Abstract
Objective
Noninvasive ventilation with pressure support (NIV-PS) therapy can augment ventilation; however, such therapy is fixed and may not adapt to varied patient needs. We tested the hypothesis that in patients with chronic respiratory insufficiency, a newer mode of ventilation [averaged volume assured pressure support (AVAPS)] and lateral decubitus position were associated with better sleep efficiency than NIV-PS and supine position. Our secondary aim was to assess the effect of mode of ventilation, body position, and sleep–wakefulness state on minute ventilation \( (\dot{V}_{E} ) \) in the same patients.
Design
Single-blind, randomized, cross-over, prospective study.
Setting
Academic institution.
Patients and participants
Twenty-eight patients.
Interventions
NIV-PS or AVAPS therapy.
Measurements and results
Three sleep studies were performed in each patient; prescription validation night, AVAPS or NIV-PS, and crossover to alternate mode. Sleep was not different between AVAPS and NIV-PS. Supine body position was associated with worse sleep efficiency than lateral decubitus position (77.9 ± 22.9 and 85.2 ± 10.5%; P = 0.04). \( \dot{V}_{E} \) was lower during stage 2 NREM and REM sleep than during wakefulness (P < 0.0001); was lower during NIV-PS than AVAPS (P = 0.029); tended to be lower with greater body mass index (P = 0.07), but was not influenced by body position.
Conclusions
In patients with chronic respiratory insufficiency, supine position was associated with worse sleep efficiency than the lateral decubitus position. AVAPS was comparable to NIV-PS therapy with regard to sleep, but statistically greater \( \dot{V}_{E} \) during AVAPS than NIV-PS of unclear significance was observed. \( \dot{V}_{E} \) was determined by sleep–wakefulness state, body mass index, and mode of therapy.
Similar content being viewed by others
Introduction
Patients with pulmonary or extra-pulmonary disorders that cause nocturnal alveolar hypoventilation—such as severe chronic obstructive pulmonary disease and morbid obesity—may develop derangements in daytime gas exchange characterized by hypoxia and hypercapnia [1, 2]. Such patients are said to have chronic respiratory insufficiency. In patients with chronic respiratory insufficiency, the failure to achieve adequate ventilation and gas exchange during sleep can lead to sleep disruption and consequent daytime sleepiness, early morning headache (due to hypercapnia), dyspnea, and fatigue [1, 2]. Correction of such ventilatory and gas exchange abnormalities using noninvasive ventilation with pressure support (NIV-PS) is a popular method for improving sleep quality, health-related quality of life, functional status, and daytime gas exchange [1–3].
In patients with chronic respiratory insufficiency, NIV-PS can improve minute ventilation \( (\dot{V}_{E} ) \) by augmenting the inspired tidal volume on a breath-by-breath basis through application of a higher inspiratory and lower expiratory PAP (IPAP and EPAP) [3]. However, such pressure settings are fixed at a certain level and may not adapt to the varying needs of a patient within a given night [3]. For example, it has been previously described that during spontaneous breathing, \( \dot{V}_{\text{E}} \) progressively decreases from wakefulness through various stages of sleep: non-rapid eye movement [NREM] 1, 2, slow wave and REM sleep [4]. Moreover, in morbidly obese patients, during spontaneous respiration, \( \dot{V}_{E} \) may decrease in the supine position when compared to the lateral decubitus position at any given sleep–wakefulness state [5]. Whether such changes in \( \dot{V}_{E} \) occur during NIV-PS therapy in patients with chronic respiratory insufficiency is unknown. Conceivably, the effectiveness of NIV-PS therapy may be limited by changes in sleep–wakefulness state or body position.
Our primary aim was to test the hypothesis that in patients with chronic respiratory insufficiency a newer mode of ventilation [averaged volume assured pressure support (AVAPS)] and the lateral decubitus position were associated with better sleep efficiency than conventional non-invasive ventilation (NIV-PS) and the supine position. Our secondary aim was to assess the effect of mode of ventilation, body position, and sleep–wakefulness state on minute ventilation in patients with chronic respiratory insufficiency.
Materials and methods
Patients
Thirty-nine patients with a diagnosis of chronic respiratory insufficiency were recruited. Institutional Review Board of the University of Arizona approved the study and written informed consent was obtained from each participant. Patients with chronic respiratory insufficiency (obesity hypoventilation syndrome with or without obstructive sleep apnea, chronic obstructive pulmonary disease, neuromuscular disease) who were currently receiving home ventilation (NIV-PS) for at least 2 months and adherent to such therapy (>4 h per night by compliance download) were considered eligible (Tables 1, 2). Exclusion criteria were: (1) Clinically unstable [hemodynamically unstable (systolic blood pressure <90 mmHg)] or acute respiratory failure [hypoxemia; SpO2 <88% despite O2 supplementation up to 4 lpm] or impending respiratory failure [respiratory rate >35 breaths per min and use of accessory muscles of respiration]; (2) history of heart failure or Cheyne–Stokes respiration; (3) inability to clear secretions; (4) acute sinusitis, otitis media, facial trauma, burns and other anatomic abnormalities interfering with mask fit; (5) inability to remove face mask due to neurological impairment. None of the patients were fully ventilator dependent (i.e., requiring greater than 6 h of ventilation per 24 h). The study was conducted in the hospital ward.
Study design
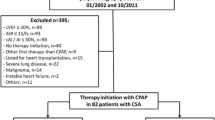
All modes of ventilation were provided by the same device using a full-face mask (AVAPS/BiPAP Synchrony; Respironics Inc; Murrysville, PA). Each subject underwent three consecutive overnight sleep studies: (1) Conventional NIV-PS set at the respective patients’ prescription settings in order to validate the prescription pressure and serve as an acclimatization night, (2) AVAPS or NIV therapy assigned randomly, and (3) and crossed over to alternate therapy mode (Fig. 1). Patients underwent randomization only if their prescription pressure did not change significantly (>5 cm H2O) during the first sleep study.
Schematic diagram showing flow of patients through the study. Dashed horizontal lines delineate as to which sleep study night the respective procedures were performed. At the start of the second sleep study night, the technician determined the baseline tidal volume (V T) over the last 1 min of a 30-min period during calm wakefulness at CPAP setting of 6 cm H2O. Subsequently, the subjects were given two 30-min trials of AVAPS, while the target V T was set at 110% of the baseline V T or at a V T derived from ideal body weight (8 ml/Kg ideal body weight). The target V T setting with the lowest dyspnea score was chosen as the preferred target V T. In the event that the subjects gave the same rating to both (target V T) trials they were queried as to which trial they preferred most
Measurements
Polysomnography
Standard full-night polysomnography (Sandman, Ontario, CA) entailed EEG (C4-A1, C3-A2, O1-A2, and O2-A1), left and right EOG, sub-mental EMG, ECG, thoraco-abdominal movement by inductance plethysmography, leg movements by bilateral anterior tibialis EMG, body position by a small sensor attached to the chest belt, naso-oral airflow using thermistor, flow and tidal volume output from the ventilator monitoring, and finger pulseoximetry. Sleep was manually staged in 30-s epochs according to standard criteria [6], and respiratory events according to consensus conference recommendations [7].
Validation of device tidal volume output
In a bench study, with the ventilator used to deliver AVAPS and PS connected to an artificial lung simulator (ASL 5000™, Ingmar Medical, Pittsburgh, PA) via a heated calibrated pneumotachograph (Hans-Rudolf, Kansas City, MO), we validated the accuracy of the tidal volume output generated by the device [8]. Three separate runs at different tidal volume settings (500, 750, and 1,000 ml) were conducted for 5 min each and the tidal volume output of the device was compared to that measured by the pneumotachograph (gold standard). The bias (<6%) and precision (<1%) errors of the device V T output were excellent.
Device settings
In each patient, NIV-PS settings were confirmed to be adequate during the first sleep study and remained at such settings during the subsequent NIV-PS therapy night. For AVAPS settings, maximum IPAP (IPAPmax) was set at 10 cm H2O above the prescription IPAP or at 30 cm H2O; whichever was the lowest. The minimum range for the IPAP (IPAPmin) was set 5 cm H2O below the prescribed IPAP level. During AVAPS, the actual IPAP level fluctuated between IPAPmax and IPAPmin to ensure adequate “target” tidal volume averaged over a 1-min period (principle of operation). Preferred target tidal volume was tailored for each patient by determining breathing comfort when tidal volume was set at 110% of baseline [9] (determined during CPAP of 6 cm H2O and calm wakefulness) or 8 mL/Kg of Ideal Body Weight (Fig. 1). Calm wakefulness was defined as a period when the subjects were supine with eyes closed and there was EEG evidence for alpha rhythm (8–12 Hz) with no evidence for movement based upon EMG and video assessment. Breathing comfort was assessed by modified Borg dyspnea scale at the end of 30 min of each setting. The target V T setting with the lowest dyspnea score was chosen as the preferred target V T. In the event that the subjects gave the same rating to both (target V T) trials, they were queried as to which trial they preferred most. In our study, 16 patients preferred 110% of the baseline V T whereas, 12 patients preferred 8 mL/Kg of ideal body weight. During AVAPS, EPAP level was the same as that during NIV-PS therapy.
Titration of pressure during prescription validation
During polysomnography (first sleep study), the EPAP setting was begun at 4 cm H2O with a minimum IPAP of 8 cm H2O, which translates to a NIV-PS level of 4 cm H2O. Subsequently, both IPAP and EPAP were increased by 2 cm H2O increments in response to (a) obstructive apneas, (b) hypopneas (defined as 50% reduction in flow signal accompanied by 3% desaturation by pulseoximetry), (c) inspiratory flow limitation events identified by flow waveform, or (d) snoring. IPAP level alone was increased by 2 cm H2O increments when persistent evidence for hypoventilation [SpO2 < 88% for 3 continuous epochs (90 s) was present in the absence of above-mentioned obstructive events].
Measurement of \( \dot{V}_{E} \)
Breath-by-breath measurements of tidal volume output “recorded simultaneously with the conventional tracings of the polysomnography” were analyzed over one-min blocks during various stages of sleep and body position. Care was taken to ensure that such time periods were devoid of arousals during sleep and movement during wakefulness (calm wakefulness). Tidal volume, respiratory rate, and minimum SpO2 (min SpO2) were measured and \( \dot{V}_{E} \) calculated as the product of tidal volume and respiratory rate.
Data analysis
Results are reported as mean ± SD unless otherwise specified. One-way or two-way repeated-measures analysis of variance (ANOVA) was performed to identify significant covariates that influenced \( \dot{V}_{E} . \) Multivariate regression models were constructed with \( \dot{V}_{E} \) as dependent variable after significant determining variables were identified by univariate regression techniques (a probability of 0.05 was regarded as significant). Multi-collinearity among independent variables was verified, and in the event of collinearity only the strongest predictor variable was included.
Results
Twenty-eight of 39 patients were found to have adequate pressure settings and went on to receive NIV-PS or AVAPS on separate nights (Tables 1, 2). IPAP level during NIV-PS remained fixed at 17 ± 4 cm H2O. During AVAPS therapy, set IPAPmin and IPAPmax were 13 ± 4 and 26 ± 3 cm H2O, respectively. During AVAPS therapy, the mean IPAP pressure was 18 ± 5 cm H2O which tended to be higher than IPAP during NIV-PS (17 ± 4 cm H2O; P = 0.08; paired t test), and the IPAP during AVAPS therapy was noted to fluctuate between a low of 14 ± 6 cm H2O and a high of 21 ± 5 cm H2O.
Sleep architecture
Neither NIV-PS nor AVAPS significantly modified sleep architecture, quality, or quantity (Table 3). However, supine body position was associated with worse sleep efficiency than the lateral decubitus position (77.9 ± 22.9 and 85.2 ± 10.5%; P = 0.04). Further analysis for the possible mechanisms that underlie such association revealed that the apnea-hypopnea index was greater during supine (median 6.3, IQR 1.8, 60 per hour) than during lateral position (median 0.6, IQR 0, 3.7 per hour; P < 0.0001).
Minute ventilation
During NIV-PS therapy in the supine position (Fig. 2; left panel, closed symbols), \( \dot{V}_{E} \) decreased progressively from wakefulness through various stages of sleep: stage 1, stage 2, and REM (one-way ANOVA with repeated measures; P = 0.0001). During NIV-PS therapy in the lateral decubitus position (Fig. 2; right panel; closed symbols), \( \dot{V}_{E} \) decreased progressively from wakefulness through various stages of sleep: stage 1, stage 2, and REM (one-way ANOVA with repeated measures; P = 0.018). During AVAPS in the supine position, however, \( \dot{V}_{\text{E}} \) did not change from wakefulness to every sleep stages [P = 0.2; (Fig. 2, left panel; open symbols)]. Moreover, during AVAPS in the lateral decubitus position, \( \dot{V}_{E} \) tended to decrease across sleep–wakefulness states [P = 0.10; (Fig. 2; right panel; open symbols)]. The changes in \( \dot{V}_{E} \) across the various sleep–wakefulness states were different between AVAPS and NIV-PS therapy (2-way ANOVA with repeated measures; P = 0.02; Fig. 2). Changes in body position did not influence \( \dot{V}_{E} \) (P = 0.9). For both modes of therapy and body positions combined, \( \dot{V}_{E} \) progressively decreased from 8.7 ± 2.3 during wakefulness to 7.8 ± 1.8, 7.4 ± 1.6, and 7.3 ± 1. 7 L/min during stage 1, stage 2, and REM sleep, respectively (P < 0.0001, ANOVA). Moreover, regardless of body position or sleep–wakefulness state, \( \dot{V}_{E} \) during AVAPS (8.0 ± 1.9 L) was greater than during NIV-PS therapy (7.6 ± 2.0 L; P = 0.03).
Minute ventilation during supine (left panel) and lateral decubitus position (right panel) while receiving bilevel positive airway pressure (NIV-PS; closed symbols) or averaged volume assured pressure support (AVAPS; open symbols). Minute ventilation associated with wakefulness and different stages of sleep are shown. Each symbol is derived from minute ventilation measured at a given body position, sleep–wakefulness state, and mode of PAP therapy in 28 patients. Post hoc comparison are represented by asterisk symbol if statistically significant (Neuman–Keuls; P < 0.05)
Univariate regression with various determining variables revealed that sleep–wakefulness state, mode of therapy (AVAPS or NIV-PS) and to a lesser extent body mass index (BMI) influenced \( \dot{V}_{E} \) (dependent variable) (Table 4). Multivariate regression revealed that NIV-PS therapy; sleep; and greater BMI were associated with lower \( \dot{V}_{E} \) (model R 2 = 0.09, P < 0.0001; Table 4).
Tidal volume
The reduction in \( \dot{V}_{E} \) in relation to various sleep states appeared to be primarily the result of a reduction in V T from wakefulness through the various sleep stages (P < 0.0001; one-way ANOVA). Changes in body position did not influence V T (P = 0.17). For both modes of therapy and body positions combined, V T was reduced from wakefulness (619 ± 163 mL) to stage 1 (546 ± 156 mL), stage 2 (513 ± 135 mL) and REM sleep (505 ± 150 mL) (P < 0.0001).
Univariate regression revealed that sleep-wakefulness state, mode of therapy (AVAPS or NIV-PS), body mass index (BMI), and O2 therapy influenced V T (Table 5). Multivariate regression revealed that NIV-PS therapy, sleep, and greater BMI were independently associated with lower V T (model R 2 = 0.13, P < 0.0001; Table 5).
Respiratory rate and oxygenation
Respiratory rate, however, was not altered by changes in sleep–wakefulness state or body position. In 11 patients who did not receive oxygen supplementation, minimum oxygen saturation (min SpO2) was 92.8 ± 3.6% and a 230 mL decrement in \( \dot{V}_{E} \) was associated with a 1% decrement in SpO2 (r 2 = 0.01; P = 0.038). In such patients, min SpO2 tended to be higher during AVAPS night (93.2 ± 2.5%) than during NIV-PS night (92.4 ± 3.6%; P = 0.10). Arterial blood gases were not different following the nights when patients received either NIV-PS or AVAPS therapy (Table 6).
Discussion
Sleep–wakefulness state
In spontaneously breathing healthy subjects, respiratory drive, and consequently \( \dot{V}_{E} , \) decreases progressively from wakefulness through various stages of sleep [4]. In disease states, decrements in \( \dot{V}_{E} \) during various stages of sleep has been measured in patients with COPD [10, 11], cystic fibrosis [12, 13] and may result in oxygen desaturation [14] and hypercarbia [15]. Whether such hypoventilation occurs during non-invasive PAP therapy, however, is less clear. Milross and colleagues [12] found decrements in \( \dot{V}_{E} \) in patients with cystic fibrosis while receiving NIV-PS therapy; however, they did not adjust for BMI or body position. Moreover, in the same study, \( \dot{V}_{E} \) decreased by only 10% with deeper stages of sleep as compared to wakefulness. In the current study, however, deeper stages of sleep were associated with up to 24% drop in \( \dot{V}_{E} \) when compared to wakefulness (Fig. 2) and such changes were adjusted for influences from BMI and body position. While some of the drop in \( \dot{V}_{E} \) could be physiological, a 24% drop in \( \dot{V}_{\text{E}} \) appears to be in greater than expected.
Conversely, one could interpret the \( \dot{V}_{E} \) data to suggest that during NIV-PS therapy \( \dot{V}_{E} \) is greater during wakefulness than during sleep (Fig. 2). Such a higher level of \( \dot{V}_{E} \) following sudden change from sleep to wakefulness—“ventilatory overshoot”—may, in some patients, set the stage for central apneas and sequelae [16–19]. Nevertheless, the inability of NIV-PS therapy to “adapt” to changes in sleep–wakefulness state may be a limitation. In our study, however, such lack of adaptation translated only to minor changes in oxygen saturation and there was no effect on sleep (Table 3). The lack of benefit to sleep measures may be attributable to the study design that potentially favored NIV-PS therapy; patients had been using NIV-PS therapy for over 2 months but were naïve to AVAPS. In contrast, Storre and colleagues [20] recruited patients naïve to NIV and found that sleep quality was better during AVAPS than during NIV-PS therapy. Moreover, the fact that NIV-PS setting was confirmed to be adequate during the first sleep study makes unlikely the probability of finding clinically significant differences compared to AVAPS during the subsequent night. Conceivably, it may be possible to set a ventilator mode in a certain way so as to obtain proper ventilatory support for the patient. The only difference is the complexity of the procedure of setting the ventilator for each mode. AVAPS might be easier to be set to obtain adequate ventilation compared to NIV-PS.
Other investigators have studied patients with chronic respiratory insufficiency while receiving NIV-PS therapy and noticed variability in \( \dot{V}_{E} \) [21], albeit less than that during proportional assist ventilation. In our study, we report less variability in \( \dot{V}_{E} \) during AVAPS than during NIV-PS therapy. Such lack of variability may be important in guaranteeing \( \dot{V}_{E} \) in patients with chronic respiratory insufficiency.
Sleep and body position
Our finding that supine body position was associated with worse sleep efficiency than the lateral decubitus position during assisted ventilation is novel. Further analysis for the possible mechanisms that underlie such association revealed that the apnea-hypopnea index was greater during supine than during lateral decubitus position. Because IPAP and EPAP levels were titrated to control obstructive apneas and obstructive hypopneas during the first “prescription validation” sleep study, only patients whose obstructed ventilation was successfully controlled were allowed to remain in the study. Consequently, the respiratory events that resulted in differences between supine and lateral position were primarily central apneas and non-obstructive hypopneas (as evidenced by the lack of a flow-limitation pattern in the inspiratory portion of the flow tracing). This finding is in line with our prior work that demonstrated that occurrence of central apneas was associated with worsening of sleep efficiency [16].
Interestingly, we did not observe any effect of body position on \( \dot{V}_{E} \) (Table 5). The respiratory effects of body position during sleep have been widely studied in normal subjects and in patients breathing spontaneously [22, 23], in patients with OSA [24] and in stable chronic hypercapnic COPD patients [25]. Some investigators [26] observed that V T, \( \dot{V}_{E} \) and lung compliance significantly decreased whereas, respiratory resistance increased while supine when compared to sitting position in spontaneously breathing healthy subjects. In awake patients with COPD, however, body position does not significantly influence breathing pattern and respiratory muscles function during NIV-PS therapy [25]. Similarly, our data shows that in patients with chronic respiratory insufficiency, who were receiving NIV-PS therapy, changes in posture did not influence \( \dot{V}_{E} . \) Therefore, the present study provides evidence that NIV-PS therapy is able to achieve adequate ventilation despite changes in body position. Moreover, since respiratory mechanics differ between wakefulness and sleep [13], results obtained during diurnal NIV-PS therapy in awake COPD patients [25] cannot apply to the night time use during sleep, our data provides additional useful information.
Mode of therapy
The finding that changes in \( \dot{V}_{E} \) were primarily due to changes in V T rather than respiratory rate calls for a mode of ventilation that corrects the variance in V T. In line with such reasoning, the decrement in \( \dot{V}_{E} \) was greater during NIV-PS therapy than AVAPS, the latter being capable of adjusting IPAP to achieve target V T. In the 11 patients who were not receiving supplemental O2, minimum SpO2 was higher during AVAPS when compared to NIV-PS therapy. This indicates that AVAPS therapy, through increments in V T, is able to prevent hypoventilation, and, thus, attenuate oxygen desaturation.
Limitations
Statistically greater \( \dot{V}_{E} \) during AVAPS than NIV-PS may not necessarily represent a clinical advantage. Moreover, although differences in \( \dot{V}_{E} \) between NIV-PS and AVAPS were statistically significant, they appear clinically minor. There are other limitations to our study. Our failure to adjust the V T measurements for air leak on a breath-by-breath basis is a limitation. However, the algorithms operating in the device are meant to adjust for the “baseline drift” in the integrated volume signal derived from flow inputs as a surrogate measure of air leak. More importantly, our inferences derived from differences in \( \dot{V}_{E} \) and daytime arterial blood gases are limited by the lack of measures of arterial PCO2 during sleep. Lastly, we caution that while mechanistic underpinnings between critically ill patients and patients with chronic respiratory insufficiency may be the similar, the presented data cannot be extrapolated to patients with acute respiratory failure without further study. Specifically, subjective perception of dyspnea that were obtained during AVAPS in our study limit the extrapolation of our results to critically ill patients. Moreover, our failure to obtain similar dyspnea ratings during NIV-PS may have favored the AVAPS mode.
Conclusions
In conclusion, in patients with chronic respiratory insufficiency, supine position was associated with worse sleep efficiency than the lateral decubitus position. AVAPS was comparable to NIV-PS therapy with regards to sleep, but statistically greater \( \dot{V}_{E} \) during AVAPS than NIV-PS of unclear significance was observed. \( \dot{V}_{\text{E}} \) was determined by sleep–wakefulness state, body mass index, and mode of therapy, but not by body position. Changes in \( \dot{V}_{E} \) during NIV-PS therapy were independent of effects of body position and BMI and was primarily due to decrements in tidal volume rather than in respiratory rate; and was less likely during AVAPS than NIV-PS therapy.
References
Gay PC (2004) Chronic obstructive pulmonary disease and sleep. Respir Care 49:39–51
Mehta S, Hill NS (2001) Noninvasive ventilation. Am J Respir Crit Care Med 163:540–577
Sanders MH, Kern N (1990) Obstructive sleep apnea treated by independently adjusted inspiratory and expiratory positive airway pressures via nasal mask. Physiologic and clinical implications. Chest 98:317–324
Calverley PMA (1998) Impact of sleep on respiration. Eur Resp Monogr 10:9–27
Parameswaran K, Todd DC, Soth M (2006) Altered respiratory physiology in obesity. Can Respir J 13:203–210
Rechtschaffen A, Kales A (1968) A manual of standardized terminology, techniques, and scoring system for sleep staging in human subjects. National Institute of Health, Washington DC, publication No. 204
American Academy of Sleep Medicine (1999) Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research; the Report of an American Academy of sleep Medicine Task Force. Sleep 22:667–689
Coller D, Stanley D, Parthasarathy S (2005) Effect on air leak on the performance of auto-PAP devices: a bench study. Sleep Breath 9:167–175
Brack T, Jubran A, Tobin MJ (2002) Dyspnea and decreased variability of breathing in patients with restrictive lung disease. Am J Respir Crit Care Med 165:1260–1264
O’Donoghue FJ, Catcheside PG, Eckert DJ, McEvoy RD (2004) Changes in respiration during NREM sleep in hypercapnic chronic obstructive pulmonary disease. J Physiol 559:663–673
Ballard RD, Clover CW, Suh BY (1995) Influence of sleep on respiratory function in emphysema. Am J Respir Crit Care Med 151:945–951
Milross MA, Piper AJ, Norman M, Becker HF, Willson GN, Grunstein RR, Sullivan CE, Bye PT (2001) Low-flow oxygen and bilevel ventilatory support. Effect on ventilation during sleep in cystic fibrosis. Am J Respir Crit Care Med 163:129–134
Ballard RD, Sutarik JM, Clover CW, Suh BY (1996) Effect of non REM sleep on ventilation and respiratory mechanics in adult with cystic fibrosis. Am J Respir Crit Care Med 153:266–271
Becker HF, Piper AJ, Flynn WE, McNamara SG, Grunstein RR, Peter JH, Sullivan CE (1999) Breathing during sleep in patients with nocturnal desaturation. Am J Respir Crit Care Med 159:112–118
Skatrud JB, Dempsey JA, Iber C, Berssenbrugge A (1981) Correction of CO2 retention during sleep in patients with chronic obstructive pulmonary diseases. Am Rev Respir Dis 124:260–268
Parthasarathy S, Tobin MJ (2002) Effect of ventilator mode on sleep quality in critically ill patients. Am J Respir Crit Care Med 166:1423–1429
Khoo MC, Koh SS, Shin JJ, Westbrook PR, Berry RB (1996) Ventilatory dynamics during transient arousal from NREM sleep: implications for respiratory control stability. J Appl Physiol 80:1475–1484
Fanfulla F, Delmastro M, Berardinelli A, Lupo ND, Nava S (2005) Effects of different ventilator settings on sleep and inspiratory effort in patients with neuromuscular disease. Am J Respir Crit Care Med 172:619–624
Meza S, Mendez M, Ostrowski M, Younes M (1998) Susceptibility to periodic breathing with assisted ventilation during sleep in normal subjects. J Appl Physiol 85:1929–1940
Storre JH, Seuthe B, Fiechter R, Milioglou S, Dreher M, Sorichter S, Windisch W (2006) Average volume-assured pressure support in obesity hypoventilation: a randomized crossover trial. Chest 130:815–821
Porta R, Appendini L, Vitacca M, Bianchi L, Donner CF, Poggi R, Ambrosino N (2002) Mask proportional assist vs pressure support ventilation in patients in clinically stable condition with chronic ventilatory failure. Chest 122:479–488
Beharakis PK, Baydur A, Jaeger MJ, Milic-Emili J (1983) Lung mechanics in sitting and horizontal body position. Chest 83:643–646
Berger R, Burky NK (1982) The effect of posture on total respiratory compliance. Am Rev Respir Dis 125:275–280
Younes M (2003) Contributions of upper airway mechanics and control mechanisms to severity of obstructive apnea. Am J Respir Crit Care Med 168:645–658
Porta R, Vitacca M, Clini E, Ambrosino N (1999) Physiological effects of posture on mask ventilation in awake stable chronic hypercapnic COPD patients. Eur Respir J 14:517–522
Vitacca M, Clini E, Spassini W, Scaglia L, Negrini P, Quadri A (1996) Does the supine position worsen respiratory function in elderly subjects? Gerontology 42:46–53
Acknowledgments
The authors are indebted to the participants in this study. S.P. had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Funded by Respironics Inc. The authors are grateful to Dr. Stuart Quan and Ralph Fregosi PhD for their critical review of the manuscript.
Conflict of interest
Dr. Parthasarathy received research funding from Respironics, Inc. for the conduct of this study. None of the other authors have any existent or potential conflicts of interest, including specific financial interests that is relevant to the subject of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ambrogio, C., Lowman, X., Kuo, M. et al. Sleep and non-invasive ventilation in patients with chronic respiratory insufficiency. Intensive Care Med 35, 306–313 (2009). https://doi.org/10.1007/s00134-008-1276-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-008-1276-4