Abstract
Objective
The study was conducted to assess the usefulness by qualitative comparison between the two intravenous sedative drugs, Diazepam and Propofol and to provide sedation in apprehensive and uncooperative patients undergoing day care oral surgical procedures.
Methods
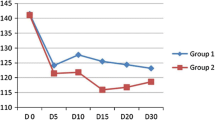
The present study was conducted on 20 adult patients, 10 in each group (Propofol and Diazepam) irrespective of age and sex. Intravenous sedation of Propofol compared with Diazepam in terms of onset of action, recovery, and anterograde amnesia, patient co-operation, surgeon’s convenience and side effects and other parameters.
Results
Propofol was found to be the superior sedating agent compared to Diazepam, having rapid onset and predictability of action, profoundness of amnesia and a faster recovery period, offering advantages of early patient discharge and better patient compliance.
Conclusion
Propofol was found to be an ideal sedating agent in day care oral surgical procedures.




Similar content being viewed by others
References
Vanderbijl P, Roelofse JA (1987) Intravenous midazolam in oral surgery. Int J Oral Maxillofac Surg 16:325–332
Sarasin DS, Ghoneim NM (1996) Effect of sedation with midazolam or propofol on cognition and psychomotor functions. J Oral Maxillofac Surg 54:1187–1193
Wylie Report (1981) Report of the working party on training in dental anesthesia. Br Dent J 151:385–388
Rodrigo MRC, Rosenquist JB (1989) Conscious sedation with Propofol. Br Dent J 166:75–79
White Paul F (1988) Propofol pharmacokinetic and pharmacodynamics. Semin Anesth 7:4–20
Guy J (1991) The neuropharmacology of propofol. J Drug Dev 4:103–105
Cillo Joseph E, Buffalo NY (1999) Propofol anaesthesia for outpatient oral maxillofacial surgery. Oral Surg Oral Med Oral Path 87:530–538
Adam HK, Briggs LP (1983) Pharmacokinetic evaluation of ICI 35868 in man. Br J Anaesth 55:97–103
Van Doze A, Westphal LM et al (1986) Comparison of propofol with methohexital for outpatient anesthesia. Anaesth Analg 65:1189–1195
Logan MR, Duggan JE et al (1987) Single shot IV anesthesia for outpatient dental surgery. Br J Anaesth 59:179–183
Richter James J et al (1981) Current theories about the mechanism of benzodiazepines and neuroleptic drugs. Anaesthesiology 54:66–72
Malamed Stanley F (1985) Sedation: a guide to patient management, 1st edn. The C.V. Mosby Company, St. Louis
Wood N, Sheikh A et al (1986) Midazolam and Diazepam for minor oral surgery. Br Dent J 160:9–12
Grattidge P (1992) Patient controlled sedation using Propofol in day surgery. Anaesthesia 47:683–685
Vickers MD (1965) The measurement of recovery from anesthesia. Br J Anesth 37:296–302
Ramsay MA, Savege TM et al (1974) Controlled sedation with alphaxalone alphadolone. Br Medical J 2:656–659
Edmondson H (1972) Biochemical evidence of anxiety in dental patients. Br Med J 4:712
Bennett CR (1984) Conscious sedation: an alternative to general anaesthesia. J Dent Res 63:832–833
Keilty SR, Blackwood S (1969) Sedation for conservative dentistry. Br Dent J of Clin Pract 23:365
Dixon HR, Tilton BE et al (1970) A comparison of the sedative and cardiopulmonary effects of Diazepam and Pentazocine premedication. Anaesth Analg 49:546
Valtonen M, Saloen M et al (1989) Propofol infusion for sedation in outpatient oral surgery. A comparison with Diazepam. Anesthesia 44:730–734
Nusstein J, Berlin J et al (2004) Comparison of injection pain, heart rate increase, post injection pain of articaine and lidocaine in a primary intraligamentary injection administered with a computer-controlled local anesthetic delivery system. J Anesth 51:126–133
Struys M, Versichelen L et al (1997) Comparison of computer controlled administration of Propofol with two manually controlled infusion techniques. Anaesthesia 52:41–50
Grounds RM, Lelor JM et al (1987) Propofol infusion for sedation in the intensive care unit. Preliminary report. Br Med J 294:397–400
Eriksson M, Englesson S et al (1997) Effects of lignocaine and pH on Propofol induced pain. Br J Anaesth 78:502–506
Mitchell Paul F (1980) Diazepam associated thrombophlebitis. J Am Dent Assoc 101:492–495
Barclay JK, Hunter KM et al (1985) Midazolam and Diazepam compared as sedatives for out patient surgery under local analgesia. Oral Surg Oral Med Oral Pathol 59:349–355
Wilbur K, Zed PJ (2001) Is propofol an optimal agent for procedural sedation and rapid sequence intubation in the emergency department? CJEM 3(4):302–310
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nirwan, A.S., Jain, N., Pragasm, M. et al. Randomised Comparative Study on Propofol and Diazepam as a Sedating Agent in Day Care Surgery. J. Maxillofac. Oral Surg. 13, 583–591 (2014). https://doi.org/10.1007/s12663-013-0537-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12663-013-0537-0