Abstract
Purpose
The efficacy of noninvasive ventilation (NIV) during procedures that require sedation and analgesia has not been established. We evaluated whether NIV reduces the incidence of respiratory events.
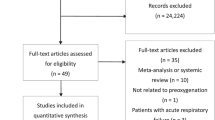
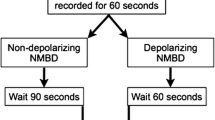
Methods
In this randomized controlled trial, we included 195 patients with an American Society of Anesthesiologists Physical Status of III or IV during electrophysiology laboratory procedures. We compared NIV with face mask oxygen therapy for patients under sedation. The primary outcome was the incidence of respiratory events determined by a computer-driven blinded analysis and defined by hypoxemia (peripheral oxygen saturation < 90%) or apnea/hypopnea (absence of breathing for 20 sec on capnography). Secondary outcomes included hemodynamic variables, sedation, patient safety (composite scores of major or minor adverse events), and adverse outcomes at day 7.
Results
A respiratory event occurred in 89/98 (95%) patients in the NIV group and in 69/97 (73%) patients with face masks (risk ratio [RR], 1.29; 95% confidence interval [CI], 1.13 to 1.47; P < 0.001). Hypoxemia occurred in 40 (42%) patients in the NIV group and in 33 (34%) patients with face masks (RR, 1.21; 95% CI, 0.84 to 1.74; P = 0.30). Apnea/hypopnea occurred in 83 patients (92%) in the NIV group vs 65 patients (70%) with face masks (RR, 1.32; 95% CI, 1.14 to 1.53; P < 0.001). Hemodynamic variables, sedation, major or minor safety events, and patient outcomes were not different between the groups.
Conclusions
Respiratory events were more frequent among patients receiving NIV without any safety or outcome impairment. These results do not support the routine use of NIV intraoperatively.
Study registration
ClinicalTrials.gov (NCT02779998); registered 4 November 2015.
Résumé
Objectif
L’efficacité de la ventilation non invasive (VNI) pendant les interventions nécessitant une sédation et une analgésie n’a pas été établie. Nous avons évalué si la VNI réduisait l’incidence des complications respiratoires.
Méthode
Dans cette étude randomisée contrôlée, nous avons inclus 195 patient·es de statut physique III ou IV selon l’American Society of Anesthesiologists pendant des interventions en laboratoire d’électrophysiologie. Nous avons comparé la VNI à l’oxygénothérapie par masque facial pour les patient·es sous sédation. Le critère d’évaluation principal était l’incidence des complications respiratoires déterminée par une analyse en aveugle assistée par ordinateur et définie par une hypoxémie (saturation périphérique en oxygène < 90 %) ou une apnée/hypopnée (absence de respiration pendant 20 secondes à la capnographie). Les critères d’évaluation secondaires comprenaient les variables hémodynamiques, la sédation, la sécurité des patient·es (scores composites des événements indésirables majeurs ou mineurs) et les issues indésirables au jour 7.
Résultats
Un événement respiratoire est survenu chez 89/98 (95 %) patient·es du groupe VNI et chez 69/97 (73 %) patient·es ayant un masque facial (risque relatif [RR], 1,29; intervalle de confiance [IC] à 95 %, 1,13 à 1,47; P < 0,001). Une hypoxémie est survenue chez 40 (42 %) patient·es du groupe VNI et chez 33 (34 %) patient·es ayant un masque facial (RR, 1,21 ; IC à 95 %, 0,84 à 1,74; P = 0,30). Une hypoxémie est survenue chez 40 (42 %) patient·es du groupe VNI et chez 33 (34 %) patient·es ayant un masque facial (RR, 1,21; IC 95 %, 0,84 à 1,74; P = 0,30). Les variables hémodynamiques, la sédation, les événements de sécurité majeurs ou mineurs et les issues pour les patient·es n’étaient pas différents entre les groupes.
Conclusion
Les complications respiratoires étaient plus fréquentes chez les patient·es recevant une VNI sans aucun impact sur la sécurité ou les issues. Ces résultats n’appuient pas l’utilisation systématique de la VNI en peropératoire.
Enregistrement de l’étude
ClinicalTrials.gov (NCT02779998); enregistrée le 4 novembre 2015.

Similar content being viewed by others
References
Brochard L, Mancebo J, Wysocki M, et al. Noninvasive ventilation for acute exacerbations of chronic obstructive pulmonary disease. N Engl J Med 1995; 333: 817–22. https://doi.org/10.1056/nejm199509283331301
Jaber S, Lescot T, Futier E, et al. Effect of noninvasive ventilation on tracheal reintubation among patients with hypoxemic respiratory failure following abdominal surgery: a randomized clinical trial. JAMA 2016; 315: 1345–53. https://doi.org/10.1001/jama.2016.2706
Zarbock A, Mueller E, Netzer S, Gabriel A, Feindt P, Kindgen-Milles D. Prophylactic nasal continuous positive airway pressure following cardiac surgery protects from postoperative pulmonary complications: a prospective, randomized, controlled trial in 500 patients. Chest 2009; 135: 1252–9. https://doi.org/10.1378/chest.08-1602
Peter JV, Moran JL, Phillips-Hughes J, Graham P, Bersten AD. Effect of noninvasive positive pressure ventilation (NIPPV) on mortality in patients with acute cardiogenic pulmonary edema: a meta-analysis. Lancet 2006; 367: 1155–63. https://doi.org/10.1016/s0140-6736(06)68506-1
Liu Q, Shan M, Liu J, Cui L, Lan C. Prophylactic noninvasive ventilation versus conventional care in patients after cardiac surgery. J Surg Res 2020; 246: 384–94. https://doi.org/10.1016/j.jss.2019.09.008
Clouzeau B, Bui HN, Vargas F, et al. Target-controlled infusion of propofol for sedation in patients with noninvasive ventilation failure due to low tolerance: a preliminary study. Intensive Care Med 2010; 36: 1675–80. https://doi.org/10.1007/s00134-010-1904-7
Deletombe B, Trouve-Buisson T, Godon A, et al. Dexmedetomidine to facilitate noninvasive ventilation after blunt chest trauma: a randomised, double-blind, crossover, placebo-controlled pilot study. Anesth Crit Care Pain Med 2019; 38: 477–83. https://doi.org/10.1016/j.accpm.2019.06.012
Cabrini L, Nobile L, Plumari VP, et al. Intraoperative prophylactic and therapeutic noninvasive ventilation: a systematic review. Br J Anesth 2014; 112: 638–47. https://doi.org/10.1093/bja/aet465
Pieri M, Landoni G, Cabrini L. Noninvasive ventilation during endoscopic procedures: rationale, clinical use, and devices. J Cardiothorac Vasc Anesth 2018; 32: 928–34. https://doi.org/10.1053/j.jvca.2017.09.038
Trouvé-Buisson T, Arvieux L, Bedague D, et al. Anesthesiological support in a cardiac electrophysiology laboratory: a single-centre prospective observational study. Eur J Anesthesiol 2013; 30: 658–63. https://doi.org/10.1097/EJA.0b013e3283626095
Esteban A, Frutos-Vivar F, Ferguson ND, et al. Noninvasive positive-pressure ventilation for respiratory failure after extubation. N Engl J Med 2004; 350: 2452–60. https://doi.org/10.1056/nejmoa032736
Auriant I, Jallot A, Hervé P, et al. Noninvasive ventilation reduces mortality in acute respiratory failure following lung resection. Am J Respir Crit Care Med 2001; 164: 1231–5. https://doi.org/10.1164/ajrccm.164.7.2101089
Squadrone V, Coha M, Cerutti E, et al. Continuous positive airway pressure for treatment of postoperative hypoxemia: a randomized controlled trial. JAMA 2005; 293: 589–95. https://doi.org/10.1001/jama.293.5.589
Pearse R, Ranieri M, Abbott T, et al. Postoperative continuous positive airway pressure to prevent pneumonia, reintubation, and death after major abdominal surgery (PRISM): a multicenter, open-label, randomized, phase 3 trial. Lancet Respir Med 2021; 9: 1221–30. https://doi.org/10.1016/S2213-2600(21)00089-8
Hui S, Fowler AJ, Cashmore RM, et al. Routine postoperative noninvasive respiratory support and pneumonia after elective surgery: a systematic review and meta-analysis of randomised trials. Br J Anaesth 2022; 128: 363–74. https://doi.org/10.1016/j.bja.2021.10.047
Moury PH, Cuisinier A, Durand M, et al. Diaphragm thickening in cardiac surgery: a perioperative prospective ultrasound study. Ann Intensive Care 2019; 9: 50. https://doi.org/10.1186/s13613-019-0521-z
Leone M, Einav S, Chiumello D, et al. Noninvasive respiratory support in the hypoxaemic peri-operative/periprocedural patient. Eur J Anesthesiol 2020; 37: 265–79. https://doi.org/10.1097/eja.0000000000001166
Jaber S, Chanques G, Jung B. Postoperative noninvasive ventilation. Anesthesiology 2010; 112: 453–61. https://doi.org/10.1097/aln.0b013e3181c5e5f2
Ambrogio C, Lowman X, Kuo M, Malo J, Prasad AR, Parthasarathy S. Sleep and noninvasive ventilation in patients with chronic respiratory insufficiency. Intensive Care Med 2009; 35: 306–13. https://doi.org/10.1007/s00134-008-1276-4
Muriel A, Peñuelas O, Frutos-Vivar F, et al. Impact of sedation and analgesia during noninvasive positive pressure ventilation on outcome: a marginal structural model causal analysis. Intensive Care Med 2015; 41: 1586–600. https://doi.org/10.1007/s00134-015-3854-6
Gaucher A, Frasca D, Mimoz O, Debaene B. Accuracy of respiratory rate monitoring by capnometry using the Capnomask(R) in extubated patients receiving supplemental oxygen after surgery. Br J Anaesth 2012; 108: 316–20. https://doi.org/10.1093/bja/aer383
Author contributions
Pierre-Henri Moury, Flora Greco, and Pierre Albaladejo designed the study; Pierre-Henri Moury, Valentin Pasquier, Flora Greco, Jean-Lionel Arvieux, Silvia Alves-Macedo, Marion Richard, and Myriam Casez-Brasseur enrolled the patients; Pierre-Henri Moury, Jean-Lionel Arvieux, Silvia Alves-Macedo, Damien Bedague, Michel Durand, and Marion Richard conducted the study; Kristina Skaare and Jean-Luc Bosson analyzed the data; Pierre-Henri Moury, Valentin Pasquier, Jean-Luc Bosson, and Pierre Albaladejo analyzed all the data; Pierre-Henri Moury and Valentin Pasquier interpreted the results; Pierre-Henri Moury and Valentin Pasquier drafted the manuscript; all authors had full access to all of the study data, contributed to drafting of the manuscript or critically revised it for important intellectual content, and took responsibility for the integrity of the data and the accuracy of the data analysis.
Acknowledgements
The authors would like to thank l’école d’infirmier anesthésiste of the CHU Grenoble Alpes, the nurse anesthetists, the anesthetists, and the intensivists of the cardiovascular and thoracic unit. The authors would like to thank the neurosurgery anesthesia and intensive care unit teams for their involvement and independent assessment in the blinded analysis: Drs Perrine Boucheix, Lara Puthon, Marie-Cécile Fèvre, and Clotilde Schilte.
Disclosures
There are no conflicts of interest to disclose related to the subject of the article.
Funding statement
This study was supported by an institutional grant from CHU Grenoble Alpes. The foundation Agiradom provided masks and the respirator. Alpha2® (Lyon, France) provided the CO2 analysis.
Prior conference presentations
The abstract of the article was accepted for presentation at the 2020 congress of the Société Française d'Anesthésie-Réanimation (24–26 Spetember 2020, Paris, France).
Editorial responsibility
This submission was handled by Dr. Philip M. Jones, Deputy Editor-in-Chief, Canadian Journal of Anesthesia/Journal canadien d’anesthésie.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Moury, PH., Pasquier, V., Greco, F. et al. A randomized controlled trial of the intraoperative use of noninvasive ventilation versus supplemental oxygen by face mask for procedural sedation in an electrophysiology laboratory. Can J Anesth/J Can Anesth 70, 1182–1193 (2023). https://doi.org/10.1007/s12630-023-02495-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-023-02495-2