Abstract
Purpose
We aimed to describe the current literature concerning propofol misuse in medical professionals, specifically relating to the individual demographics of those misusing propofol and the outcomes of propofol misuse.
Methods
We conducted a retrospective scoping review of the literature using a modified PRISMA approach. We used MEDLINE, EMBASE, and PsycINFO databases to identify relevant studies based on search terms. Studies describing individual medical professionals misusing propofol were included.
Results
Twenty-four articles describing 88 individual cases of propofol misuse were included for data charting and analysis. Anesthesiologists and certified registered nurse anesthetists were most commonly identified. Death was a common method of identification of misuse, while rehabilitation and death were common final outcomes associated with propofol misuse.
Conclusions
Despite knowledge of the pharmacokinetic and pharmacodynamic properties of propofol by those misusing this medication, death was a common outcome reported in the literature. Data related to long-term outcomes including re-entry to clinical practice or success of rehabilitation were limited.
Résumé
Objectif
Nous avons cherché à décrire la littérature actuelle concernant l’abus de propofol chez les professionnels de la santé, en particulier en ce qui concerne les données démographiques individuelles de ceux qui abusent du propofol et les issues d’un tel abus.
Méthode
Nous avons réalisé une étude de portée rétrospective de la littérature à l’aide d’une approche PRISMA modifiée. Nous avons utilisé les bases de données MEDLINE, EMBASE et PsycINFO pour identifier les études pertinentes en fonction des termes de recherche. Les études décrivant des professionnels de la santé abusant du propofol ont été incluses.
Résultats
Vingt-quatre articles décrivant 88 cas individuels d’abus de propofol ont été inclus pour la cartographie et l’analyse des données. Les anesthésiologistes et les infirmières anesthésistes autorisées certifiées ont été le plus souvent identifiés. La mort était une méthode courante d’identification de l’abus, tandis que la réhabilitation et la mort étaient des issues finales fréquemment associées à l’abus de propofol.
Conclusion
Malgré la connaissance des propriétés pharmacocinétiques et pharmacodynamiques du propofol par ceux qui abusent de ce médicament, le décès était une issue fréquente rapportée dans la littérature. Les données relatives aux issues à long terme, y compris le retour à la pratique clinique ou le succès de la réhabilitation, étaient limitées.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Diversion and misuse of a variety of anesthetic medications have been reported in medical professionals.1, 2 Diversion can be defined as the channeling of a prescription drug to an unlawful channel of distribution or use,3 and misuse can be defined as any medication use without a prescription or in ways not intended by the prescriber.4 While many misused anesthetic medications are classified as controlled substances, the commonly used intravenous anesthetic agent propofol is not currently defined as a controlled substance by the United States Drug Enforcement Administration (DEA)5 or the Canadian Controlled Drugs and Substances Act.6 Propofol is, however, classified as a controlled substance in South Korea7 and, in the USA, in Alabama, Georgia, and North Dakota.8
While opioids often receive the most attention regarding substance misuse by medical professionals, misuse of nonopioid medications including propofol, ketamine, and inhalational anesthetics has been described.9 Increasingly, reports of propofol misuse are becoming more prevalent and should be given more attention.10, 11 This is particularly true in cases of misuse by medical professionals with easy access to propofol. Due to the lack of accountability and oversight of propofol, diversion for misuse may be easier for medical professionals to obtain than for other commonly misused controlled substances such as opioids or benzodiazepines.12 Additionally, the mortality rate associated with propofol misuse may be as high as 33%, even in persons with knowledge of the pharmacokinetics and pharmacodynamics of the medication.13
The reported rate of substance use disorder in medical professionals is 5.7%,14 with some reporting that 10–15% of all medical professionals will misuse drugs or alcohol during their career.15 As more emphasis is placed on wellness of medical professionals, consideration needs to be given to propofol misuse, particularly given its potentially fatal consequences. Identifying common themes in those misusing propofol, including baseline characteristics and outcomes, is vital in improving medical professional wellbeing.
In this scoping review, our aim was to describe the current literature regarding propofol misuse in medical professionals, specifically the individual demographics of the medical professionals identified as being involved with propofol misuse and the outcomes of those misusing propofol to identify gaps in knowledge and future areas for research.
Methods
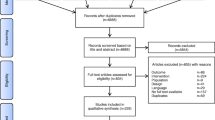
The methodology for this scoping review was developed using previously published guidelines by Arksey and O’Malley16 based on a modified Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) approach for scoping reviews (PRISMA-ScR).17 This process involves five stages for conducting a scoping review, which are described below. The PRISMA-ScR checklist can be found in the Electronic Supplementary Material eAppendix 1.
Stage 1: Identify the research question
To better evaluate propofol misuse by medical professionals, the research team developed the following research question: What individual characteristics of medical professionals misusing propofol are commonly reported in the literature and what are the reported consequences of propofol misuse?
Stage 2: Identify relevant studies
A comprehensive search strategy was used with search terms including propofol, medication misuse, medical professionals, and addiction. A full list of search terms is available in ESM eAppendix 2. Searches were conducted on 29 November 2021 within the following databases: Ovid MEDLINE (1986 to November 2021), Ovid EMBASE (1986 to November 2021), and Ovid PsycINFO (1986 to November 2021). No article type restrictions were included to obtain broad search results from a wide variety of sources. Date restrictions from 1986 to present were used to reflect the period of clinical use of propofol. Because of limitations in translation services, the search was limited to articles written in English. Reference lists of the identified sources were reviewed to identify applicable sources not found in the initial search.
Inclusion criteria for the scoping review included reports on medical professionals misusing propofol. Exclusion criteria included discussions of laypersons misusing propofol, medical professionals misusing substances other than propofol, no full-text availability, and non-English language sources.
Stage 3: Study selection
Two members of the research team independently screened publications for inclusion based on title and abstract review using a systematic review software (Covidence, Veritas Health Innovation; Melbourne, VIC, Australia). Sources deemed to be relevant by title and abstract review were screened for inclusion using a full-text review. Any disagreements were discussed until a consensus could be reached. A third reviewer was available to discuss disagreements that could not be resolved by the initial reviewers.
Stage 4: Charting the data
After the full-text review, data were extracted from relevant sources. Extracted data included the article type, country of origin, year of report, profession, trainee status, sex, age, pre-existing psychiatric disorders, polysubstance use (use of propofol in addition to other substances), method of discovery, outcome, and if the misuse was associated with suicide.
Stage 5: Synthesis of results
Analysis of identified articles including individual characteristics of medical professionals was conducted based on the previously listed data points to identify relevant themes.
Results
Details of source selection are available in Fig. 1. Twenty-one articles identified through database searches were deemed relevant to our research question, while three additional articles were identified through reference list review. Twenty-four articles were included for data charting and synthesis.10, 18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40
Data charting of the final 24 articles is available in the Table. Included articles were published between 1992 and 2021, with half of the included articles being published between 2007 and 2013 (n = 12). The most common article type was case reports (n = 17) focusing on single cases, but six included articles were case series reporting 2–25 cases of propofol misuse. One additional article meeting inclusion criteria was a survey study. Most included articles originated from Europe (n = 15), but most of the identified cases were from North America in two larger case series.
Demographics
Of the identified articles reporting age of medical professionals misusing propofol, the median [interquartile range] age was 35 [29,30,31,32,33,34,35,36,37,38,39,40,41,42,43] yr, though discrete age data were only available for approximately half of the cases. The medical professionals’ sex was approximately even when indicated (male, n = 33; female, n = 30), but was unknown in nearly one third of cases (unknown, n = 25). No articles provided information on race or ethnicity of medical professionals misusing propofol.
Medical professional occupation
Twenty-two articles provided the medical professional occupation of 85 individuals. Medical professionals identified as misusing propofol most commonly worked within the field of anesthesiology as anesthesiologists (n = 42) or as certified registered nurse anesthetists (CRNAs; n = 16). Additionally, registered nurses (n = 12) and nonanesthesiologist physicians (n = 12) were also identified as misusing propofol in the literature. Nonanesthesiology physicians’ specialties were surgery (n = 2), general practice (n = 2), critical care (n = 1), obstetrics (n = 1), emergency medicine (n = 1), radiology (n = 1) and unknown (n = 4). Figure 2 shows the full breakdown of medical professions. Only 22 of the identified cases involved trainees, but all 22 of the trainees identified as misusing propofol were noted to be anesthesiologists.
Previous psychiatric history/polysubstance use
Pre-existing psychiatric history was available in only 14 included articles spanning 59 cases. Pre-existing psychiatric disorder was noted in nearly half of the cases with available information (26 cases), but the information provided was limited in these articles. History of polysubstance use (use of substances in addition to propofol) was better reported in nearly all included articles, with one article providing partial data for identified cases. Overall, history of polysubstance use was reported in 72 cases and was present in most identified cases (n = 42).
Method of discovery/outcome
Data regarding method of discovery were available in 23 articles covering 48 cases, though these data were incomplete in one article. Among cases with a known method of discovery, death was most common (n = 38). Symptomatic intoxication (n = 6) and self-admission to rehabilitation (n = 4) were also noted methods of discovery.
Data regarding outcome of cases were available in all 24 articles, but one article included incomplete data on outcome, leaving known outcome data on 83 cases. Self-admission to rehabilitation (n = 42) and death (n = 41) were the most common outcomes. Of the 41 cases of death, association with suicide was reported in 31 cases. Suicide was associated with death in 13 cases. Information regarding subsequent recovery or resumption of clinical practice following rehabilitation was not identified.
Discussion
Propofol is the one of the most common intravenous anesthetic agents used today. When administered by a trained professional, it is a safe and effective anesthetic agent, but self-administration can have devastating consequences. Our scoping review identified 24 articles reporting on individual characteristics of propofol misuse in 88 healthcare professionals over a 30-year period. While this may seem a small number given the amount of propofol in use worldwide during this period, it should be noted that these cases likely represent the tip of a large iceberg of unreported events. It is also likely that these reports represent a sample skewed toward prevalence in academic institutions where someone might be more likely to write a report. While it appears that the incidence of propofol misuse is increasing, without a clear understanding of either the real numerator or denominator involved, we cannot estimate a rate and our findings should be viewed in this context.
Given our search criteria, it is not surprising that individual case reports were the most common article type in this review. Despite this, much of the more robust data from the included articles came from multiple larger case series and a single survey study. This shows the need for larger studies to strengthen the understanding of medical professionals who misuse propofol and identify methods to identify and mitigate propofol misuse. Despite this need for additional data, future studies may be limited to the practical difficulties of measuring the impact of interventions to prevent propofol misuse due to difficulties in determining its true incidence.
Anesthesiologists and CRNAs represented the majority of identified articles and cases. Ease of access and familiarity with how it is used may explain why the rate of propofol misuse appears to be highest in this group of healthcare professionals. Other healthcare professionals with access and familiarity made up the second highest percentage group of medical professionals, which included registered nurses and nonanesthesiologist physicians in specialties such as critical care, surgery, and emergency medicine. The findings of this scoping review provide support to focus future prevention and recognition strategies on those working within the field of anesthesiology.
Previous studies investigating substances more generally11 and propofol specifically10 have suggested that trainees represent a larger proportion of medical professionals misusing these substances. Less than half of propofol misuse cases identified in this scoping review were in trainees, and all trainees identified were anesthesiologists. Though collation of the case reports, case series, and one survey study should not be used as a reliable direct comparator with previous studies, we do recognize anesthesiology trainees as a high-risk population for propofol misuse. This finding suggests that propofol misuse may be more common in those out of training than previously believed and should be further investigated to truly understand the extent of this problem. Previous literature shows that the greatest risk for anesthesiologists and CRNAs developing addiction-related complications with misuse of anesthetic agents is early in their career.41 Focus should therefore be on preventing healthcare professionals, particularly anesthesiologists, from misusing propofol early in their career.
Death was a commonly described outcome in cases of propofol misuse identified in the literature and was similar to findings in opioid misuse.42 Most strikingly, this review found that death was a frequently reported method of discovery in cases of propofol misuse. Interpretation of this finding should be tempered as nearly half of all identified cases lacked a known method of discovery. Previous studies have shown mortality rates as high as 28% among anesthesiology attending physicians and 38% among resident physicians.10 Induction doses of propofol can cause apnea more frequently than other anesthetic agents can, even opioids.43 Rapid injection of propofol most commonly leads to death due to respiratory depression without ventilatory support and may also result in anoxic brain injury, aspiration pneumonitis, or cardiac arrest.30, 44 When self-administered or administered outside the controlled medical setting, an induction dose of this medication may provide a lethal injection as shown in this review.
It is also important to note that death related to propofol misuse and known suicide were commonly reported, though data regarding suicide was not available for a portion of articles identified in this review. Suicide risk has been shown to be elevated in healthcare professionals,45, 46 and particularly high-risk fields of medicine including specialties with access to propofol such as anesthesiology and general surgery.46 While pre-existing psychiatric history was available in only 14 of the included articles, nearly half of the individuals in these articles had a pre-existing psychiatric disorder. It is vital that all medical professionals remain vigilant and able to recognize colleagues with signs of depression or suicidality, particularly in those with access to drugs such as propofol, which is frequently used to facilitate suicide in this cohort.
There have been increasing reports of propofol misuse among medical professionals beyond the case reports and case series targeted by this scoping review. In a study including 11,666 attending physicians and resident physicians from 1990 to 1997 by Booth et al., the calculated ten-year incidence of propofol misuse was 0.02%.47 In a more recent study by Wischmeyer et al., which included 20,865 attending physicians and resident physicians, the incidence rate increased five-fold to 0.10% during the period 1995–2005.10 Most recently, Fry et al. surveyed the heads of 185 Australian and New Zealand departments of anesthesia and found that propofol was the most commonly misused drug, even when considering more traditionally misused substances such as opiates, benzodiazepines, and alcohol.11 Due to this increasingly more common incidence of propofol misuse, it is important to recognize the misuse potential of propofol.
Compared with other commonly used anesthetic agents, propofol has a rapid onset of action for induction combined with rapid recovery,43 making it an attractive target for diversion in the workplace setting. Individuals who have misused propofol reported self-administration of anesthetic or subanesthetic doses repeatedly throughout the day while still being able to function at a high enough level to avoid detection in between doses. So called “pro-napping” is associated with self-administration of a single bolus dose followed by rapid recovery and immediate return to work.48 These reports of propofol misuse while on duty raise concerns regarding patient safety while being treated by medical professionals misusing propofol.
Similar to alcohol, benzodiazepines, and barbiturates, all of which have proven addiction potential, propofol acts on γ-aminobutyric acid type A (GABAA) receptors to enhance chloride currents.44 The potentiation of GABAA receptor-mediated chloride currents by propofol occurs at low concentrations with direct activation of the GABAA receptor occurring with high concentrations of propofol.49 Antagonizing the GABAA receptor blocks the action of propofol.50 Both subanesthetic and anesthetic doses of propofol have been shown to increase the concentration of dopamine in the nucleus accumbens of rats, a main component of the mesolimbic reward process.51 This is very similar to what occurs with alcohol and other recreational drugs that stimulate dopamine release in the nucleus accumbens and further enhance activation of neural networks associated with attention and reward behavior.52 In a study conducted on baboons, these primates were shown to preferentially self-administer propofol, suggesting this medication also acts as a reinforcer.53 In a more recent study evaluating patients undergoing propofol sedation during gastrointestinal endoscopy procedures, propofol induced euphoria in nearly half of patients enrolled.54
Although propofol isn’t currently listed as a controlled substance throughout the USA or Canada, some institutions require propofol to be accounted for. Wischmeyer et al. showed that at 90 academic anesthesia programs (71% of programs in the study), the pharmacy did not securely store and account for propofol.10 This study also showed that more cases of propofol misuse were reported at programs without pharmacy control of propofol. While having stricter control on the supply of propofol in the hospital, even if propofol is not ultimately reclassified as a controlled substance (that is, treating propofol as a controlled substance) could potentially reduce the rate of diversion.
Through this scoping review, we identified several knowledge gaps regarding propofol misuse. One is the etiology for propofol misuse, an important point for identifying potential future mitigation strategies. Other gaps include the demographics of those misusing propofol, such as information on race, ethnicity, and socioeconomic background, which could be associated with propofol misuse. Another notable knowledge gap is related to re-entry to clinical practice following propofol misuse. It is unknown if those misusing propofol successfully complete rehabilitation and are able to re-enter clinical practice within their previous subspecialty or within a new subspecialty. One identified study does provide a proposed framework for re-entry to clinical practice following propofol misuse,55 but no data regarding success of this program exist. Similarly, no long-term follow-up of those who have undergone rehabilitation for propofol misuse has been reported, so it is unknown if rehabilitation prevents relapse or death. Additionally, the duration of misuse of propofol is unknown. Identifying how long those misusing propofol have been actively misusing may provide insight into opportunities to prevent diversion and misuse. Lastly, the success of potential training interventions or other prevention strategies is also unknown. While Wischmeyer et al. showed that pharmacy accountability of propofol was associated with a lower incidence of propofol misuse,10 very little additional information related to training interventions or other prevention strategies exists, including outcomes related to propofol misuse in regions where propofol is listed as a controlled substance, such as South Korea, Alabama, Georgia, and North Dakota.
Future directions of research involving propofol misuse in medical professionals should address these knowledge gaps. An anonymous database of cases to better identify risk factors and outcomes associated with propofol misuse is one possible future direction. Care to make certain a database such as this maintains confidentiality and would not be reported to authorities or governing bodies would be imperative to limit stigmatization or discouragement from self-presenting for help. This database could help provide further insight into propofol misuse and outcomes through larger data analysis, similar to what has previously been done with the Malignant Hyperthermia Hotline.56 Data from this database could be monitored over time to provide a more robust method for measuring success of interventions to prevent propofol misuse in medical professionals.
The limitations of this review should be recognized to minimize overinterpretation of our findings. We relied on reported cases in the literature, and it is possible that propofol misuse is under-reported for a number of reasons, limiting the impact of our review. Substance misuse in general still carries a significant stigma and data on death of a medical professional following an overdose of any kind are usually not publicly available. Suicide, for the same reasons, is also under-reported, and it is often difficult to distinguish between an intentional and unintentional propofol overdose because of the narrow therapeutic index of propofol. When propofol misuse causes death, there might be less inhibition (and more motivation) to publish the case reports, as opposed to when the victim survives and successfully enters treatment. Furthermore, we are unable to comment on duplicate reporting of propofol misuse between multiple articles identified because of the anonymous nature of these cases. It is possible that the same cases have been counted multiple times, particularly in articles with a case series design. Individual case reports seen in Table show no identifiable duplicate cases, but the possibility of duplicate cases should be considered when interpreting our findings.
Conclusion
Propofol misuse by medical professionals exists and in the literature is most commonly reported in anesthesiologists and CRNAs. As death is a common reported result of propofol misuse, even in medical professionals who have knowledge of the pharmacokinetic and pharmacodynamic properties of the medication, areas for future study should focus on quantifying the significance of this problem and looking for ways to identify potential interventions for at-risk populations. Possible strategies include development of an anonymous database of medical professionals known to misuse propofol or expanding the scope of search to include public records such as from law enforcement, the national death index, or records from licensing agencies relating to suspension or termination due to substance misuse-related issues.
References
Warner DO, Berge K, Sun H, Harman A, Hanson A, Schroeder DR. Substance use disorder among anesthesiology residents, 1975-2009. JAMA 2013; 310: 2289–96. https://doi.org/10.1001/jama.2013.281954
Mayall RM. Substance abuse in anaesthetists. BJA Educ 2016; 16: 236–41. https://doi.org/10.1093/bjaed/mkv054
Berge KH, Dillon KR, Sikkink KM, Taylor TK, Lanier WL. Diversion of drugs within health care facilities, a multiple-victim crime: patterns of diversion, scope, consequences, detection, and prevention. Mayo Clin Proc 2012; 87:674–82. https://doi.org/10.1016/j.mayocp.2012.03.013
Schepis TS, Klare DL, Ford JA, McCabe SE. Prescription drug misuse: taking a lifespan perspective. Subst Abuse 2020; 14: 1178221820909352. https://doi.org/10.1177/1178221820909352
Drug Enforcement Administration. Propofol (Diprivan), 2020. Available from URL: https://www.deadiversion.usdoj.gov/drug_chem_info/propofol.pdf (accessed November 2022).
Government of Canada Justice Laws. Controlled Drugs and Substances Act (S.C. 1996, c. 19), 2022. Available from URL: https://laws-lois.justice.gc.ca/eng/acts/c-38.8/ (accessed November 2022).
Kim EJ, Kim SH, Hyun YJ, et al. Clinical and psychological characteristics of propofol abusers in Korea: a survey of propofol abuse in 38, non-healthcare professionals. Korean J Anesthesiol 2015; 68: 586–93. https://doi.org/10.4097/kjae.2015.68.6.586
Gordon D, McGarry SM. Disposal and treatment of controlled substances from the OR. ASA Monit 2018; 82: 18–21.
Burnett G, Fry RA, Bryson EO. Emerging worldwide trends in substances diverted for personal non-medical use by anaesthetists. BJA Educ 2020; 20: 114–9. https://doi.org/10.1016/j.bjae.2020.01.002
Wischmeyer PE, Johnson BR, Wilson JE, et al. A survey of propofol abuse in academic anesthesia programs. Anesth Analg 2007; 105: 1066–71. https://doi.org/10.1213/01.ane.0000270215.86253.30
Fry RA, Fry LE, Castanelli DJ. A retrospective survey of substance abuse in anaesthetists in Australia and New Zealand from 2004 to 2013. Anaesth Intensive Care 2015; 43: 11–7. https://doi.org/10.1177/0310057x1504300117
Stocks G. Abuse of propofol by anesthesia providers: the case for re-classification as a controlled substance. J Addict Nurs 2011; 22: 57–62.
Drug Enforcement Administration, Department of Justice. Schedules of controlled substances: placement of propofol into schedule IV. Proposed rule. Fed Regist 2010; 75: 66195–9.
Bush DM, Lipari RN. Substance use and substance use disorder by industry, 2015. Available from URL: https://www.samhsa.gov/data/sites/default/files/report_1959/ShortReport-1959.html (accessed November 2022).
Baldisseri MR. Impaired healthcare professional. Crit Care Med 2007; 35: S106–16. https://doi.org/10.1097/01.ccm.0000252918.87746.96
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 2007; 8: 19–32. https://doi.org/10.1080/1364557032000119616
Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 2018; 169: 467–73. https://doi.org/10.7326/m18-0850
Follette JW, Farley WJ. Anesthesiologist addicted to propofol. Anesthesiology 1992; 77: 817–8. https://doi.org/10.1097/00000542-199210000-00028
Bonnet U, Harkener J, Scherbaum N. A case report of propofol dependence in a physician. J Psychoactive Drugs 2008; 40: 215–7. https://doi.org/10.1080/02791072.2008.10400634
Riezzo I, Centini F, Neri M, et al. Brugada-like EKG pattern and myocardial effects in a chronic propofol abuser. Clin Toxicol 2009; 47: 358–63. https://doi.org/10.1080/15563650902887842
Klausz G, Róna K, Kristóf I, Töro K. Evaluation of a fatal propofol intoxication due to self administration. J Forensic Leg Med 2009; 16: 287–9. https://doi.org/10.1016/j.jflm.2008.12.010
Koopmann A, von der Goltz C, Hermann D, Kiefer F. Propofol addiction initiated by anesthetic use. Am J Psychiatry 2011; 168: 211–2. https://doi.org/10.1176/appi.ajp.2010.10091293
Welliver MD, Bertrand A, Garza J, Baker K. Two new case reports of propofol abuse and a pattern analysis of the literature. Int J Adv Nurs Stud 2012; 1: 22–42.
Bonnet U, Scherbaum N. Craving dominates propofol addiction of an affected physician. J Psychoactive Drugs 2012; 44: 186–90. https://doi.org/10.1080/02791072.2012.684635
Colucci AP, Gagliano-Candela R, Aventaggiato L, et al. Suicide by self-administration of a drug mixture (propofol, midazolam, and zolpidem) in an anesthesiologist: the first case report in Italy. J Forensic Sci 2013; 58: 837–41. https://doi.org/10.1111/1556-4029.12053
Mannocchi G, Napoleoni F, Napoletano S, et al. Fatal self administration of tramadol and propofol: a case report. J Forensic Leg Med 2013; 20: 715–9. https://doi.org/10.1016/j.jflm.2013.04.003
Han E, Jung S, Baeck S, Lee S, Chung H. Deaths from recreational use of propofol in Korea. Forensic Sci Int 2013; 233: 333–7. https://doi.org/10.1016/j.forsciint.2013.10.008
Hayashi T, Buschmann C, Riesselmann B, Roscher S, Tsokos M. Circumstantial and toxicological features of deaths from self-administered intravenous anesthetic/narcotic agents. Forensic Sci Med Pathol 2013; 9: 138–44. https://doi.org/10.1007/s12024-012-9374-6
Ward CF. Substance abuse: now, and for some time to come. Anesthesiology 1992; 77: 619–22.
Earley PH, Finver T. Addiction to propofol: a study of 22 treatment cases. J Addict Med 2013; 7: 169–76. https://doi.org/10.1097/adm.0b013e3182872901
Köroğlu G, Tezcan AH. A case report of the first propofol addiction in Turkey. Turk J Anaesthesiol Reanim 2015; 43: 434–6. https://doi.org/10.5152/tjar.2015.54872
Procaccianti P, Farè F, Argo A, et al. Determination of propofol by GC/MS and fast GC/MS-TOF in two cases of poisoning. J Anal Toxicol 2017; 41: 771–6. https://doi.org/10.1093/jat/bkx056
Gwiazda S, Dixon E, Cronly M, Kavanagh Y, Cullinane M, Mulligan LM. Propofol misuse in Ireland - two case reports and a review of the literature. Forensic Sci Int 2021; 326: 110909. https://doi.org/10.1016/j.forsciint.2021.110909
Drummer OH. A fatality due to propofol poisoning. J Forensic Sci 1992; 37: 1186–9.
Chao TC, Lo DS, Chui PP, Koh TH. The first fatal 2,6-di-isopropylphenol (propofol) poisoning in Singapore: a case report. Forensic Sci Int 1994; 66: 1–7. https://doi.org/10.1016/0379-0738(94)90314-x
Soyka M, Schutz CG. Propofol dependency. Addiction 1997; 92: 1369–70. https://doi.org/10.1111/j.1360-0443.1997.tb02856.x
Iwersen-Bergmann S, Rösner P, Kühnau HC, Junge M, Schmoldt A. Death after excessive propofol abuse. Int J Legal Med 2001; 114: 248–51. https://doi.org/10.1007/s004149900129
Cirimele V, Kintz P, Doray S, Ludes B. Determination of chronic abuse of the anaesthetic agents midazolam and propofol as demonstrated by hair analysis. Int J Legal Med 2002; 116: 54–7. https://doi.org/10.1007/s004140100240
Roussin A, Mirepoix M, Lassabe G, et al. Death related to a recreational abuse of propofol at therapeutic dose range. Br J Anaesth 2006; 97: 268. https://doi.org/10.1093/bja/ael168
Kranioti EF, Mavroforou A, Mylonakis P, Michalodimitrakis M. Lethal self administration of propofol (Diprivan). A case report and review of the literature. Forensic Sci Int 2007; 167: 56–8. https://doi.org/10.1016/j.forsciint.2005.12.027
Alexander BH, Checkoway H, Nagahama SI, Domino KB. Cause-specific mortality risks of anesthesiologists. Anesthesiology 2000; 93: 922–30. https://doi.org/10.1097/00000542-200010000-00008
Bryson E. The opioid epidemic and the current prevalence of substance use disorder in anesthesiologists. Curr Opin Anaesthesiol 2018; 31: 388–92. https://doi.org/10.1097/aco.0000000000000589
Langley MS, Heel RC. Propofol. A review of its pharmacodynamic and pharmacokinetic properties and use as an intravenous anaesthetic. Drugs 1988; 35: 334–72. https://doi.org/10.2165/00003495-198835040-00002
Roussin A, Montastruc JL, Lapeyre-Mestre M. Pharmacological and clinical evidences on the potential for abuse and dependence of propofol: a review of the literature. Fundam Clin Pharmacol 2007; 21: 459–66. https://doi.org/10.1111/j.1472-8206.2007.00497.x
Hawton K, Agerbo E, Simkin S, Platt B, Mellanby RJ. Risk of suicide in medical and related occupational groups: a national study based on Danish case population-based registers. J Affect Disord 2011; 134: 320–6. https://doi.org/10.1016/j.jad.2011.05.044
Dutheil F, Aubert C, Pereira B, et al. Suicide among physicians and health-care workers: a systematic review and meta-analysis. PLoS One 2019; 14: e0226361. https://doi.org/10.1371/journal.pone.0226361
Booth JV, Grossman D, Moore J, et al. Substance abuse among physicians: a survey of academic anesthesiology programs. Anesth Analg 2002; 95: 1024–30. https://doi.org/10.1097/00000539-200210000-00043
Frost EA, Bryson EO. Propofol abuse. In: Frost EA, Bryson EO (Eds.). Perioperative Addiction: Clinical Management of the Addicted Patient, 1st ed. New York: Springer; 2012: 179–88.
Sieghart W. Structure and pharmacology of gamma-aminobutyric acidA receptor subtypes. Pharmacol Rev 1995; 47: 181–234
Bovill J, Sonner J, Zhang Y, et al. GABA(A) receptor blockade antagonizes the immobilizing action of propofol but not ketamine or isoflurane in a dose-related manner. Anesth Analg 2003; 96: 706–12. https://doi.org/10.1213/01.ane.0000048821.23225.3a
Pain L, Gobaille S, Schleef C, Aunis D, Oberling P. In vivo dopamine measurements in the nucleus accumbens after nonanesthetic and anesthetic doses of propofol in rats. Anesth Analg 2002; 95: 915–9. https://doi.org/10.1097/00000539-200210000-00022
Heinz A, Siessmeier T, Wrase J, et al. Correlation between dopamine D(2) receptors in the ventral striatum and central processing of alcohol cues and craving. Am J Psychiatry 2004; 161: 1783–9. https://doi.org/10.1176/appi.ajp.161.10.1783
Weerts EM, Ator NA, Griffiths RR. Comparison of the intravenous reinforcing effects of propofol and methohexital in baboons. Drug Alcohol Depend 1999; 57: 51–60. https://doi.org/10.1016/s0376-8716(99)00044-7
Brechmann T, Maier C, Kaisler M, et al. Propofol sedation during gastrointestinal endoscopy arouses euphoria in a large subset of patients. United European Gastroenterol J 2018; 6: 536–46. https://doi.org/10.1177/2050640617736231
Monroe T, Hamza H, Stocks G, Davies Scimeca P, Cowan R. The misuse and abuse of propofol. Subst Use Misuse 2011; 46: 1199–205. https://doi.org/10.3109/10826084.2011.564705
Garcia FJ, Litman RS, Pinyavat T. Lessons learned from calls to the MHAUS malignant hyperthermia hotline, 2021. Available from URL: https://www.apsf.org/article/lessons-learned-from-calls-to-the-mhaus-malignant-hyperthermia-hotline/ (accessed November 2022).
Author information
Authors and Affiliations
Contributions
Garrett W. Burnett, Amir Taree, and Ethan O. Bryson contributed to all aspects of this manuscript, including study conception and design; acquisition, analysis, and interpretation of data; and drafting the article. Lili Martin contributed to acquisition of data.
Corresponding author
Ethics declarations
Disclosures
The authors have no conflicts of interest to report.
Funding statement
This research was internally funded by the Department of Anesthesiology, Perioperative & Pain Medicine at the Icahn School of Medicine at Mount Sinai. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Prior conference presentations
Portions of this manuscript were previously presented at the New York State Society of Anesthesiologists’ 75th Post Graduate Assembly in Anesthesia in December 2021.
Editorial responsibility
This submission was handled by Dr. Stephan K. W. Schwarz, Editor-in-Chief, Canadian Journal of Anesthesia/Journal canadien d’anesthésie.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Burnett, G.W., Taree, A., Martin, L. et al. Propofol misuse in medical professions: a scoping review. Can J Anesth/J Can Anesth 70, 395–405 (2023). https://doi.org/10.1007/s12630-022-02382-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-022-02382-2