Abstract
There are two anatomic formulations of death by neurologic criteria accepted worldwide: whole-brain death and brainstem death. As part of the Canadian Death Definition and Determination Project, we convened an expert working group and performed a narrative review of the literature. Infratentorial brain injury (IBI) with an unconfounded clinical assessment consistent with death by neurologic criteria represents a nonrecoverable injury. The clinical determination of death cannot distinguish between IBI and whole-brain cessation of function. Current clinical, functional, and neuroimaging assessments cannot reliably confirm the complete and permanent destruction of the brainstem. No patient with isolated brainstem death has been reported to recover consciousness and all patients have died. Studies suggest a significant majority of isolated brainstem death will evolve into whole-brain death, influenced by time/duration of somatic support and impacted by ventricular drainage and/or posterior fossa decompressive craniectomy. Acknowledging variability in intensive care unit (ICU) physician opinion on this matter, a majority of Canadian ICU physicians would perform ancillary testing for death determination by neurologic criteria in the context of IBI. There is currently no reliable ancillary test to confirm complete destruction of the brainstem; ancillary testing currently includes evaluation of both infratentorial and supratentorial flow. Acknowledging international variability in this regard, the existing evidence reviewed does not provide sufficient confidence that the clinical exam in IBI represents a complete and permanent destruction of the reticular activating system and thus the capacity for consciousness. On this basis, IBI consistent with clinical signs of death by neurologic criteria without significant supratentorial involvement does not fulfill criteria for death in Canada and ancillary testing is required.
Résumé
Il existe deux formulations anatomiques du décès selon des critères neurologiques acceptés dans le monde entier : la mort du cerveau entier et la mort du tronc cérébral. Dans le cadre du Projet canadien de définition et de détermination du décès, nous avons réuni un groupe de travail composé d’experts et réalisé un compte rendu narratif de la littérature. Une lésion cérébrale infratentorielle (LCI) avec une évaluation clinique sans facteur confondant et compatible avec un décès selon des critères neurologiques représente une atteinte irrécupérable. La détermination clinique du décès ne permet pas de faire la distinction entre une LCI et l’arrêt de la fonction dans le cerveau entier. Les évaluations cliniques, fonctionnelles et de neuroimagerie actuelles ne peuvent pas confirmer de manière fiable la destruction complète et permanente du tronc cérébral. La récupération de la conscience n’a jamais été signalée chez aucun patient présentant une mort isolée du tronc cérébral, et tous les patients sont décédés. Des études suggèrent qu’une majorité significative des morts isolées du tronc cérébral évolueront vers la mort cérébrale entière, étant influencées par le temps et la durée de l’assistance somatique et impactées par le drainage ventriculaire et/ou la craniectomie décompressive de la fosse postérieure. Compte tenu de la variabilité des opinions des médecins intensivistes à ce sujet, la majorité des médecins intensivistes canadiens réaliseraient des examens auxiliaires pour déterminer le décès selon des critères neurologiques dans le contexte d’une LCI. Il n’existe actuellement aucun examen auxiliaire fiable pour confirmer la destruction complète du tronc cérébral; les examens auxiliaires comprennent actuellement l’évaluation de la circulation infratentorielle et supratentorielle. Reconnaissant la variabilité internationale à cet égard, les données probantes existantes passées en revue ne sont pas suffisamment fiables pour affirmer que l’examen clinique en cas de LCI représente une destruction complète et permanente du système d’activation réticulaire et donc de la capacité de conscience. En se fondant sur cette base, une LCI compatible avec les signes cliniques d’un décès selon des critères neurologiques sans atteinte supratentorielle significative ne répond pas aux critères de décès au Canada et un examen auxiliaire est requis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Death is defined in Canada1 and internationally2 as the permanent cessation of brain function characterized by the complete absence of consciousness and the absence of brainstem reflexes, including the ability to breathe independently. Two anatomic formulations of death by neurologic criteria are accepted worldwide: whole-brain death and brainstem death. The concept of brainstem death was originally advanced by Pallis and influenced practice in the UK and other commonwealth countries.3 There is international variability and inconsistency in whether death by neurologic criteria is conceptually defined based on permanent loss of brainstem function (“brainstem death”) or whole-brain function (“whole-brain death”). A review of international protocols (n = 72) shows that 65/72 (90%) protocols are whole-brain based whereas 7/72 (10%) refer to brainstem death, but only 3/72 (4%) clearly accept brainstem formulations of death.4 Whereas the distinction between whole-brain and brainstem formulations of death are primarily anatomic, the definition of death by neurologic criteria is based on the permanent cessation of pertinent brain functions (such as the capacity for consciousness and the ability to breathe, and excluding neuroendocrine functions), and there is currently debate as to whether legal definitions of death should be based on the loss of these essential functions to align with current medical evidence and practice.5 Previous Canadian guidelines are not definitive6 on the distinction between whole-brain and brainstem formulations, and Canadian expert evidence-informed consensus is required to guide clinical practice.
As part of the Canadian Critical Care Society, Canadian Medical Association, and Canadian Blood Services project “Brain-Based Definition of Death and Criteria for its Determination After Arrest of Circulation or Neurologic Function in Canada,” we convened a working group of neurocritical care experts to address the question of whether infratentorial brain injury (IBI) fulfills the criteria for death in Canada. We performed a narrative review and synthesis of the literature on the elucidation of the reticular activating system and its role in consciousness.7 This review included searches of MEDLINE from inception to August 2021, and a comprehensive search of texts and reference lists to identify historical experimental evidence prior to 1966. The natural history of infratentorial brain injury among patients suspected of death by neurologic criteria was based on a recently published systematic review, conducted by working group members.8 There were multiple meetings to discuss concepts, existing scientific foundations, and limitations to inform practice. We formulated a proposal which we presented for review by the project’s Guideline Panel; it subsequently was endorsed by the project’s Steering Committee.
An IBI is a brainstem or cerebellar lesion such as ischemic or hemorrhagic stroke. In its most devastating form, it can lead to loss of all clinically detectable brainstem function. On presentation, the lesion may be isolated to the brainstem without significant supratentorial cerebral involvement, but it may lead to supratentorial involvement with time. Isolated brainstem death can occur in a patient with an IBI who fulfills all clinical criteria for death by neurologic criteria, but in whom there is evidence of preserved supratentorial blood flow, perfusion, or electrophysiologic activity, the clinical significance of which is currently unknown. Whole-brain death is the diagnosis and confirmation of death based on cessation of brainstem function requiring demonstration of both brainstem and cerebrum involvement, typically through neuroimaging. The clinicial assessment for both formulations are identical and clinically indistinguishable, based on the absence of consciousness, absence of brain-mediated motor responses, and brainstem areflexia, including the capacity to breathe independently.
Clinical and neurophysiologic experiments have made clear that a functioning reticular activating system (RAS) is a key requirement for consciousness,7 hence the primacy of the brainstem exam in all clinical assessments for death by neurologic criteria. Infratentorial brain injury may conceptually fulfill the criteria for death by neurologic criteria based on the complete and permanent loss of function of the RAS. Brainstem formulations of death by neurologic criteria infer the permanent loss of consciousness through destruction of the RAS, manifest by the lack of measurable brainstem function.
The World Brain Death Project2 supported a whole-brain concept of death, but acknowledged international variability and suggested that if an assessment for death by neurologic criteria is being made in a region that equates whole-brain death with death by neurologic criteria, in the setting of an isolated brainstem lesion or posterior circulation vascular lesion, ancillary testing should be performed. In these circumstances, it was suggested that death by neurologic criteria should not be diagnosed until supratentorial and infratentorial blood flow is lost.
Potential challenges to clinical assessment of death by neurologic criteria in infratentorial brain injury
Infratentorial brain injury may cause loss of all detectable brainstem function such that patients may fulfill clinical determination of death by neurologic criteria while still having ancillary test evidence of preserved supratentorial blood flow, perfusion, and/or electrical activity.8,9,10 Compared with global or supratentorial brain injuries leading to death by neurologic criteria, it may be more challenging to confirm the complete destruction of the RAS, thus ensuring that there is permanent loss of the capacity of consciousness and fulfilling this defining criterion for death.
In patients who fulfill clinical criteria for death by neurologic criteria following a supratentorial or global brain injury, the mechanism of brainstem injury occurs through transtentorial herniation after malignant supratentorial intracranial hypertension and progressive rostrocaudal infarction. This descending infarction implies that, at the time of the infarction of the brainstem and RAS, all superior elements of the RAS network (the basal forebrain, thalamus, and thalamocortical projections) are also damaged, thus providing reassurance that the capacity for consciousness is lost.
The pathophysiology is different in IBI where the direct infratentorial lesion may, or may not, cause complete brainstem infarction. Reports of perfusion or electrical cortical activity in patients with IBI and a clinical exam consistent with death by neurologic criteria would suggest that it is possible for some rostral elements of the RAS to persist despite the absence of clinically demonstrable brain function. It is not infrequent for patients fulfilling clinical criteria for death by neurologic criteria following a devastating supratentorial or global brain injury to have preserved cerebral blood flow on ancillary testing. Nevertheless, preserved cerebral blood flow, perfusion, or electrophysiologic activity on ancillary testing appears to be more common among patients fulfilling clinical criteria for death by neurologic criteria following a primary IBI than in patients fulfilling clinical criteria for death by neurologic criteria following a primary supratentorial brain injury.11 The clinical significance of preserved blood flow, perfusion, or electrical activity in patients meeting clinical criteria for death by neurologic criteria is currently unknown.12 The presence of these vascular and, in particular, neurophysiologic phenomena make it difficult to confidently confirm the permanent and complete loss of consciousness at that moment in time, and thus failing to fulfill this key defining criterion for death. There is no method to clinically differentiate IBI from whole-brain death, and the transition from IBI to whole-brain death (in those patients in whom it occurs) is also clinically silent.
There are currently insufficient data to support the inference that the absence of clinically detectable brainstem function in patients without evidence of supratentorial injury is adequate to conclude complete brainstem destruction and exclude the capacity for conciousness. Studies evaluating any potential for covert consciousness in patients with IBI and isolated brainstem death have not yet been performed. Consequently, the inference that absence of demonstrable brainstem function in IBI reflects complete and permanent loss of the capacity for consciousness cannot be validated at this point in time, although this may change with further research. Such research may be challenging given that severe brainstem injury may cause cognitive motor dissociation if it were to exist. The only intact sensory pathway in IBI without supratentorial involvement relate to visual pathways, and studies to assess any potential for functional cerebral response to visual inputs have not been performed.
Ancillary testing to support death by neurologic criteria in infratentorial brain injury
Infratentorial brain injury, primary supratentorial brain injury, and whole-brain injury can all eventually cause complete absence of consciousness and absence of brain stem reflexes. Death is principally a clinical determination by bedside physical examination; ancillary testing is reserved for when prerequisites cannot be fulfilled, confounding conditions cannot be resolved, or the clinical exam cannot be fully completed. Currently recommended ancillary testing is based on the absence of whole-brain blood flow/perfusion.1,2 There is currently no perfectly reliable ancillary test to confirm the destruction of the entire brainstem. Concerns regarding IBI and the possibility of undetected cerebral function or covert consciousness may lead many clinicians to consider ancillary testing in this context to reassure themselves of the loss of the capacity for consciousness by showing whole-brain injury.9 Given existing clinical assessment for death by neurologic criteria cannot distinguish IBI from whole-brain death, neuroimaging and/or ancillary testing is required to distinguish these conditions. In a survey of Canadian intensive care unit (ICU) physicians, 59% of respondents would perform ancillary testing in patients with IBI who appear to fulfill clinical criteria for death by neurologic criteria, whereas 30% would not.13
Prevalence, characteristics, and evolution of isolated brainstem death
A recent Alberta study estimated that the annual incidence of infratentorial stroke leading to clinical criteria for death by neurologic criteria is 0.55 cases per million population.9 On this basis, the estimated Canadian incidence would be approximately 20 cases per year. There is variability in clinicians’ use of ancillary testing in this situation. Persistent supratentorial blood flow was detected in more than half (6/10) of infratentorial stroke patients that underwent radionuclide scans. A systematic review and meta-analysis of the prevalence, characteristics and evolution of IBI,8 including isolated brainstem death shows the prevalence of IBI among patients suspected of death by neurologic criteria ranged from 2% to 16% (mean prevalence, 6.3%; highest density interval 2.4–14.2%), whereas the prevalence of isolated brainstem death ranged from 1% to 4% (mean prevalence, 1.5%; highest density interval, 0.5–3.9%). A total of 38 isolated brainstem death cases were found in the literature, all of which had infratentorial strokes. Among these 38 patients, 20 had electroencephalography background activity in the alpha or theta frequencies, 19 had preserved cerebral blood flow, two had preserved supratentorial cerebral perfusion, two had cortical responses to visual-evoked potentials, and one had cortical responses to somatosensory-evoked potentials (the presence of which calls into question the completeness of brainstem destruction). At the latest follow-up provided in these reports, 28 of the 38 cases had progressed to whole brain death based on repeat ancillary testing, consistent with the absence of cerebral blood flow, perfusion, or electrophysiologic activity.
Natural history of infratentorial brain injury and implications for serial assessments/ancillary testing
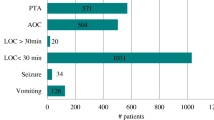
A majority of patients suspected of death by neurologic criteria following an IBI eventually progress to whole-brain death through obstructive hydrocephalus and/or venous obstruction, leading to cessation of supratentorial blood flow, perfusion, or electrical function.8,9 In a cohort of individuals who fulfilled clinical criteria for death by neurologic criteria, 12% of patients with IBI had isolated brainstem death at the time of their first ancillary test, whereas 73% of these patients had whole-brain death (unclear neurologic state in the remaining 15%). In this cohort, at least 81% of patients with an IBI eventually progressed to whole-brain death, as shown by repeat ancillary testing.8 Case reports and case series of isolated brainstem death suggest there is a high risk of progression to whole-brain death.8 Of these 38 individuals, 71% eventually progressed to whole-brain death (the delay from isolated brainstem death diagnosis to whole-brain death diagnosis was < 1 to 16 days), whereas 16% were still in apparent isolated brainstem death. The final neurologic status was unknown in 13% of cases. Importantly, there are no reported cases of patients with isolated brainstem death that regained any clinically observable signs of brain function. Figure 1 illustrates how patients with IBI may meet clinical criteria for death by neurologic criteria despite persistent cerebral blood flow, perfusion, or electrophysiologic function, and relative absence of supratentorial injury.
Patients with infratentorial brain injury may meet clinical criteria for death by neurologic criteria despite persistent cerebral blood flow, perfusion, or electrophysiologic function, and relative absence of supratentorial injury
DNC = death by neurologic criteria; EEG = electroencephalogram; SSEP = somatosensory evoked potentials
Areas of uncertainty and future work
Overall, there is significant uncertainty regarding the epidemiology of IBI among patients with suspected death by neurologic criteria. The literature pertaining to the prevalence, characteristics, and evolution of IBI among patients with suspected death by neurologic criteria is mostly composed of studies at moderate to high risk of bias.8 Furthermore, there is much variability in the target population, sampling, and investigational methods (e.g., timing and choice of ancillary test modality) in these studies, which calls into question the validity of their findings. The lack of large-scale, high-quality epidemiological data on IBI among patients with suspected death by neurologic criteria likely contributes to the ongoing debate on the appropriate approach to the determination of death by neurologic criteria among IBI patients, and this uncertainty may be compounded by variable societal, philosophical, or religious views on the construct of death. Thus, robust epidemiological research on IBI among patients with suspected death by neurologic criteria is required to better inform clinical practice.
Perhaps more importantly, the concern for potential residual consciousness in IBI patients who fulfill clinical criteria for death by neurologic criteria but have preserved supratentorial blood flow, perfusion, or neurophysiologic function is largely based on theoretical anatomic arguments. The clinical significance of ancillary test findings in these patients is currently unknown. In fact, there are no data directly supporting nor refuting residual consciousness in IBI patients who fulfill clinical criteria for death by neurologic criteria. Fundamental research is therefore required to address this area of uncertainty and investigate the potential for consciousness in this patient population. Until such research is conducted, the decision to accept or refute brainstem death as DNC is principally rooted in perceptions of the theoretical pathophysiologic mechanisms by which consciousness is abolished. Current uncertainty on these phenomena may lead to variability in clinical practice in different jurisdictions despite the absence of robust evidence clearly supporting either position.
Consensus recommendations
For patients with infratentorial brain injury suspected of death by neurologic criteria
-
1.
A clinical assessment (physical examination) is necessary but not sufficient to determine death by neurologic criteria.
-
2.
For patients initially presenting with IBI who currently or subsequently have structural neuroimaging evidence of significant supratentorial involvement, which may include but is not limited to hydrocephalus, diffuse supratentorial cerebral edema, or diffuse loss of white-grey matter differentiation, ancillary testing is not necessarily required and a clinical assessment for death by neurologic criteria is sufficient.
-
3.
If brain injury remains isolated to the brainstem without significant supratentorial involvement on structural neuroimaging (such as brain computed tomography or magnetic resonance imaging), ancillary testing is required.
-
4.
Demonstration of preserved cerebral blood flow/perfusion by ancillary testing in a patient with IBI does not fulfill the definition of death in Canada.
-
5.
In the event that ancillary testing does not support death by neurologic criteria and the clinical exam remains consistent with brain death, ancillary testing can be repeated (e.g., in 24–48 hr) to confirm death by neurologic criteria, as many patients progress to whole-brain death during this time. Alternatively, on the basis of poor prognosis, withdrawal of life sustaining measures may be considered without fulfillment of criteria for brain death.
Figure 2 summarizes the above final recommendation for patients with suspected death by neurologic criteria following a primary IBI who do not have significant supratentorial involvement on structural neuroimaging.
References
Shemie SD, Wilson LC, Hornby L, et al. A brain-based definition of death and criteria for its determination after arrest of circulation or neurologic function in Canada: a 2023 Clinical Practice Guideline. Can J Anesth 2023; https://doi.org/10.1007/s12630-023-02428-z.
Greer DM, Shemie SD, Lewis A, et al. Determination of brain death/death by neurologic criteria: the World Brain Death Project. JAMA 2020; 324: 1078–97. https://doi.org/10.1001/jama.2020.11586
Honorary Secretary. Diagnosis of brain death. Statement issued by the Honorary Secretary of the Conference of Medical Royal Colleges and their Faculties in the United Kingdom on 11 October 1976. Br Med J 1976; 2: 1187–8. https://doi.org/10.1136/bmj.2.6045.1187
Spears WE, Lewis A, Bakkar A, et al. What does brainstem death mean? A review of international protocols. Can J Anesth 2023; https://doi.org/10.1007/s12630-023-02431-4.
Omelianchuk A, Bernat J, Caplan A, et al. Revise the Uniform Determination of Death Act to align the law with practice through neurorespiratory criteria. Neurology 2022; 98: 532–6. https://doi.org/10.1212/wnl.0000000000200024
Shemie SD, Doig C, Dickens B, et al. Severe brain injury to neurological determination of death: Canadian forum recommendations. CMAJ 2006;174: S1–13. https://doi.org/10.1503/cmaj.045142
Taran S, Gros P, Gofton T, et al. The reticular activating system: a narrative review of discovery, evolving understanding, and relevance to current formulations of brain death. Can J Anesth 2023; https://doi.org/10.1007/s12630-023-02421-6.
Neves Briard J, Plourde G, Nitulescu R, et al. Infratentorial brain injury among patients suspected of death by neurologic criteria : a systematic review and meta-analysis. Neurology 2022; https://doi.org/10.1212/wnl.0000000000201449
Kramer AH, Kromm JA, Doig CJ, Chassé M, Couillard PL. Neurological determination of death following infratentorial stroke: a population-based cohort study. Can J Neurol Sci 2022; 49: 553–9. https://doi.org/10.1017/cjn.2021.177
Varelas PN, Brady P, Rehman M, et al. Primary posterior fossa lesions and preserved supratentorial cerebral blood flow: implications for brain death determination. Neurocrit Care 2017; 27: 407–14. https://doi.org/10.1007/s12028-017-0442-3
Hoffmann O, Masuhr F. Use of observational periods or ancillary tests in the determination of brain death in Germany. Eur Neurol 2015; 74: 11–7. https://doi.org/10.1159/000431089
Plourde G, Neves Briard J, Shemie SD, Shankar JJ, Chassé M. Flow is not perfusion, and perfusion is not function: ancillary testing for the diagnosis of brain death. Can J Anesth 2021: 953–61. https://doi.org/10.1007/s12630-021-01988-2
Chassé M, Neves Briard J, Yu M, et al. Clinical evaluation and ancillary testing for the diagnosis of death by neurologic criteria: a cross-sectional survey of Canadian intensivists. Can J Anesth 2022; 69: 353–63. https://doi.org/10.1007/s12630-021-02166-0
Author contributions
All authors contributed to the working group deliberation and decisions and drafting of the manuscript.
Disclosures
Dr. Shemie is a medical advisor for Canadian Blood Services (Ottawa, ON, Canada). Drs Boyd and Singh are donation physicians with Trillium Gift of Life Network (Toronto, ON, Canada). Dr. Kramer is the medical director of the Southern Alberta Organ and Tissue Donation agency (Calgary, AB, Canada).
Funding statement
Funded by Health Canada and Canadian Blood Services through the Organ Donation and Transplant Collaborative.
Prior conference presentations
Preliminary recommendations presented 24 November 2022 at the Critical Care Canada Forum (Toronto, ON, Canada).
Editorial responsibility
This submission was handled by Dr. Dale Gardiner, Guest Editor, Canadian Journal of Anesthesia/Journal canadien d’anesthésie.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Shemie, S.D., Briard, J.N., Boyd, J.G. et al. Infratentorial brain injury and death by neurologic criteria in Canada: a narrative review. Can J Anesth/J Can Anesth 70, 781–787 (2023). https://doi.org/10.1007/s12630-023-02427-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-023-02427-0