
Huang ZP, Yang XF, Lan LS, et al. Correlation between social factors and anxiety-depression in function dyspepsia: do relationships exist? Prz Gastroenterol. 2014;9:348–53.
Kim YS, Song BK, Oh JS, Woo SS. Aerobic exercise improves gastrointestinal motility in psychiatric inpatients. World J Gastroenterol. 2014;20:10577-84.
Heijnen S, Hommel B, Kibele A, Colzato LS. Neuromodulation of aerobic exercise—a review. Front Psychol. 2015;6:1890.
Crosby KM, Bains JS. The intricate link between glucocorticoids and endocannabinoids at stress-relevant synapses in the hypothalamus. Neuroscience. 2012;204:31–7.
Heyman E, Gamelin FX, Goekint M, et al. Intense exercise increases circulating endocannabinoid and BDNF levels in humans—possible implications for reward and depression. Psychoneuroendocrinology. 2012;37:844–51.
Marco EM, García-Gutiérrez MS, Bermúdez-Silva FJ, et al. Endocannabinoid system and psychiatry: in search of a neurobiological basis for detrimental and potential therapeutic effects. Front Behav Neurosci. 2011;5:63.
Patrick RP, Ames BN. Vitamin D and the omega-3 fatty acids control serotonin synthesis and action, part 2: relevance for ADHD, bipolar, schizophrenia, and impulsive behavior. FASEB J. 2015;29:2207–22.
Harmer CJ. Serotonin and emotional processing: does it help explain antidepressant drug action? Neuropharmacology. 2008;55:1023–8.
Foley TE, Fleshner M. Neuroplasticity of dopamine circuits after exercise: implications for central fatigue. Neuromolecular Med. 2008;10:67–80.
Tziatzios G, Gkolfakis P, Papanikolaou, et al. Gut microbiota dysbiosis in functional dyspepsia. Microorganisms. 2020;8:691.
Bravo JA, Forsythe P, Chew MV, et al. Ingestion of Lactobacillus strain regulates emotional behavior and central GABA receptor expression in a mouse via the vagus nerve. Proc Natl Acad Sci U S A. 2011;108:16050–5.
Mika A, Van Treuren W, González A, et al. Exercise is more effective at altering gut microbial composition and producing stable changes in lean mass in juvenile versus adult male F344 rats. PLoS One. 2015;10:e0125889.
Author information
Authors and Affiliations
Contributions
Siddhesh Vijay Rane, Bharati Asgaonkar, Pravin Rathi, Qais Contractor, Sanjay Chandnani, Parmeshwar Junare, Prasanta Debnath, and Vidya Bhat were involved in conceptualizing and designing the study. Siddhesh Vijay Rane, Bharati Asgaonkar, Pravin Rathi, Qais Contractor, and Vidya Bhat searched the literature. Siddhesh VijayRane and Bharati Asgaonkar acquired the data and analyzed it with Pravin Rathi, Qais Contractor, Sanjay Chandnani, Parmeshwar Junare, and Prasanta Debnath. The initial manuscript was prepared by Siddhesh Vijay Rane, Bharati Asgaonkar, Sanjay Chandnani, and Vidya Bhat. Manuscript editing was done by Pravin Rathi, Qais Contractor, Sanjay Chandnani, Parmeshwar Junare, and Prasanta Debnath. All the authors agreed upon the final version.
Corresponding author
Ethics declarations
Conflict of interest
SVR, BA, PR, QC, SC, PJ, PD, and VB declare that they have no conflict of interest.
Ethics statement
The study was performed conforming to the Helsinki declaration of 1975, as revised in 2000 and 2008 concerning human and animal rights, and the authors followed the policy concerning informed consent as shown on Springer.com.
Disclaimer
The authors are solely responsible for the data and the contents of the paper. In no way, the Honorary Editor-in-Chief, Editorial Board Members, the Indian Society of Gastroenterology or the printer/publishers are responsible for the results/findings and content of this article.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Rane, S.V., Asgaonkar, B., Rathi, P. et al. Effect of moderate aerobic exercises on symptoms of functional dyspepsia. Indian J Gastroenterol 40, 189–197 (2021). https://doi.org/10.1007/s12664-021-01174-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12664-021-01174-8