Abstract
Purpose
The management of patients with an anticipated difficult airway remains challenging. We evaluated laryngeal visualization with the recently introduced Vie Scope® as a straight blade laryngoscope consisting of an illuminated tube necessitating bougie-facilitated intubation vs Macintosh videolaryngoscopy.
Methods
We conducted a prospective randomized controlled noninferiority trial. Patients undergoing elective ear, nose, and throat or oral and maxillofacial surgery with an anticipated difficult airway were randomized 1:1 to receive tracheal intubation with the Vie Scope or Macintosh videolaryngoscope (C-MAC®). The primary outcome measure was laryngeal visualization by the percentage of glottis opening (POGO) scale. Secondary outcome measures were the time to successful intubation (TTI) and first-attempt and overall success rates.
Results
We included two sets of 29 patients in our analysis. For visualization, the Vie Scope was noninferior to videolaryngoscopy (VL) with mean (standard deviation [SD]) POGO scores of 71 (31)% vs 64 (30)% in the VL group [difference in means, 7 (8)%; 95% confidence interval, –9 to 23; P = 0.38]. Mean (SD) TTI was 125 (129) sec in the Vie Scope and 51 (36) sec in the VL group (difference in means, 75 sec; 95% confidence interval, 25 to 124; P = 0.005). The first-attempt and overall success rates were 22/29 (76%) and 27/29 (93%) in both groups. Two patients per group were switched to a different device. Four accidental esophageal intubations occurred in the Vie Scope group, these were presumably due to bougie misplacement.
Conclusion
Visualization with the Vie Scope was noninferior to VL in patients with an anticipated difficult airway, but TTI was longer in the Vie Scope group.
Study registration
ClinicalTrials.gov (NCT05044416); registered 5 September 2021.
Résumé
Objectif
La prise en charge des patients dont les voies aériennes sont anticipées comme étant difficiles demeure un défi. Nous avons évalué la visualisation laryngée obtenue avec le nouveau Vie Scope®, un laryngoscope à lame droite constitué d’un tube éclairé nécessitant une intubation facilitée par bougie, par rapport à celle obtenue avec un vidéolaryngoscope Macintosh.
Méthode
Nous avons réalisé une étude randomisée contrôlée prospective de non-infériorité. Les patient·es bénéficiant d’une chirurgie non urgente des oreilles, du nez et de la gorge ou une chirurgie buccale et maxillo-faciale présentant des voies aériennes anticipées comme difficiles ont été randomisé·es à un ratio 1:1 à recevoir une intubation trachéale avec un laryngoscope Vie Scope ou un vidéolaryngoscope Macintosh (C-MAC®). Le critère d’évaluation principal était la visualisation laryngée selon l’échelle de pourcentage d’ouverture de la glotte (POGO). Les critères d’évaluation secondaires étaient le délai avant une intubation réussie et les taux de réussite de la première tentative et globaux.
Résultats
Nous avons inclus deux groupes de 29 patient·es dans notre analyse. En matière de visualisation, le Vie Scope n’était pas inférieur à la vidéolaryngoscopie (VL), avec des scores POGO moyens (écart type [ET]) de 71 (31) % vs 64 (30) % dans le groupe VL [différence dans les moyennes, 7 (8) %; intervalle de confiance à 95 %, –9 à 23; P = 0,38]. Le délai moyen (ET) avant une intubation réussie était de 125 (129) sec avec le Vie Scope et de 51 (36) secondes dans le groupe VL (différence dans les moyennes, 75 sec; intervalle de confiance à 95 %, 25 à 124; P = 0,005). Les taux de réussite de la première tentative et de réussite globale étaient de 22/29 (76 %) et 27/29 (93 %) dans les deux groupes. Un dispositif différent a dû être utilisé chez deux patient·es par groupe. Quatre intubations œsophagiennes accidentelles sont survenues dans le groupe Vie Scope; celles-ci étaient probablement dues à un mauvais placement de la bougie.
Conclusion
La visualisation obtenue avec le Vie Scope n’était pas inférieure à la vidéolaryngoscopie chez les patient·es dont les voies aériennes étaient anticipées comme difficiles, mais le délai avant une intubation réussie était plus long dans le groupe Vie Scope.
Enregistrement de l’étude
ClinicalTrials.gov (NCT05044416); registered 5 September 2021.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Tracheal intubation is required for different surgical procedures for mechanical ventilation and prevention of aspiration. Nevertheless, many patients present with a difficult airway not manageable by direct laryngoscopy and may require other techniques for airway management.1 For cases in which the difficult airway is anticipated before induction of anesthesia, awake tracheal intubation is regarded as the gold standard, but not all cases may require tracheal intubation with this technique and graduated approaches including management by videolaryngoscopy (VL) after the induction of general anesthesia have been recommended.2,3 Furthermore, the vast majority of difficult airways are unexpected.4 Nevertheless, airway management in patients with anticipated difficult airways remains a challenge and a high rate of difficult tracheal intubations has to be expected, particularly in patients scheduled for ear, nose, and throat (ENT) or oral and maxillofacial (OMF) surgery.5 Most frequently, VL is used for tracheal intubation in these patients.
Recently, a new type of laryngoscope was introduced consisting of an illuminated straight closed circular tube with a bevelled end for laryngoscopy, allowing for a two-step approach to intubation via a bougie (Vie Scope®; Adroit Surgical LLC, Oklahoma City, OK, USA)6 (Fig. 1). The Vie Scope is inspired by the principle of anterior commissure scopes that are traditionally used by ENT surgeons for the purpose of microsurgery but have also been used as rescue devices in difficult or failed tracheal intubation and follow the principle of a straight blade technique by directly lifting the epiglottis. Nevertheless, it is still unclear if a similarly designed, single-use device can be equally useful in the hands of non-ENT practitioners for routine or difficult airway management.7
So far, the Vie Scope has been shown to improve visualization over conventional direct laryngoscopy in intubations without a difficult airway, although time to intubation was longer.8,9 Furthermore, the Vie Scope was associated with higher first-attempt success rates over conventional Macintosh laryngoscopy in a prehospital setting.10 It has been claimed that the Vie Scope might be particularly useful in emergency situations in patients with difficult airways because it is easy-to-use and facilitates a good glottis view, which is an important prerequisite for successful intubation. Nevertheless, until now, no data are available in patients with an expected difficult airway. We hypothesized that visualization of the larynx, quantified by the percentage of glottis opening (POGO), with the Vie Scope is noninferior to a Macintosh videolaryngoscope in patients with an expected difficult airway undergoing ENT or OMF surgery.
Methods
Ethics
The study was approved by the Ethics Committee of the Hamburg Chamber of Physicians (2020-10238-BO-ff, original approval: 21 December 2020, amendment for expected difficult airways: 12 August 2021; chairman, Prof. Dr. Stahl). All patients provided written informed consent. The study was registered prior to patient enrolment on ClinicalTrials.gov (NCT05044416) on 5 September 2021 and was conducted in accordance with the Declaration of Helsinki. The reporting of study adheres to the applicable CONSORT guidelines.
Study design
The VieScOP-2 trial was a prospective randomized noninferiority investigator-initiated study with a 1:1 allocation ratio to either Vie Scope or VL. Patients were blinded to the study intervention.
Setting and participants
The study was conducted at the Center for Anesthesiology and Intensive Care Medicine of the University Medical Center Hamburg-Eppendorf, Germany.
Eligibility
Patients were eligible if they were at least 18 yr old, required transoral tracheal intubation for elective otorhinolaryngologic or OMF surgery, and had an expected difficult airway. All patients underwent a structured airway assessment in our pre-op clinic that included clinical history (for instance, radiotherapy, head and neck tumours, or difficult tracheal intubation), a physical examination such as the upper lip bite test (ULBT), the Wilson score, and the simplified airway risk index (SARI).11,12,13 Only patients with indicators for difficult tracheal intubation, such as a SARI ≥ 4 points, Wilson score ≥ 2 points, a positive ULBT, relevant pharyngolaryngeal lesions, reported previous difficult tracheal intubations (e.g., anesthesia alert card or a videolaryngoscopic intubation and difficult airway classification [VIDIAC] score ≥ 2), or a combination of these factors were considered eligible for study inclusion.5,11,13,14,15,16 Furthermore, patients were checked for indicators for awake tracheal intubation using a previously recommended decision-making tool taking predictors for difficult tracheal intubation, suspected difficult facemask and/or supraglottic-airway ventilation, physiologic issues such as apnea intolerance, risk for aspiration and hemodynamic instability, and contextual issues into account.2 Patients that qualified for awake tracheal intubation or required a nasotracheal intubation, special tubes such as laser or microlaryngoscopy tubes, rapid-sequence induction, or had loose teeth were excluded.
Participating physicians
All participating physicians were consultant anesthetists experienced in the management of difficult airways. Most physicians had participated in a prior Vie Scope trial and were familiar with the device. Furthermore, physicians attended a structured manikin airway training to practice paraglossal approaches with the Vie Scope. The years of physicians’ work experience were assessed in a questionnaire.
Interventions
Patients randomized to the intervention group received laryngoscopy and consecutive intubation with the Vie Scope. Midline and paraglossal approaches for optimal visualization of the larynx were permitted. Participating anesthetists were instructed to directly lift the epiglottis with the Vie Scope, as this is the designated technique with the Vie Scope (anterior commissure scopes, straight blade technique). After visualization of the larynx, a straight tip bougie (Tactical Bougie®, Adroit Surgical LLC, Oklahoma City, OK, USA) was advanced into the trachea up to the green marking indicating correct insertion depth. The Vie Scope was withdrawn, and the tracheal tube placed over the bougie and advanced into the trachea without any soft tissue retraction by a laryngoscope. After intubation, the Vie Scope was discarded as a single-use device.
Patients randomized into the control group received VL (C-MAC® video laryngoscope, Karl Storz SE & Co. KG, Tuttlingen, Germany) with a Macintosh type size 3 or 4 blade in a single-stage intubation approach. Participating anesthetists were instructed to indirectly lift the epiglottis with the Macintosh videolaryngoscope by placing the tip in the vallecula (point pressure on the hypoepiglottic ligament) as previously described while direct lifting was only allowed as a rescue maneuver.5,17
In both groups, the tube size was chosen at the discretion of the attending anesthetist. Per protocol, all participating anesthetists were instructed to obtain the best possible glottic view with either device while suboptimal laryngoscopy attempts were not allowed. Stylets, introducers, or forceps as well as airway optimization maneuvers such as backward upward rightward pressure or optimum external laryngeal manipulation could be used to optimize the glottic view. The glottic view (POGO and Cormack–Lehane) ratings were obtained by direct view (Vie Scope) or indirect view (videolaryngoscope: camera view displayed on the VL monitor). Propofol and sufentanil or remifentanil were used for anesthesia induction, and rocuronium or mivacurium for neuromuscular paralysis. Face mask ventilation between attempts was left at the discretion of the attending anesthetist. To avoid bias, randomization was performed after the anesthetist had been assigned to the patient and had specified tube and blade size in cases of VL.
Outcome parameters
The primary outcome measure was the visualization of the larynx assessed by POGO during laryngoscopy (between the anterior commissure to the interarytenoid notch).18 The POGO was assessed by the airway operator. Secondary outcome measures were the first-attempt and overall success rates, time to successful intubation (TTI), TTI with one attempt, time to bougie placement, time to bougie placement with one attempt, time to best view with one attempt, total and average number of attempts, grade according to Cormack–Lehane,5,19 end-tidal carbon dioxide concentration (etCO2) after intubation, vomiting or aspiration during intubation, esophageal intubation, hypoxia defined as a pulsoximetric saturation below 80%, hypotension defined as a systolic blood pressure below 70 mm Hg, and intubation difficulty rated with a visual analogue scale (0–100, lower values better).
A maximum of three attempts was permitted with the allocated method. After three attempts the method was rated as a failure and further attempts had to be conducted with a different method at the discretion of the attending anesthetist, e.g., change to a hyperangulated videolaryngoscope blade or fibreoptic intubation. Time to successful intubation was measured from Vie Scope or laryngoscope blade tip passing the teeth to the first of at least three positive, nondeclining end-tidal carbon dioxide readings.
Sample size
Based on a mean (standard deviation [SD]) POGO score of 90 (20)% for VL in an artificial difficult airway,20 a noninferiority margin of 15%, and an add-on of 10% for a possible nonnormal distribution, two sets of 29 patients were required with errors of α = 0.05 and β = 0.2 to show noninferiority for the intervention method. The sample size calculation was based on a t test.
Randomization and allocation
Patients were randomized 1:1 to the intervention and the control group. Randomization and allocation took place in the operating room immediately before anesthesia induction and after the anesthetist had been assigned to the patient. The randomization codes were contained in sealed opaque and numbered envelopes. Because of the nature of the study, the airway operator could not be blinded. Nevertheless, the patient was blinded to the intervention.
Statistics
Statistical analyses were performed using IBM SPSS for Windows version 27 (IBM Corp., Armonk, NY, USA). For the analyses of continuous parameters, we used Welch or t tests depending on equality of variances as assessed by Levene’s test. Two by two contingency tables were analyzed by Fisher’s exact tests and larger contingency tables by Pearson’s Chi square tests. We regarded two-tailed P values < 0.05 as statistically significant. Data are given as mean (SD). Mean differences between groups are given with 95% confidence intervals (CIs).
Results
From 11 September 2021 to 26 June 2022, 58 patients were randomly assigned to intubation facilitated by the Vie Scope or by Macintosh VL. An overview on patient inclusion is given in Fig. 2 and the patients’ characteristics are depicted in Table 1. The raw outcome data are available in the eAppendix.
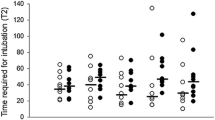
The mean (SD) POGO scores as the primary outcome measure were 71 (31)% in the Vie Scope vs 64 (30)% in the VL group (difference in means, 7%; 95% CI, –9 to 23; P = 0.38), fulfilling the noninferiority criteria for the Vie Scope over VL. The mean (SD) TTI was 125 (129) sec in the Vie Scope group and 51 (36) sec in the VL group (difference in means, 75 sec; 95% CI, 25 to 124; P = 0.005) and 63 (40) sec vs 39 (24) sec (difference in means, 24 sec; 95% CI, 4 to 44; P = 0.02) in cases with successful intubation on the first attempt. An overview of outcome parameters is shown in Table 2. The TTI and time to best view in cases of successful first-attempt intubation are depicted in Fig. 3. In both groups, two of 29 cases each were unsuccessful with the allocated method. In the Vie Scope group, one case was managed with Macintosh VL and one with hyperangulated VL (C-MAC D-BLADE; Karl Storz SE & Co. KG, Tuttlingen, Germany). In the VL group, both cases were managed with hyperangulated VL.
All participating anesthetists were specialists with a mean (SD) professional experience of 17 (6) yr in the Vie Scope group vs 17 (5) yr in the control group (difference in means, 0 yr; 95% CI, –3 to 3; P = 0.96).
Discussion
We studied laryngeal visualization with the Vie Scope in patients with an expected difficult airway and found a noninferior visualization of the larynx with the Vie Scope compared with Macintosh VL. Nevertheless, TTI was longer with the Vie Scope while the first-attempt success rates were similar between groups.
Excluding simulation-based studies, only two trials have evaluated the use of the Vie Scope for intubation in vivo. Neither of the studies included patients with an expected difficult airway. Szarpak et al. studied the preclinical use of the Vie Scope by paramedics.10 The POGO scores in the Vie Scope group were higher, and the first-attempt success rate for the Vie Scope was above 90% and only 51% for Macintosh laryngoscopy. Time to successful intubation as measured from “the laryngoscope touches the patient” to cuff-inflation was faster in the Vie Scope group at 49 sec. The second study was conducted by our working group and included patients receiving anesthesia with intubation for elective ENT and OMF surgery without anticipated difficult airways performed by experienced anesthetists.9 In that study, the POGO scores were significantly higher in the Vie Scope group than in the group with direct laryngoscopy with a Macintosh laryngoscope (86% vs 68%), and the first-attempt success rates were similar between the groups at around 85%; however, TTI was longer in the Vie Scope group.
In our present study, laryngoscopy with the Vie Scope showed similar POGO scores compared with VL. Laryngeal visualization with the Vie Scope is obtained through the illuminated tube shielding the line of sight from secretions. Concerning the technique, the Vie Scope resembles a straight blade anterior commissural laryngoscope with an improvement over blades (e.g., Miller blades) that do not provide shielding from secretions. Furthermore, the Vie Scope’s tube design might be helpful to control soft tissues. Particularly for Miller blades, several studies have shown improved visualization compared with curved Macintosh laryngoscope blades.21,22,23 Correct alignment of the oral, pharyngeal, and laryngeal axes to obtain an adequate direct view of the larynx is an important prerequisite for both techniques. In VL, the visualization axis is primarily defined by the angulation of the blade’s tip with the included camera and correct alignment of the direct view axis becomes less important with increasing angulation of the blade, particularly with hyperangulated blades that provide an angle of approximately 60°. It has been shown that different videolaryngoscopes perform differently in difficult airways20 and that hyperangulated blades may further improve laryngeal views.24,25 Nevertheless, our study compared the Vie Scope as a straight blade laryngoscope to VL with Macintosh blades angulated at approximately 30°. An important difference between the Vie Scope and Macintosh laryngoscopy is the direct lifting of the glottis, which might contribute to a better view with the straight blade technique.26 With the Macintosh approach, an incompletely lifted epiglottis (e.g., impaired epiglottis movement) acts like a shield in this view axis that restricts the view of the glottis.5 Thus, direct lifting of the epiglottis might be advantageous in this situation to improve glottis exposure.26
Previously, it has been shown that visualization was better with the Vie Scope over conventional laryngoscopy,9 so POGO was chosen as a primary outcome measure. Although of importance for the placement of tracheal tubes, successful visualization of the larynx does not necessarily translate into successful intubation. Tube advancement via the bougie through the laryngeal inlet is not visualized in Vie Scope-facilitated intubations, while tube advancement is performed under visual control with VL. In our Vie Scope group, time to successful insertion of the bougie was short compared with the overall TTI, indicating that the main challenge was to advance the tube into the trachea. As we have discussed elsewhere9 the tube may impinge on the arytenoid cartilages upon advancement and rotation maneuvers are required to allow for successful intubation of the trachea.27 These maneuvers may be time-consuming and explain the longer TTI in our Vie Scope group; but in elective tracheal intubation, no relevant impact on oxygenation or carbon dioxide level could be shown.28
In cases with low POGO values, the inability to visually follow the final entry of the bougie into the trachea through the Vie Scope tube may explain the four cases in the Vie Scope group where the bougie was misplaced and an accidental esophageal intubation occurred and a second attempt of correct bougie placement was required. A second or third intubation attempt was required in the VL group in six cases; however, no tracheal tube was placed in the esophagus in this group.
The use of any device on a patient requires sufficient experience and success rates increase in the sense of a learning curve. For tracheal intubation facilitated by direct laryngoscopy, at least 50 intubations are required to reach a plateau on the learning curve.29 Nevertheless, some clinical30 and mannequin studies31 have shown far steeper learning curves for videolaryngoscopic devices. No learning curves for the Vie Scope have been defined because only few data are available.6,10 To exclude any effect of a potential learning curve, physicians taking part in the present study were experienced anesthetists who had previously attended structured airway training sessions using the Vie Scope and all but one had taken part in a prior study evaluating the Vie Scope.9
Concerning visualization and intubation difficulty as subjectively assessed by a visual analogue scale, no difference between the groups was detected.
Our study has certain limitations. Because of the study design, operator blinding was not feasible. The POGO as the primary outcome measure was assessed by the airway operator, which may have introduced a bias. Furthermore, difficulty of intubation was also assessed by the operator, which may be influenced by experience using the respective devices. By using POGO as the primary outcome measure, we only evaluated the glottis visualization, while other steps of the tracheal intubation such as tube placement, intubation success, and intubation time were only secondary outcome parameters. We may have excluded the most difficult airways from this study in favour of management by awake fiberoptic intubation as gold standard. Nevertheless, this is the first study to systematically evaluate the Vie Scope in expected difficult airways.
Conclusion
Laryngoscopy and intubation are feasible with the Vie Scope in patients with an expectation for a difficult airway. Laryngeal visualization with the Vie Scope was noninferior to Macintosh VL. Nevertheless, TTI was longer in the Vie Scope group. No difference existed in the first-attempt success rates. According to our data, the Vie Scope might offer a new option for the management of difficult airways in a clinical setting, but limitations such as longer TTI have to be considered. Furthermore, we deem proper training in the use of straight blade devices mandatory before using the Vie Scope for this indication.
References
Cook TM, MacDougall-Davis SR. Complications and failure of airway management. Br J Anaesth 2012; 109: i68–85. https://doi.org/10.1093/bja/aes393
Law JA, Duggan LV, Asselin M, et al. Canadian Airway Focus Group updated consensus-based recommendations for management of the difficult airway: part 2. Planning and implementing safe management of the patient with an anticipated difficult airway. Can J Anesth 2021; 68: 1405–36. https://doi.org/10.1007/s12630-021-02008-z
Ahmad I, El-Boghdadly K, Bhagrath R, et al. Difficult Airway Society guidelines for awake tracheal intubation (ATI) in adults. Anaesthesia 2020; 75: 509–28. https://doi.org/10.1111/anae.14904
Nørskov AK, Rosenstock CV, Wetterslev J, Astrup G, Afshari A, Lundstrøm LH. Diagnostic accuracy of anaesthesiologists' prediction of difficult airway management in daily clinical practice: a cohort study of 188 064 patients registered in the Danish Anaesthesia Database. Anaesthesia 2015; 70: 272–81. https://doi.org/10.1111/anae.12955
Kohse EK, Siebert HK, Sasu PB, et al. A model to predict difficult airway alerts after videolaryngoscopy in adults with anticipated difficult airways - the VIDIAC score. Anaesthesia 2022; 77: 1089–96. https://doi.org/10.1111/anae.15841
Maslanka M, Szarpak L, Ahuja S, Ruetzler K, Smereka J. Novel airway device Vie Scope in several pediatric airway scenario: a randomized simulation pilot trial. Medicine (Baltimore) 2020; 99: e21084. https://doi.org/10.1097/md.0000000000021084
Khan SM, Cooper RM. Superior glottic views with the GlideScope® and Airtraq® laryngoscopes compared with an anterior commissure laryngoscope. Can J Anesth 2011; 58: 224–5. https://doi.org/10.1007/s12630-010-9413-2
Ecker H, Kolvenbach S, Stranz S, Herff H, Wetsch WA. Comparison of the novel Vie Scope® with conventional and video laryngoscope in a difficult airway scenario - a randomized, controlled simulation trial. BMC Emerg Med 2021; 21: 90. https://doi.org/10.1186/s12873-021-00484-6
Petzoldt M, Engels Y, Popal Z, et al. Elective tracheal intubation with the Vie Scope®-A prospective randomized non-inferiority pilot study (VieScOP-Trial). Front Med (Lausanne) 2022; 9: 820847. https://doi.org/10.3389/fmed.2022.820847
Szarpak L, Peacock FW, Rafique Z, et al. Comparison of Vie Scope® and Macintosh laryngoscopes for intubation during resuscitation by paramedics wearing personal protective equipment. Am J Emerg Med 2022; 53: 122–6. https://doi.org/10.1016/j.ajem.2021.12.069
Detsky ME, Jivraj N, Adhikari NK, et al. Will this patient be difficult to intubate?: the rational clinical examination systematic review. JAMA 2019; 321: 493–503. https://doi.org/10.1001/jama.2018.21413
el-Ganzouri AR, McCarthy RJ, Tuman KJ, Tanck EN, Ivankovich AD. Preoperative airway assessment: predictive value of a multivariate risk index. Anesth Analg 1996; 82: 1197–204. https://doi.org/10.1097/00000539-199606000-00017
Roth D, Pace NL, Lee A, et al. Airway physical examination tests for detection of difficult airway management in apparently normal adult patients. Cochrane Database Syst Rev 2018; 5: CD008874. https://doi.org/10.1002/14651858.cd008874.pub2
Sasu PB, Pansa JI, Stadlhofer R, et al. Nasendoscopy to predict difficult videolaryngoscopy: a multivariable model development study. J Clin Med 2023; 12(10): 3433
Lundstrøm LH, Møller AM, Rosenstock C, et al. A documented previous difficult tracheal intubation as a prognostic test for a subsequent difficult tracheal intubation in adults. Anaesthesia 2009; 64: 1081–8. https://doi.org/10.1111/j.1365-2044.2009.06057.x
Barclay-Steuart A, Großhenning H, Sasu PB, et al. Transnasal videoendoscopy for preoperative airway risk stratification - development and validation of a multivariable risk prediction model. Anesth Analg 2023; 136: 1164–73
Macintosh RR. A new laryngoscope. Lancet 1943; 241: 205. https://doi.org/10.1016/S0140-6736(00)89390-3
Levitan RM, Ochroch EA, Kush S, Shofer FS, Hollander JE. Assessment of airway visualization: validation of the percentage of glottic opening (POGO) scale. Acad Emerg Med 1998; 5: 919–23. https://doi.org/10.1111/j.1553-2712.1998.tb02823.x
Cormack RS, Lehane J. Difficult tracheal intubation in obstetrics. Anaesthesia 1984; 39: 1105–11.
Kleine-Brueggeney M, Greif R, Schoettker P, Savoldelli GL, Nabecker S, Theiler LG. Evaluation of six videolaryngoscopes in 720 patients with a simulated difficult airway: a multicentre randomized controlled trial. Br J Anaesth 2016; 116: 670–9. https://doi.org/10.1093/bja/aew058
Saracoglu KT, Eti Z, Kavas AD, Umuroglu T. Straight video blades are advantageous than curved blades in simulated pediatric difficult intubation. Paediatr Anaesth 2014; 24: 297–302. https://doi.org/10.1111/pan.12298
Achen B, Terblanche OC, Finucane BT. View of the larynx obtained using the Miller blade and paraglossal approach, compared to that with the Macintosh blade. Anaesth Intensive Care 2008; 36: 717–21. https://doi.org/10.1177/0310057x0803600515
Reiterer C, Waltl B, Kabon B, Schramm W. Retromolar laryngoscopy: a randomized crossover vocal cords visualization study. Minerva Anestesiol 2017; 83: 798–803. https://doi.org/10.23736/s0375-9393.17.11537-3
Serocki G, Bein B, Scholz J, Dörges V. Management of the predicted difficult airway: a comparison of conventional blade laryngoscopy with video-assisted blade laryngoscopy and the GlideScope. Eur J Anaesthesiol 2010; 27: 24–30. https://doi.org/10.1097/eja.0b013e32832d328d
de Carvalho CC, da Silva DM, Lemos VM, et al. Videolaryngoscopy vs. direct Macintosh laryngoscopy in tracheal intubation in adults: a ranking systematic review and network meta-analysis. Anaesthesia 2022; 77: 326–38. https://doi.org/10.1111/anae.15626
Oh JY, Lee JH, Kim YY, Baek SM, Jung DW, Park JH. A comparative study of glottis visualization according to the method of lifting the epiglottis in video laryngoscopy: indirect and direct lifting methods. Anesth Pain Med (Seoul) 2021; 16: 196–200. https://doi.org/10.17085/apm.20073
Driver BE, Prekker ME, Klein LR, et al. Effect of use of a Bougie vs endotracheal tube and stylet on first-attempt intubation success among patients with difficult airways undergoing emergency intubation: a randomized clinical trial. JAMA 2018; 319: 2179–89. https://doi.org/10.1001/jama.2018.6496
Grensemann J, Möhlenkamp E, Breitfeld P, et al. Tracheal tube-mounted camera assisted intubation vs. videolaryngoscopy in expected difficult airway: a prospective, randomized trial (VivaOP Trial). Front Med (Lausanne) 2021; 8: 767182. https://doi.org/10.3389/fmed.2021.767182
Buis ML, Maissan IM, Hoeks SE, Klimek M, Stolker RJ. Defining the learning curve for endotracheal intubation using direct laryngoscopy: a systematic review. Resuscitation 2016; 99: 63–71. https://doi.org/10.1016/j.resuscitation.2015.11.005
Di Marco P, Scattoni L, Spinoglio A, et al. Learning curves of the Airtraq and the Macintosh laryngoscopes for tracheal intubation by novice laryngoscopists: a clinical study. Anesth Analg 2011; 112: 122–5. https://doi.org/10.1213/ane.0b013e3182005ef0
McElwain J, Malik MA, Harte BH, Flynn NM, Laffey JG. Comparison of the C-MAC® videolaryngoscope with the Macintosh, Glidescope, and Airtraq laryngoscopes in easy and difficult laryngoscopy scenarios in manikins. Anaesthesia 2010; 65: 483–9. https://doi.org/10.1111/j.1365-2044.2010.06307.x
Author contributions
Martin Petzoldt designed the study, interpreted the data, helped to write the manuscript, and helped to acquire the data; Catharina Grün conducted the study, acquired the data, and performed the statistical analysis; Viktor A. Wünsch and Marcus Bauer helped to conduct the study and to acquire the data; Tim T. Hardel helped with the statistical analysis and to interpret the data; Jörn Grensemann designed the study, interpreted the data, helped to perform the statistical analysis, and wrote the manuscript.
Acknowledgements
We thank Dr. Hans O. Pinnschmidt for his valuable help with the power analysis.
Disclosures
Martin Petzoldt has received a study grant from Verathon Inc., Bothell, WA, USA. Tim T. Hardel has received research support from Drägerwerk; and Jörn Grensemann has received research support from Ambu and ETView, and consultant fees from Drägerwerk and GE Healthcare. The other authors declare no conflicts of interests.
Funding statement
Open Access funding enabled and organized by Projekt DEAL. The study was funded from departmental resources, with the Vie Scope® laryngoscopes kindly provided free of charge by the distributor. All other expenses were covered from departmental resources.
Data availability statement
The outcome data are available in the Electronic Supplementary Material.
Editorial responsibility
This submission was handled by Dr. Stephan K. W. Schwarz, Editor-in-Chief, Canadian Journal of Anesthesia/Journal canadien d’anesthésie.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Petzoldt, M., Grün, C., Wünsch, V.A. et al. Vie Scope® versus videolaryngoscopy in expected difficult airways: a randomized controlled trial. Can J Anesth/J Can Anesth 70, 1486–1494 (2023). https://doi.org/10.1007/s12630-023-02534-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-023-02534-y