Abstract
Purpose
We aimed to identify whether social determinants of health (SDoH) are associated with the development of sepsis and assess the differences between individuals living within systematically disadvantaged neighbourhoods compared with those living outside these neighbourhoods.
Methods
We conducted a single-centre case-control study including 300 randomly selected adult patients (100 patients with sepsis and 200 patients without sepsis) admitted to the emergency department of a large academic tertiary care hospital in Hamilton, ON, Canada. We collected data on demographics and a limited set of SDoH variables, including neighbourhood household income, smoking history, social support, and history of alcohol disorder. We analyzed study data using multivariate logistic regression models.
Results
The study included 100 patients with sepsis with a median [interquartile range (IQR)] age of 75 [58–84] yr and 200 patients without sepsis with a median [IQR] age of 72 [60–83] yr. Factors significantly associated with sepsis included arrival by ambulance, absence of a family physician, higher Hamilton Early Warning Score, and a recorded history of dyslipidemia. Important SDoH variables, such as individual or household income and race, were not available in the medical chart. In patients with SDoH available in their medical records, no SDoH was significantly associated with sepsis. Nevertheless, compared with their proportion of the Hamilton population, the rate of sepsis cases and sepsis deaths was approximately two times higher among patients living in systematically disadvantaged neighbourhoods.
Conclusions
This study revealed the lack of available SDoH data in electronic health records. Despite no association between the SDoH variables available and sepsis, we found a higher rate of sepsis cases and sepsis deaths among individuals living in systematically disadvantaged neighbourhoods. Including SDoH in electronic health records is crucial to study their effect on the risk of sepsis and to provide equitable care.
Résumé
Objectif
Nous avons cherché à déterminer si les déterminants sociaux de la santé (DSS) étaient associés à l’apparition de sepsis et à évaluer les différences entre les personnes vivant dans des quartiers systématiquement défavorisés et celles vivant à l’extérieur de ces quartiers.
Méthode
Nous avons mené une étude cas témoins monocentrique portant sur 300 patient·es adultes sélectionné·es au hasard (100 personnes atteintes de sepsis et 200 témoins sans sepsis) admis·es au service des urgences d’un grand hôpital universitaire de soins tertiaires à Hamilton, ON, Canada. Nous avons recueilli des données démographiques et un ensemble limité de variables de DSS, y compris le revenu des ménages du quartier, les antécédents de tabagisme, le soutien social et les antécédents de troubles liés à l’alcool. Nous avons analysé les données de l’étude à l’aide de modèles de régression logistique multivariés.
Résultats
L’étude a inclus 100 patient·es atteint·es de sepsis avec un âge médian [écart interquartile (ÉIQ)] de 75 [58-84] ans et 200 patient·es sans sepsis avec un âge médian [ÉIQ] de 72 [60-83] ans. Les facteurs significativement associés au sepsis comprenaient l’arrivée en ambulance, l’absence de médecin de famille, un score Hamilton Early Warning Score plus élevé et des antécédents enregistrés de dyslipidémie. D’importantes variables de DSS, telles que le revenu individuel et du ménage et la race, n’étaient pas disponibles dans le dossier médical. Chez les personnes dont les DSS étaient disponibles dans leur dossier médical, aucun DSS n’était significativement associé au sepsis. Néanmoins, comparativement à leur proportion dans la population de Hamilton, le taux de cas de sepsis et de décès dus au sepsis était environ deux fois plus élevé chez les personnes vivant dans des quartiers systématiquement défavorisés.
Conclusion
Cette étude a révélé le manque de données disponibles sur les DSS dans les dossiers de santé électroniques. Bien qu’il n’y ait pas d’association entre les variables disponibles et le sepsis, nous avons constaté un taux plus élevé de cas de sepsis et de décès dus à la septicémie chez les personnes vivant dans des quartiers systématiquement défavorisés. L’inclusion des DSS dans les dossiers de santé électroniques est cruciale pour étudier leur effet sur le risque de sepsis et pour dispenser des soins équitables.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Sepsis, defined as organ dysfunction because of a dysregulated host response to infection, is a significant cause of morbidity and mortality worldwide.1 In 2017, the worldwide incidence of sepsis was 48.9 million cases with 11 million sepsis-related deaths, representing approximately 20% of all global deaths.2 In Ontario alone, sepsis is associated with a higher long-term risk of death, rehospitalization, and an incremental one-year cost of one billion dollars to the Ontario health care system.3 Although early therapeutic intervention reduces sepsis morbidity and mortality, the heterogeneous presentation of the disease, combined with the lack of a gold standard diagnostic test for sepsis, makes early and accurate identification and treatment challenging.4,5 To address the significant impact of sepsis on human health and health care systems, strategies to prevent and detect sepsis early are needed.
The World Health Organization defines social determinants of health (SDoH) as “the conditions in which people are born, grow, work, live, and age, and the wider set of forces and systems shaping the conditions of daily life.”6 Although poverty has long been understood to be associated with poor health outcomes, a growing body of evidence suggests that social factors such as race, ethnicity, education, social status, and levels of social support, may also affect health.7 For example, data from the USA showed that avoidable factors associated with lower education accounted for almost half of all adult deaths in 2001. Similarly, the Code Red project, conducted in Hamilton, ON, Canada, has identified inequities in health outcomes that may be related to disparities in social and economic factors. Specifically, the project identified physically and socially disadvantaged neighbourhoods, referred to as the Code Red Zone, with significantly worse health outcomes, including a 21-year gap in average life expectancy, compared with other neighbourhoods in Hamilton.8 This shows that SDoH may play a significant role in impacting health outcomes of residents. Nevertheless, there is a lack of high-quality evidence that explores whether SDoH may affect the early incidence and outcomes of sepsis.
In a review investigating the association between SDoH and sepsis, we identified that socioeconomic status (SES), aging, frailty, gender, alcohol dependence, and social support showed an increased association with sepsis. Of the six studies that evaluated race, four revealed a higher incidence of sepsis in Black patients than in White patients, and two showed the opposite trend.9 Nevertheless, the review identified significant methodological heterogeneity between studies because of the investigated populations and the lack of consistent definitions used for SDoH and sepsis.9 To address these disparities and reduce the burden of sepsis on patients and the health care system, rigorous and high-quality evidence is needed to determine the association between SDoH and sepsis. The purpose of this study was to explore the effects of clinical and social factors on the development of sepsis. Specifically, we aimed to 1) identify whether SDoH, including residence in a Code Red Zone, affect sepsis development among patients presenting to the emergency department (ED); and 2) investigate differences in sepsis development and outcomes, based on Code Red residence, among ED admissions relative to the total population in Hamilton.
Methods
Study design
We conducted a case-control study of adults aged over 18 yr who presented to the ED of a large academic tertiary care hospital in Hamilton, ON, Canada, from January to June 2014. This study was a secondary analysis of a database including prospectively identified and consecutive ED patients admitted to medical and surgical units as part of the implementation of a local early warning score.10,11 Population estimates were calculated based on 2016 Canadian census data to reflect clinical data from patient health records. The results of this study were organized and reported according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) checklist.
Data collection
Data were abstracted in accordance with retrospective chart review methodology.12 First, a study protocol, a standardized operating procedure, and a detailed case report form were developed. Trained abstractors (F. S., W. D., Y. D., R. G., and C. M.) independently extracted data from patient health records. Interrater agreement was calculated using Cohen’s kappa statistic (\(\kappa\)) on a random sample of patients, completed independently and in duplicate (\(\kappa\) = 0.93). Disagreements between reviewers were resolved by discussion with the principal investigator (A. F.-R.).
Variables and measurement
Patients with sepsis, defined as patients with an infection and two of the three quick sequential organ failure assessment score criteria or a recorded diagnosis of sepsis, were identified from the prospectively collected data set. Controls without sepsis were collected in a 1:2 ratio.13
All variables, including demographic data, presenting symptoms, triage vitals, medical history, and SDoH data, were recorded at ED presentation. We selected variables based on the existing literature and their availability in health records. Demographic variables included age, birth-assigned sex, the first three digits (forward sortation area) of their postal code, and the median household income based on postal code region. Based on the 2010 Hamilton Code Red project, postal codes were further classified as being part of physically and socially disadvantaged neighbourhoods (Code Red neighbourhoods).8 Presenting symptoms, comorbidities and the patient’s medical history, were reported as either “present” or “absent” based on the patient’s health record. Additionally, the Charlson Comorbidity Index (CCI), which predicts one-year mortality based on a patient’s burden of comorbid disease,14 and the Hamilton Early Warning Score (HEWS), shown to predict the likelihood of a critical event,10,11 were calculated using the first complete set of vitals within the first 24 hr. We defined frailty as the presence of at least two of three frailty indicators (weakness, exhaustion, and/or low physical activity) or evidence of frailty from the patient’s history. Because of the limited availability of social history in health records, we categorized smoking status, and alcohol use (past or present) as binary variables (“yes” or “no”). We also collected registration with a family physician and the presence or absence of a diagnosis of mental illness.
Data were considered missing if they were not available in the health record or if the data needed to calculate the appropriate values were not available during the specified period. A complete list of variables and an explanation of how they were reported is available in Electronic Supplementary Material (ESM) eAppendix 1. All deidentified data were stored in REDCap® (Vanderbilt University, Nashville, TN, USA).
Data analysis
We report descriptive statistics as median [interquartile range (IQR)], counts, and proportions for patients with sepsis and patients without sepsis. We assessed differences in baseline characteristics between patients with sepsis and patients without sepsis using the Wilcoxon rank sum and Chi square tests, where appropriate. We used multivariable logistic regression to examine the association between clinical and social factors and sepsis. We used a stepwise procedure for model-building, in which variables of importance were individually added or removed according to their statistical significance, to identify a parsimonious subset of variables. We used this method given the limited literature, large number of potential predictor variables, and our intent to identify a subset of variables that may be meaningful with respect to our outcome.15 We reported data as unadjusted and adjusted odds ratios (OR and aOR, respectively) with the corresponding 95% confidence intervals (CIs) to show associations. Additionally, we compared participants’ postal code data with population data from the 2016 Canadian Census to determine the proportion of study participants in the Code Red Zone compared with the total Hamilton population, and reported this as rates per 100,000 people. Lastly, we conducted a sensitivity analysis on the subset of patients living in the Code Red Zone to identify any differences in our final model and interpretations. We defined statistical significance as P values < 0.05. Given our sample size, outcome incidence, and alpha of 0.05, our post hoc analysis suggested 99.9% power to detect differences between the study groups. We performed all analyses in SAS version 9.4 (SAS Institute Inc., Cary, NC, USA).
Ethics
We received ethics approval from the Hamilton Integrated Research Ethics Board, with a waiver of informed consent, prior to starting the study (Reference Number: 5061).
Results
Among the 7,156 patients included in the data set, we included 100 randomly selected patients with sepsis and 200 patients without sepsis in the study. Characteristics of the participants are described in Table 1. In patients with sepsis, the median [IQR] age was 75 [58–84] yr with 45% identifying as female, and in patients without sepsis, the median [IQR] age was 72 [60–83] yr with 55% identifying as female. There were significant differences in triage vitals, and HEWS between patients with sepsis and patients without sepsis. Eighty-five percent of patients with sepsis and 68% of patients without sepsis arrived by ambulance (P = 0.002), and 93% of patients with sepsis and 99% of patients without sepsis had a recorded family physician (P = 0.01). Both patients with sepsis and patients without sepsis had a median [IQR] CCI of 5 [4–8], showing a similar baseline burden of disease. There were significantly fewer reports of dyslipidemia in patients with sepsis than in patients without sepsis (with sepsis, 42%; without sepsis, 57%; P = 0.02).
Social determinants of health data, including neighbourhood household income, smoking history, social support, and history of alcohol disorders, were collected. Of the patients with sepsis and patients without sepsis, respectively, 66% were frail compared with 58% (P = 0.17). A history of mental illness was present in 34% of patients with sepsis compared with 27% of patients without sepsis (P = 0.21). A smoking history was present in 47% of patients with sepsis compared with 55% of patients without sepsis (P = 0.18). Seventy-five percent of patients with sepsis compared with 76% had some level of social support (P = 0.94) and 28% compared with 30% had a history of disordered alcohol use (P = 0.66). There were some missing data among patients with sepsis and patients without sepsis—particularly related to SDoH, including frailty, mental illness, smoking history, presence of social support, and alcohol disorder (ESM eAppendix 2). There were no significant differences in the presence of SDoH available in health records between patients with sepsis and patients without sepsis.
Unadjusted and adjusted odds ratios for clinical and social determinants are reported in Table 2. Univariate logistic regression analysis showed that arrival by ambulance (OR, 2.53; 95% CI, 1.35 to 4.73), and higher HEWS (OR, 1.33; 95% CI, 1.18 to 1.51) were significantly associated with increased odds of sepsis, while having a recorded family physician (OR, 0.21; 95% CI, 0.05 to 0.83) and dyslipidemia (OR, 0.55; 95% CI, 0.33 to 0.91) were significantly associated with decreased odds. Following the stepwise procedure for model building, the presence of a family physician and HEWS were included in the final multivariate logistic regression model, and HEWS remained statistically significant (aOR, 1.18; 95% CI, 1.02 to 1.36). None of the other clinical or social determinants investigated were significantly associated with sepsis (Table 2).
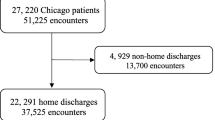
We conducted additional population-level analyses to compare the proportion of residents living in the Code Red Zone and presenting to the ED with sepsis, and the proportion of Hamilton residents living in the Code Red Zone. As of the 2016 Canadian census, only 17.9% of Hamilton residents lived within the Code Red Zone. Compared with their proportion of the total Hamilton population, Code Red residents comprised a disproportionate number of ED patients (32%) and ED patients admitted with sepsis (32%; Figure). Furthermore, there was an increased rate of sepsis (33.3 cases per 100,000 vs 15.4 cases per 100,000) and deaths from sepsis (8.3 deaths per 100,000 vs 4.5 deaths per 100,000) in patients living in the Code Red Zone compared with patients who were not living in the Code Red Zone (ESM eAppendix 3). Our sensitivity analysis did not yield any differences in the significance of associations for the subset of participants living in the Code Red Zone (ESM eAppendix 4).
Discussion
In this case-control study of adults who presented to the ED at a tertiary academic hospital, arrival by ambulance, absence of a family physician, a higher HEWS, and presence of dyslipidemia, were significantly associated with sepsis. Following adjustment, higher HEWS remained significantly associated with sepsis, confirming previous findings on the importance of vital signs at ED presentation in patients with an infection.11 In contrast, the SDoH available in health records were not significantly associated with sepsis. Despite this lack of association between SDoH and sepsis, our study highlighted that there were twice as many patients presenting to the ED with sepsis, and deaths from sepsis, among patients living in the Code Red Zone than among patients living outside of the Code Red Zone. Limited and inconsistent SDoH data available in health records may explain the lack of association between SDoH and the development of sepsis.
In a scoping review of SDoH and sepsis, studies evaluating SES, gender, smoking status, alcohol disorders, social support, age, and frailty all showed an association between the SDoH studied and sepsis.9 Four studies evaluating race showed a higher risk of sepsis among Black patients than among White patients, and two studies showed an increased risk among Black patients compared with White patients.9 Contrary to our hypothesis and the results of previous studies, SDoH, smoking status, social support, and alcohol disorders, were not significantly associated with sepsis. Individual or household income, race, and gender, as distinct from sex, were not available in health records and could not be studied.
These results can be explained by missing or unreported data in health records, a well-documented challenge when using electronic health records,16,17 and even more pronounced when integrating individual-level SDoH.18 For example, among critically ill patients, smoking and alcohol use are frequently underrecognized and underreported.19 Although studies have shown the contribution of individual-level SDoH to the prediction of 30-day readmission,20 HIV risk assessment,21 suicide attempts,22,23 and hospitalization, they have also highlighted the challenges of accurately collecting SDoH data. These challenges include the limited amount of SDoH data included in electronic health records, the difficulty in capturing accurate and complete data, and the lack of common measures or a minimum set of SDoH measures that should be recorded in a patient’s record.18 This emphasizes the need to collect and better integrate individual-level SDoH into health records to help guide and inform equitable care.
In addition to individual-level SDoH, neighbourhood-level SDoH including median household income were collected. The associations between median household income, residence in the Code Red Zone, and the incidence of sepsis were not significant. Other neighbourhood SES studies have shown an increased risk of microbiologically verified Staphylococcus aureus bacteremia,24 bloodstream infection,25 and higher rates of infection.26 Nevertheless, in line with our results, Donnelly et al. did not find an association between neighbourhood SES and the risk of sepsis at presentation among patients hospitalized with an infection.26 In addition to SES, residence in medically underserved areas (defined according to the ratio of primary care physicians per 1,000 people), infant mortality rate, the proportion of individuals with an income below the poverty line, and the percentage of the population over 65 yr of age, are also associated with a higher incidence of sepsis and higher rates of mortality due to sepsis.19 Although residence in the Code Red Zone was not significantly associated with sepsis, a disproportionate number of patients from the Code Red Zone were admitted from the ED to the hospital with sepsis, relative to the proportion of Hamilton residents living in the Code Red Zone. Similar to medically underserved areas, the Code Red project showed glaring disparities in social and economic factors, including ED visits, rates of cardiovascular incidents, respiratory emergencies, and, perhaps most concerning, a 21-yr difference in life expectancy between those living in and outside of the Code Red Zone.8,27 The increased number of patients presenting with sepsis from the Code Red Zone suggests that the incidence of sepsis may be affected by neighbourhood-level determinants, including access to care. These results may be transferable to other communities with similar structural challenges.
Arrival by ambulance and the absence of a family physician were also significantly associated with sepsis. Although the data in this study do not establish a causal mechanism between SDoH and sepsis, access to primary care and early detection and treatment of infections can limit sepsis cases. In this study, the median CCI value was the same for patients with sepsis and patients without sepsis, albeit CCI is only a measure of the number of comorbidities and does not account for how the conditions are managed. Access to primary care and a designated family physician can improve the management of chronic comorbidities and decrease the risk of developing sepsis.28 Therefore, access to care, as shown in our study and corroborated by the Code Red project8 and existing literature,29 is an important determinant for further studies. This includes understanding how structural determinants impact health literacy, for example, and delays in accessing care.
This study has limitations. First, this was a retrospective chart review of existing data, not originally collected for research purposes. Although efforts were made to ensure the quality and rigour of the data extracted, including extracting data independently and in duplicate, considerable challenges remained in collecting accurate and complete SDoH data. Second, in addition to quality issues and missing data, the limited amount of SDoH data available in health records prevented the analysis of other determinants, including individual household income and race. Lastly, this was a single-centre study of patients admitted to the ED of a large academic tertiary care hospital in Hamilton and was limited by sample size. It is not clear whether the results of this study can be generalized to other health care settings. Future prospective studies are needed to address data quality issues and the limited SDoH available in health records. This includes going beyond SDoH data inputted by health care workers and including self-reported measures such as race and ethnicity, among other self-reported SDoH.
Nevertheless, this study highlights the importance of adding of SDoH data into electronic health records and its implications for the future of sepsis research. Importantly, this work exposed the current challenges of integrating SDoH into health records, a crucial element to ensure equitable care and to inform health care policy.
Conclusions
Our study highlights both the limited set of SDoH data collected in health records and the challenges of collecting accurate and complete SDoH data. Furthermore, it emphasizes the importance of integrating individual-level SDoH in health records to inform early interventions and downstream care. Given the significant burden of sepsis and the growing body of evidence showing the utility of SDoH, integrating self-reported SDoH into electronic health records is necessary to inform programs and policies for populations disproportionately affected by adverse health outcomes and to guide research and clinical care based on identified inequities and patient needs.
References
Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 2016; 315: 801–10. https://doi.org/10.1001/jama.2016.0287
Rudd KE, Johnson SC, Agesa KM, et al. Global, regional, and national sepsis incidence and mortality, 1990–2017: analysis for the Global Burden of Disease Study. Lancet 2020; 395: 200–11. https://doi.org/10.1016/s0140-6736(19)32989-7
Farrah K, McIntyre L, Doig CJ, et al. Sepsis-associated mortality, resource use, and healthcare costs: a propensity-matched cohort study. Crit Care Med 2021; 49: 215–27. https://doi.org/10.1097/ccm.0000000000004777
Evans L, Rhodes A, Alhazzani W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Intensive Care Med 2021; 47: 1181–247. https://doi.org/10.1097/ccm.0000000000005337
Leligdowicz A, Matthay MA. Heterogeneity in sepsis: new biological evidence with clinical applications. Crit Care 2019; 23: 80. https://doi.org/10.1186/s13054-019-2372-2
World Health Organizaiton. Social determinants of health; 2022. Available from URL: https://www.who.int/westernpacific/health-topics/social-determinants-of-health (accessed April 2024).
Braveman P, Gottlieb L. The social determinants of health: it’s time to consider the causes of the causes. Public Health Rep 2014; 129: 19–31. https://doi.org/10.1177/00333549141291s206
Buist S. Code red part 1: worlds apart; 2010. Available from URL: https://www.thespec.com/news/hamilton-region/code-red/2022/09/20/worlds-apart.html (accessed April 2024).
Sheikh F, Douglas W, Catenacci V, Machon C, Fox-Robichaud AE. Social determinants of health associated with the development of sepsis in adults: a scoping review. Crit Care Explor 2022; 4: e0731. https://doi.org/10.1097/cce.0000000000000731
Tam B, Xu M, Kwong M, Wardell C, Kwong A, Fox-Robichaud A. The admission Hamilton Early Warning Score (HEWS) predicts the risk of critical event during hospitalization. Can J Gen Intern Med 2016; 11: 24–7. https://doi.org/10.22374/cjgim.v11i4.190
Skitch S, Tam B, Xu M, McInnis L, Vu A, Fox-Robichaud A. Examining the utility of the Hamilton early warning scores (HEWS) at triage: retrospective pilot study in a Canadian emergency department. CJME 2018; 20: 266–74. https://doi.org/10.1017/cem.2017.21
Gearing RE, Mian IA, Barber J, Ickowicz A. A methodology for conducting retrospective chart review research in child and adolescent psychiatry. J Can Acad Child Adolesc Psychiatry 2006; 15: 126–34.
Tenny S, Kerndt CC, Hoffman MR. Case Control Studies. Treasure Island: StatPearls Publishing; 2017.
Needham DM, Scales DC, Laupacis A, Pronovost PJ. A systematic review of the Charlson comorbidity index using Canadian administrative databases: a perspective on risk adjustment in critical care research. J Crit Care 2005; 20: 12–9. https://doi.org/10.1016/j.jcrc.2004.09.007
Thayer JD. Stepwise regression as an exploratory data analysis procedure; 2002. Available from URL: https://eric.ed.gov/?id=ED464932 (accessed April 2024).
Wells BJ, Chagin KM, Nowacki AS, Kattan MW. Strategies for handling missing data in electronic health record derived data. EGEMS (Wash DC) 2013; 1: 1035. https://doi.org/10.13063/2327-9214.1035
Madden JM, Lakoma MD, Rusinak D, Lu CY, Soumerai SB. Missing clinical and behavioral health data in a large electronic health record (EHR) system. J Am Med Inform Assoc 2016; 23: 1143–9. https://doi.org/10.1093/jamia/ocw021
Chen M, Tan X, Padman R. Social determinants of health in electronic health records and their impact on analysis and risk prediction: a systematic review. J Am Med Inform Assoc 2020; 27: 1764–73. https://doi.org/10.1093/jamia/ocaa143
Goodwin AJ, Nadig NR, McElligott JT, Simpson KN, Ford DW. Where you live matters: the impact of place of residence on severe sepsis incidence and mortality. Chest 2016; 150: 829–36. https://doi.org/10.1016/j.chest.2016.07.004
Nijhawan AE, Metsch LR, Zhang S, et al. Clinical and sociobehavioral prediction model of 30-day hospital readmissions among people with HIV and substance use disorder: beyond electronic health record data. J Acquir Immune Defic Syndr 2019; 80: 330–41. https://doi.org/10.1097/qai.0000000000001925
Feller DJ, Zucker J, Yin MT, Gordon P, Elhadad N. Using clinical notes and natural language processing for automated HIV risk assessment. J Acquir Immune Defic Syndr 2018; 77: 160–6. https://doi.org/10.1097/qai.0000000000001580
Zheng L, Wang O, Hao S, et al. Development of an early-warning system for high-risk patients for suicide attempt using deep learning and electronic health records. Transl Psychiatry 2020; 10: 72. https://doi.org/10.1038/s41398-020-0684-2
Walsh CG, Ribeiro JD, Franklin JC. Predicting suicide attempts in adolescents with longitudinal clinical data and machine learning. J Child Psychol Psychiatry 2018; 59: 1261–70. https://doi.org/10.1111/jcpp.12916
Oestergaard LB, Schmiegelow MD, Bruun NE, et al. The associations between socioeconomic status and risk of Staphylococcus aureus bacteremia and subsequent endocarditis – a Danish nationwide cohort study. BMC Infect Dis 2017; 17: 589. https://doi.org/10.1186/s12879-017-2691-3
Mendu ML, Zager S, Gibbons FK, Christopher KB. Relationship between neighborhood poverty rate and bloodstream infections in the critically ill. Crit Care Med 2012; 40: 1427–36. https://doi.org/10.1097/ccm.0b013e318241e51e
Donnelly JP, Lakkur S, Judd SE, et al. Association of neighborhood socioeconomic status with risk of infection and sepsis. Clin Infect Dis 2018; 66: 1940–7. https://doi.org/10.1093/cid/cix1109
Buist S. Ten years later part 1: “a five-alarm fire”; 2019. Available from URL: https://www.thespec.com/news/hamilton-region/code-red/2022/10/04/code-red-ten-years-later-part-1.html (accessed April 2024).
Wang HE, Shapiro NI, Griffin R, Safford MM, Judd S, Howard G. Chronic medical conditions and risk of sepsis. PLoS One 2012; 7: e48307. https://doi.org/10.1371/journal.pone.0048307
Peel A, Gutmanis I, Bon T. Disparities in health outcomes among seniors without a family physician in the North West Local Health Integration Network: a retrospective cohort study. CMAJ Open 2019; 7: E94–100. https://doi.org/10.9778/cmajo.20180004
Author contributions
Fatima Sheikh contributed to all aspects of this manuscript, including study conception and design; acquisition, analysis, and interpretation of data; and drafting the article. Alison E. Fox-Robichaud, William Douglas, Rachel Gregoris, and Christina Machon contributed to the conception and design of the study. William Douglas, Yi (David) Diao, Rachel Gregoris, and Christina Machon contributed to the acquisition of the data. William Douglas, Rebecca H. Correia, and Neil Johnston contributed to the analysis and interpretation of the data. All authors provided feedback throughout and reviewed a draft of the manuscript.
Acknowledgments
We would like to thank Drs Allison Williams and Gloria Vasquez Grande for their detailed review and feedback of this manuscript and Sana Hamideh for helping with the Figure.
Disclosures
Alison Fox-Robichaud is the Scientific Director of Sepsis Canada, a CIHR-funded network. The other authors have no conflicts of interest to declare.
Funding statement
This research did not receive a specific grant from any funding agency in the public, commercial, or nonprofit sectors.
Prior conference presentations
The abstract of this study was presented at the 2023 Critical Care Canada Forum (28 November to 1 December, Toronto, ON, Canada).
Editorial responsibility
This submission was handled by Dr. Patricia S. Fontela, Associate Editor, Canadian Journal of Anesthesia/Journal canadien d’anesthésie.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Sheikh, F., Douglas, W., Diao, Y. et al. Social determinants of health and sepsis: a case-control study. Can J Anesth/J Can Anesth (2024). https://doi.org/10.1007/s12630-024-02790-6
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12630-024-02790-6