Abstract
This study aimed to address current gaps in the literature on the impacts of Mental Health First Aid (MHFA) training by comparing long-term outcomes on different cohorts. University students studying health and non-health degrees, university staff and community members who had completed MHFA within the past three years completed a survey to assess their mental health literacy, and their use of knowledge and skills acquired through the training. The study found few significant differences between the different group outcomes and between different time points post-completion of MHFA. This study found that although participant-reported measures show positive outcomes from MHFA, further research on the common tools used to rate mental health literacy and how mental health literacy impacts behaviours and help-seeking would provide greater insight into the outcomes of running MHFA as a mental health prevention and early intervention program at universities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mental illness is a rampant issue in Australia, with one in five (21.4%) Australians having a mental or behavioural condition in 2020–2021 (Australian Bureau of Statistics, 2022). For people aged 15–24, this is particularly prevalent, with almost one in two (46.6%) females and almost one in three (31.2%) males experiencing a mental or behavioural condition (Australian Bureau of Statistics, 2022). High rates of mental ill-health in this age bracket are relevant to universities as 62% of university students are under 25 years of age (Department of Education, 2022). The latest National Tertiary Student Wellbeing Survey also found that two-thirds of Australian students rate their mental health as fair or poor, two-thirds rate their psychological distress as high or very high (Rickwood et al., 2017).
There are a range of barriers that impact upon university students’ ability to deal with poor mental health outcomes. One such barrier is poor mental health literacy (Gorczynski et al., 2017; Zochil & Thorsteinsson, 2018). Due to lack of knowledge and understanding of mental health conditions, university students are frequently unable to recognise symptoms and identify the need to access support (Gorczynski et al., 2017; Zochil & Thorsteinsson, 2018). Another significant barrier is the logistics of accessing professional help, including having to call to book an appointment with a counsellor or not knowing where and how to get to scheduled appointments (Gagnon et al., 2017). In this context, universities have a range of unique opportunities to deliver multi-faceted and intensive prevention and early intervention programs to meet students’ mental health needs and break down barriers (Orygen, 2017). Although universities choose to resource, fund, embed and deliver these mental health interventions differently, often, interventions involve the running of mental health promotion programs or short mental health courses.
The Mental Health First Aid (MHFA) is a short course that is rapidly expanding worldwide. In 2019, MHFA was run over 4500 times and over 800,000 Australians had completed the course (Mental Health First Aid Australia, 2019). The 12-h course, designed for the community, covers an array of mental health conditions and mental health crises (Kitchener et al., 2017). When delivered in university settings, MHFA aims to teach basic skills to all students and staff and to encourage help-seeking, reduce stigma and teach skills to facilitate peer support (Kitchener & Jorm, 2017).
Although MHFA training is one of the most researched mental health interventions for university students (Lo et al., 2018), there are still gaps in the literature. These gaps include an overwhelming focus on MHFA training delivered to students completing health-related degrees (Bond et al., 2015; Burns et al., 2017; Kitchener & Jorm, 2017; McCormack et al., 2018; O'Reilly et al., 2011; Rose et al., 2019) and therefore, neglecting those students who are less likely to have mental health knowledge and skills gained through their course curriculum. Other gaps in research are the length of time that participants experience the positive outcomes of MHFA (Burns et al., 2017; Rose et al., 2019), the impact of MHFA on help-seeking behaviours and how MHFA impacts the mental health of the participant (Gorczynski et al., 2017). With MHFA’s growing popularity, filling these gaps and understanding the outcomes will allow for greater targeting and use of MHFA to meet students’ mental health needs, and therefore, support mental health promotion practitioners in designing their interventions in university settings. The present study aims to contribute to addressing some of these gaps by comparing the long-term outcomes of MHFA training on different cohorts of university students and comparing them with the outcomes experienced by staff and members of the general community.
Methods
Participants
The study involved a convenience sample of students and staff from a Sydney-based university and community members who had completed the training through a local mental health organisation based in Sydney within the last three years. Participants were included in the study if they met the inclusion criteria of having completed the full MHFA course, were older than 18 years of age and could read English.
An invitation for survey participation went to all participants who had completed MHFA training through the university and a partner organisation within the past three years. Participants received two emails, with the second sent out two weeks following the initial invitation. A total of 531 emails were sent each time, 344 from the university database and 187 from the mental health partner organisation.
Study Design
This was a cross-sectional and correlational study looking at the relationship between different sample groups at a specific time point. The survey included validated instruments to measure mental health literacy: the Mental Health Literacy Scale (MHLS) and the General Help-Seeking Questionnaire (GHSQ). The MHLS is a 35-item scale-based measure that assesses attributes of mental health literacy. Items in the scale identify one’s knowledge about mental health conditions including recognition, risk factors, causes and treatment (O’Connor & Casey, 2015). The first 15 items are given a mark out of four (with 1—very unlikely/unhelpful to 4—very likely/helpful) and the remaining 20 out of five (with 1—strongly disagree/definitely unwilling to 5—strongly agree/definitely willing). Eleven of the 35 questions are reverse scored to increase reliability of results. In total, the MHLS has a minimum score of 35 and a maximum of 160. MHLS has good tester–retester reliability and internal consistency (O’Connor & Casey, 2015). The GHSQ aims to assess intentions to seek help and from whom people are likely to seek help (Wilson et al., 2005). The GHSQ requires participants to rate from 1 to 7 how likely they are to get help from a range of people for a personal or emotional problem and for suicidal thoughts; participants are provided with 10 different options of people/professionals to rate. In total, the GHSQ has a minimum score of 20 and a maximum of 140. A higher score reflects higher intentions to help-seek (Wilson et al., 2005). The GHSQ also has good test–retest reliability and significant correlation with seeking counselling (Wilson et al., 2005).
In addition to the validated tools, questions about the use of knowledge gained through the MHFA training, including where, when and how many times they used it, and perceived personal mental health benefits from the training, including the level of impact and in what ways they felt the benefits, were included in the survey.
Data Analysis
Participants that were university students were split into two categories based on assumed prior knowledge about mental health from their degrees. Participants put in the health stream student category included students enrolled in any health-related degree but also students that were studying psychology and social work. Non-health stream students were students not studying what was considered a health-related degree or students who answered the question in an unclear manner, making determination of their degree difficult. Students from health stream (HS), students from non-health stream (NHS), university staff (US) and community members (CM) were then also split into three groups based on time post-completion of MHFA. These groups were: (1) had completed MHFA less than 6 months ago, (2) completed MHFA between 7 and 12 months ago, and (3) had completed MHFA more than 12 months ago.
Data were initially analysed using descriptive analysis to help understand distribution patterns. A linear regression model was then used to assess the effects of time since course completion, group, and the interaction between these factors on the results from the MHLS, GHSQ and the number of times knowledge was used.
For the short response questions, a summative content analysis of the text was completed to categorise the data (Hsieh & Shannon, 2005). Following initial thorough familiarisation with the data, the entries were divided into themes and subthemes based on common conceptual similarities and identified patterns found in participant responses. For the question on how knowledge was used, three themes and seven subthemes were identified. For the question on MHFA training’s benefit to personal mental health, five themes were identified. Answers to the question on the contexts in which knowledge gained from the training was used were grouped into personal, work or university/study context. All participants responses were allocated to an identified theme. Details on themes and subthemes are presented in the Results section below.
A logistic regression model was then used to assess relationships between group and time post-completion of MHFA and the interaction between these two factors on categorised data. The model was adjusted for each category comparing the binary outcomes of the category being mentioned in the respondents’ answer with it not being mentioned.
In both the linear and logistic regression models, the variables sex and age were included as possible confounding factors.
All analyses were performed in R software.
Ethics
Ethical approval was secured prior to commencement of the study through the authors’ institutional Human Research Ethics Committee (approval number H13708). All participants provided informed consent to participate in the study.
Results
A total of 185 survey responses were received. However, 62 surveys were unable to be used due to participants having not completed the MHLS part of the survey, leaving 123 useable surveys.
Table 1 shows respondents’ demographic characteristics as well as time since MHFA completion, which ranged from 1 to 38 months prior.
Mean MHLS scores ranged from 125.7 to 143.4 (Fig. 1). The effect of group on MHLS scores was significant (F3,109:5.10; p = 0.002), with students from health stream having a significantly higher mean score than students from non-health stream and university staff. No significant effect was found for time since course completion (F2,109; p = 0.226), or interaction between group and time (F6,109; p = 0.463).
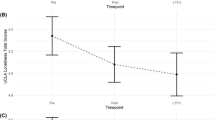
Figure 2 shows the GHSQ scores for experiencing a personal or emotional problem. No significant effect between groups was found (F3,103:0.055; p = 0.983), nor when comparing time since course completion (F2,103:0.531; p = 0.590), or an interaction between group and time (F6,103:0.702; p = 0.648). Figure 3 shows the GHSQ scores for experiencing suicidal thoughts. Again, no significant effect was found between groups (F3,103:0.207; p = 0.891), between time post-completion (F2,103:1.358; p = 0.262) or between groups at each time interval (F6,103:1.754; p = 0.116).
Participants were asked if and how many times they remembered having used the knowledge gained from MHFA. The large majority of respondents (89.7%) indicated using the knowledge they had gained without significant differences between students (health and non-health stream) and non-students (i.e. university staff and community members) on the number of times knowledge was used (F3,90: 1.656; p = 0.182). Time post-completion was significant for both groups of students, as knowledge was used significantly more in students who completed MHFA more than 12 months ago than those who had completed MHFA less than 6 months ago. For non-students, no significant effect of time was observed.
Ninety-three respondents answered the open-ended question where participants could name contexts in which they used their skills. Table 2 shows the distribution of personal, work and university contexts mentioned. A logistic regression model found no statistically significant difference between the groups’ responses.
Sixty-four respondents answered the open-ended question on how they had used the MHFA knowledge. Table 3 highlights the reoccurring themes of supporting others, improved personal skills and helpful for university course content and placements found in participants short responses. A logistic regression model found no statistically significant difference between the groups’ responses in any theme or subtheme.
MHFA benefiting the mental health of participants was reported by 96.6% (n = 116) of respondents. Of the respondents who felt some benefit to their mental health, 95.5% (n = 111) said that the benefit was still ongoing. Of the respondents who reported no longer feeling the benefits of MHFA on their mental health, two completed MHFA training less than 6 months ago and two completed training 7–12 months ago.
One hundred and eight respondents answered the question on the way they had felt the benefit to their mental health. Themes identified (Table 4) included reduced negative stigma, increase recognition of symptoms, equipped with strategies to deal with personal mental health, improved knowledge on mental health conditions and increased self-awareness. A logistic regression model found no statistically significant difference between the groups’ responses in any of the themes.
Discussion
This study uniquely looked at the association of time and group membership (i.e. students from health and non-health streams, university staff and community members) and participant outcomes post-MHFA training completion.
The vast majority of participants (89.7%) in the present study reported using the knowledge they gained from MHFA. This rate was similar to the one found in Kelly and Birks’ (2017) study on nursing and midwifery students, which found that 92% of participants had used their knowledge. However, these are both considerably higher than seen in Ashoorian et al.’s (2018) study, which found a rate of 64.5% when asking students about the use of skills. A possible cause for variation in these rates is the phrasing of the questions. The current study and Kelly & Birks’ (2017) study worded the question as ‘use of knowledge’, whereas Ashoorian et al. (2018) worded the question as ‘application of skills’, possibly implying the use of skills in a mental health crisis, a focus of MHFA training. This hypothesis is further supported in this study’s short responses, often finding that participants reported that they had used their knowledge in simple ways. For example, 53% of participants reported that post-MHFA training they were able to better support a friend or family member with a mental health condition or that MHFA training provided them with “confidence to have conversations about mental health”. MHFA knowledge used subtly by participants is also supported in the other literature where, at two years post-completion, listening without judgement was the most commonly reported use of MHFA skills (Svensson & Hansson, 2014; Yap & Jorm, 2012). Although a relatively ‘simple’ skill, this general use of mental health knowledge in everyday life is increasingly important with mental health conditions on the rise and high rates of mental health conditions in university students.
The study also found that 96.6% of respondents felt MHFA had a direct impact on their mental health. That is a 7.6% higher rate than those who reported that they had used knowledge gained from MHFA. When participants were asked in what ways these benefits were felt, 45.1% reported that MHFA increased their awareness to recognise poor mental health within themselves, and 28.9% mentioned that it equipped them with strategies to deal with their mental health. These strategies included enabling participants to “reach out to my support system”, “know places to go and online resources” that are available and provided a sense of not being alone in struggling with poor mental health. de Jesus Loureiro and Brandão Valente da Costa (2019) found that post-completion of MHFA training students are more likely to seek help for their own mental health problems, although, to the best of our knowledge, there is no other research on MHFA training’s direct impact on participants’ mental health. However, as this study found that a majority of respondents reported they felt a positive impact on their own mental health post-completion, which directly supports the use of MHFA in meeting universities’ mental health promotion goals, further research looking at MHFA training’s direct impact on participants’ mental health would assist and enable deeper understanding of this outcome.
This study’s finding that students from health stream have higher mental health literacy than students from non-health stream is not surprising and is supported in the other literature that used the MHLS on students who had not completed MHFA. Gorczynski et al. (2017) found a mean MHLS score of 122.8 for non-medical university students, and Marwood and Hearn (2019) found a mean score of 127.7 for medical students. This difference is proportionality similar to the current study’s MHLS means of 137.8 for students from non-health stream and 143.0 for students from health stream. This proportional difference between MHLS scores could be attributed to MHFA having a positive impact on the mental health literacy of students from both health and non-health streams. This hypothesis that MHFA training increases the mental health literacy of students is supported in the other literature (Ashoorian et al., 2018; Bond et al., 2015; Burns et al., 2017). However, although a change in mental health literacy can be seen, the MHLS scores in Gorczynski et al. (2017) and Marwood & Hearn (2019) studies are already high. With only a small change in MHLS found in this study post-completion of MHFA, it can be questioned if that size of impact is significantly impacting the mental health literacy of university students.
Lam (2014) found that an increase in mental health literacy levels among school students, particularly classification of depression, was associated with better mental health status. However, research on university students has found that recognition of depression is high at baseline and therefore, no significant change around depression from pre- and post-completion of MHFA is commonly found (Bond et al., 2015; Burns et al., 2017; Morrissey et al., 2017). Gagnon et al.’s (2017) study further argued that university students already have a good awareness of mental health conditions and focus of interventions should be on more practical skills such as information on when to seek help.
Gorczynski et al.’s (2017) study questions the impact of mental health literacy on mental health outcomes in the university student population. Their study found that the MHLS scores were not significantly different between people who were heterosexual and people who were bisexual; however, people who were bisexual indicated significantly lower well-being and higher levels of distress (Gorczynski et al., 2017). This leaves questions as to whether the MHLS is providing an accurate measure of mental health literacy and if mental health and mental health literacy are linked. Potential factors impacting the measurement of mental health literacy may be the length of the tool as well as the depth of its illness-specific content. The high dropout rate seen in this study suggests that these factors may be biasing responses, as participants who find the survey challenging may be opting out halfway through it. Further research looking at mental health literacy and mental health outcomes, both pre- and post-MHFA completion and over a longer period of time, would provide better understanding of the link between the increase in mental health literacy and mental health outcomes. Understanding this link is vital to establish whether MHFA training is an effective mental health prevention and early intervention program for university students.
Limitations
An important limitation of this study was the dropout rate of participants when completing the MHLS. It is likely that this limitation is also experienced by other studies that use the MHLS and highlights the need to explore other ways of more accurately measuring MHL.
A further limitation is the lack of participants’ baseline measure as well as of a control group of participants who had not undergone any mental health first aid training. However, comparisons between individuals with varying times post-completion enabled identification of differences within and across groups of interest (i.e. those who have undergone training). In addition, this longitudinal understanding of MHFA outcomes provided vital information, as there is lack of research on the long-term impacts of MHFA broadly and in university students more specifically (Lo et al., 2018; Morgan et al., 2018). A longitudinal study, including a control group and baseline data at the time of entry in the university, is recommended for future research in this field.
Implications for Practise and Research
Generally, this study has found that MHFA provides a good foundation of mental health literacy for participants, with a considerable perception of increase in the use of the knowledge gained to support others and oneself. This has implication for practise, providing further support to the value of such programs to the university student population. This study has also found that benefits from the course are found across different population groups and, although students from non-health stream present lower levels of MHL than their health counterparts, MHL remains stable for all groups up to 12-month post-completion, a finding that adds to hitherto very limited body of research that has measured the impact of this program beyond 6 months.
However, despite these positive results, this study’s findings raise some important questions. The lack of variability between groups and between timeframes post-completion of the course up to 12 months suggests that either: (1) benefits from the course were too small to make a difference large enough to produce changes over time; or (2) validated instruments commonly used to measure mental health literacy outcomes (in this case, the MHLS and the GHSQ) have low sensibility to detect more subtle differences and therefore, do not present a true and accurate measure of the mental health literacy benefits of such courses. Therefore, we conclude that although participant-reported measures show positive outcomes from MHFA, further research on the tools used to rate mental health literacy and how mental health literacy impacts behaviours, including help-seeking, would provide greater insight into the outcomes of running MHFA as a mental health prevention and early intervention program at universities.
Availability of data
The data that support the findings of this study are available from the corresponding author, AR, upon reasonable request.
References
Ashoorian, D., Albrecht, K.-L., Baxter, C., Giftakis, E., Clifford, R., Greenwell-Barnden, J., & Wylde, T. (2018). Evaluation of Mental Health First Aid skills in an Australian university population. Early Intervention in Psychiatry, 13(5), 1121–1128.
Australian Bureau of Statistics. (2022). National study of mental health and wellbeing, 2020–2021. https://www.abs.gov.au/statistics/health/mental-health/national-study-mental-health-and-wellbeing
Bond, K. S., Jorm, A. F., Kitchener, B. A., & Reavley, N. J. (2015). Mental health first aid training for Australian medical and nursing students: An evaluation study. BMC Psychology, 3(1), 11–11.
Burns, S., Crawford, G., Hallett, J., Hunt, K., Hui, J., & Tilley, P. (2017). What’s wrong with John? A randomised controlled trial of Mental Health First Aid (MHFA) training with nursing students. BMC Psychiatry, 17(1).
de Jesus Loureiro, L. M., & Brandão Valente da Costa, L. M. (2019). Evaluation of the Mental Health First Aid program in undergraduate nursing students. Revista De Enfermagem Referência, 4(20), 9–18.
Department of Education (2022). Selected higher education statistics, 2020 student data. https://www.education.gov.au/higher-education-statistics/student-data/selected-higher-education-statistics-2020-student-data-0
Gagnon, M. M., Gelinas, B. L., & Friesen, L. N. (2017). Mental health literacy in emerging adults in a university setting: Distinctions between symptom awareness and appraisal. Journal of Adolescent Research, 32(5), 642–664.
Gorczynski, P., Sims-schouten, W., Hill, D., & Wilson, J. C. (2017). Examining mental health literacy, help seeking behaviours, and mental health outcomes in UK university students. Journal of Mental Health Training, Education and Practice, 12(2), 111–120.
Hsieh, H.-F., & Shannon, S. E. (2005). Three approaches to qualitative content analysis. Qualitative Health Research, 15(9), 1277–1288.
Kelly, J., & Birks, M. (2017). ‘It’s the simple things you do first that start the process of help’: Undergraduate nursing and midwifery students’ experiences of the Mental Health First Aid course. Collegian, 24(3), 275–280.
Kitchener, B., Jorm, A., & Kelly, C. (2017). Mental Health First Aid Manual (4th ed.). Mental Health First Aid Australia.
Kitchener, B., & Jorm, A. (2017). The role of Mental Health First Aid training in nursing education: A response to Happell, Wilson & McNamara (2015). Collegian, 24(3), 313–315.
Lam, L. T. (2014). Mental health literacy and mental health status in adolescents: A population-based survey. Child and Adolescent Psychiatry and Mental Health, 8(1), 26–26.
Lo, K., Gupta, T., & Keating, J. L. (2018). Interventions to promote mental health literacy in university students and their clinical educators. A systematic review of randomised control trials. Health Professions Education, 4(3), 161–175.
Marwood, M. R., & Hearn, J. H. (2019). Evaluating mental health literacy in medical students in the United Kingdom. Journal of Mental Health Training, Education and Practice, 14(5), 339–347.
McCormack, Z., Gilbert, J. L., Ott, C., & Plake, K. S. (2018). Mental health first aid training among pharmacy and other university students and its impact on stigma toward mental illness. Currents in Pharmacy Teaching and Learning, 10(10), 1342–1347.
Mental Health First Aid Australia. (2019). Welcome to Mental Health First Aid Australia. Retrieved 16/03 from https://mhfa.com.au/
Morgan, A. J., Ross, A., & Reavley, N. J. (2018). Systematic review and meta-analysis of Mental Health First Aid training: Effects on knowledge, stigma, and helping behaviour. PLoS ONE, 13(5), e0197102.
Morrissey, H., Moss, S., Alexi, N., & Ball, P. (2017). Do Mental Health First Aid™ courses enhance knowledge? Journal of Mental Health Training, Education & Practice, 12(2), 69–76.
O’Connor, M., & Casey, L. (2015). The Mental Health Literacy Scale (MHLS): A new scale-based measure of mental health literacy. Psychiatry Research, 229(1), 511–516.
O’Reilly, C. L., Bell, J. S., Kelly, P. J., & Chen, T. F. (2011). Impact of Mental Health First Aid training on pharmacy students’ knowledge, attitudes and self-reported behaviour: A controlled trial. Australian and New Zealand Journal of Psychiatry, 45(7), 549–557.
Orygen. (2017). Under the radar: The mental health of Australian university students. https://www.orygen.org.au/Policy/Policy-Reports/Under-the-radar/Orygen-Under_the_radar_report
Rickwood, D., Telford, N., O’Sullivan, S., Crisp, D., & Magyar, R. (2017). National Tertiary Student Wellbeing Survey 2016. Headspace. https://headspace.org.au/assets/Uploads/headspace-NUS-Publication-Digital.pdf
Rose, T., Leitch, J., Collins, K. S., Frey, J. J., & Osteen, P. J. (2019). Effectiveness of Youth Mental Health First Aid USA for social work students. Research on Social Work Practice, 29(3), 291–302.
Svensson, B., & Hansson, L. (2014). Effectiveness of Mental Health First Aid training in Sweden: A randomized controlled trial with a six-month and two-year follow-up. PLoS ONE, 9(6), e100911.
Wilson, C., Deane, F., Ciarrochi, J., & Rickwood, D. (2005). Measuring help-seeking intentions: properties of the general help-seeking questionnaire. Canadian Journal of Counselling, 39(1), 15–28.
Yap, M. B. H., & Jorm, A. F. (2012). Young people’s mental health first aid intentions and beliefs prospectively predict their actions: Findings from an Australian National Survey of Youth. Psychiatry Research, 196(2–3), 315–319.
Zochil, M. L., & Thorsteinsson, E. B. (2018). Exploring poor sleep, mental health, and help-seeking intention in university students. Australian Journal of Psychology, 70(1), 41–47.
Acknowledgements
The authors would like to acknowledge the support provided by Lifeline Macarthur to the present study, helping distribute the survey to potential participants. We would also like to acknowledge the contribution of each individual participant in the study for their time and insights.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. This study received no external funding.
Author information
Authors and Affiliations
Contributions
CL contributed to data collection, data analysis (under supervision), interpretation of findings, writing (original draft); SS contributed to study design, data curation, statistical analysis, interpretation of findings, writing (review & editing); RS contributed to data collection coordination, interpretation of findings, writing (review & editing); AR contributed to project administration, study design, interpretation of findings, writing (review & editing).
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Ethical approval was secured prior to commencement of the study through Western Sydney University’s Human Research Ethics Committee (approval number H13708).
Consent to participate
All participants provided informed consent to take part in the study.
Consent for publication
All authors agree with the content included in this manuscript and all have given explicit consent to submit it to Psychological Studies.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lancaster, C., Sperandei, S., Saheb, R. et al. The Long-Term Outcomes of Mental Health First Aid Training for University Students. Psychol Stud 68, 463–471 (2023). https://doi.org/10.1007/s12646-023-00745-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12646-023-00745-3