Abstract
Purpose
Remimazolam, an ultra-short-acting benzodiazepine, was recently approved in numerous jurisdictions as an induction drug for general anesthesia. We aimed to determine the doses of remimazolam that would allow placement of a supraglottic airway device (SGD) in 50% and 95% of nonparalyzed patients (ED50 and ED95).
Methods
In this prospective study, 30 American Society of Anesthesiology Physical Status I–II grade female patients scheduled for hysteroscopic surgery were enrolled. Anesthesia was induced with 1 μg·kg−1 of fentanyl and continuous infusion of remimazolam without neuromuscular blockade. An i-gel® SGD was inserted 2.5 min after the start of remimazolam infusion. We used Dixon’s up-and-down method and isotonic regression to determine the ED50 and ED95 of remimazolam for insertion of an SGD.
Results
Twenty-eight patients were included in the final analysis. The ED50 and ED95 of remimazolam required for successful i-gel insertion were 8.8 mg·kg−1·hr−1 (95% confidence interval [CI], 6.3 to 10.6) and 10.7 mg·kg−1·hr−1 (95% CI, 10.6 to 11.7), respectively. A nonfully relaxed jaw was found in 7/13 patients (54%) in the success group and 14/15 patients (93%) in the failure group (difference in proportions, 40%; 95% CI, 7 to 65; P = 0.02). Bucking or other movements during SGD insertion only occurred in the failure group (11/15, 73%).
Conclusion
In 95% of nonparalyzed female patients undergoing hysteroscopy, 10.7 mg·kg−1·hr−1 of remimazolam with 1 μg·kg−1 of fentanyl facilitates i-gel insertion. Remimazolam showed a high incidence of poor jaw relaxation and bucking or other movements during SGD insertion.
Study registration
Clinical Trial Registry of the Republic of Korea (KCT0006527, https://cris.nih.go.kr; registered 1 September 2021; principal investigator: Ji Seon Jeong).
Résumé
Objectif
Le remimazolam, une benzodiazépine à action ultra-brève, a récemment été approuvé dans de nombreuses juridictions comme agent d’induction pour l’anesthésie générale. Notre objectif était de déterminer les doses de remimazolam qui permettraient l’insertion d’un dispositif supraglottique (DSG) chez 50 % et 95 % des patients non paralysés (DE50 et DE95).
Méthode
Dans cette étude prospective, 30 patientes de statut physique I-II selon l’American Society of Anesthesiology devant bénéficier d’une chirurgie hystéroscopique ont été recrutées. L’anesthésie a été induite avec 1 μg·kg−1 de fentanyl et une perfusion continue de remimazolam sans bloc neuromusculaire. Un DSG i-gel® a été inséré 2,5 minutes après l’amorce de la perfusion de remimazolam. Nous avons utilisé la méthode de l’escalier de Dixon et la régression isotonique pour déterminer la DE50 et DE95 de remimazolam pour l’insertion d’un DSG.
Résultats
Vingt-huit patientes ont été incluses dans l’analyse. Les DE50 et DE95 du remimazolam requises pour une insertion réussie de l’i-gel était de 8,8 mg·kg−1·h−1 (intervalle de confiance [IC] à 95 %, 6,3 à 10,6) et 10,7 mg·kg−1·h−1 (IC 95 %, 10,6 à 11,7), respectivement. Une mâchoire non complètement détendue a été observée chez 7 patientes sur 13 (54 %) dans le groupe d’intubation réussie et chez 14/15 patientes (93 %) dans le groupe d’échec d’intubation (différence de proportions, 40 %; IC 95 %, 7 à 65; P = 0,02). Le fléchissement ou d’autres mouvements pendant l’insertion du DSG ne se sont produits que dans le groupe d’échec de l’induction (11/15, 73 %).
Conclusion
Chez 95 % des patientes non paralysées bénéficiant d’une hystéroscopie, 10,7 mg·kg−1·h−1 de remimazolam avec 1 μg·kg−1 de fentanyl ont facilité l’insertion d’un dispositif i-gel. Le remimazolam a montré une incidence élevée de mauvaise relaxation de la mâchoire et de fléchissement ou d’autres mouvements lors de l’insertion du DSG.
Enregistrement de l’étude
Registre des essais cliniques de la République de Corée (KCT0006527, https://cris.nih.go.kr; enregistrée le 1er septembre 2021; chercheur principal : Ji Seon Jeong).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Remimazolam besylate (Byfavo injection in the Republic of Korea, Byfavo™ in the USA, Anerem® in Japan, Aptimyda™ in the EU, and Ruima® in China), an ultra-short-acting benzodiazepine, was approved in the USA (in July 2020), the EU/EEA/UK (in March 2021), the Republic of Korea (in August 2021), and China (in July 2020) for procedural sedation and in Japan (in January 2020) and the Republic of Korea (in January 2021) for general anesthesia.1 It has the desirable features of rapid onset and offset of action, no injection pain, and the availability of a reversal agent.2 These features provide a chance to reconsider benzodiazepine as the principal anesthetic for general anesthesia.3 Previous studies have reported that remimazolam is just as effective as propofol, but has a slower offset without reversal and produces less hypotension and pain on injection.4 In particular, regarding reversal at the end of surgery in cirrhotic patients, remimazolam has a faster recovery and produces less hypoxia and hypotension.5 Because remimazolam is a new drug, limited data are available regarding the dosing for various clinical needs during general anesthesia. The licensed prescribing information of remimazolam specifies an initial dose of 6 or 12 mg·kg−1·hr−1 for induction of general anesthesia. Previous studies have determined the induction dose either according to the manufacturer's recommendation or with arbitrary doses not previously supported by clinical evidence.4,5,6
There are data concerning the dosing of other induction agents for placement of supraglottic airway devices (SGDs) without neuromuscular blockade (NMB). These dose requirements vary according to whether adjuvants, such as opioids or neuromuscular blocking agents, are used.7, 8 Nevertheless, no study has yet reported the optimal dose of remimazolam for successful insertion of an SGD in nonparalyzed patients. Therefore, we aimed to evaluate the effective dose of remimazolam to successfully insert an SGD in 50% and 95% (ED50 and ED95) of nonparalyzed patients who had also received fentanyl.
Methods
This study was conducted at Samsung Medical Center (Seoul, Republic of Korea), a quaternary-level university teaching hospital, and was approved by the Samsung Medical Center Institutional Review Board (IRB no. SMC 2021-06-091, 2 September 2021) and registered in the Clinical Trial Registry of the Republic of Korea on 1 September 2021 (KCT0006527, https://cris.nih.go.kr; principal investigator: Ji Seon Jeong) before recruitment of the first participant.
Study population
From 11 November 2021 to 10 December 2021, we screened consecutive adult female patients aged 19–65 yr with an American Society of Anesthesiology Physical Status of I or II who were scheduled for elective hysteroscopic surgery under general anesthesia. We obtained written informed consent from all participants before any protocol-specific procedures were performed. The study exclusion criteria were body mass index > 30 kg·m-2 or < 18.5 kg·m-2; lactation or pregnancy; severe liver disease; neuromuscular disease; mental illness; metabolic disease; drug or alcohol addiction; contraindication to benzodiazepine drugs, sevoflurane, opioid, or dextran 40 (including allergies to these drugs or a history of a hypersensitivity reaction); acute narrow-angle glaucoma; shock or coma; genetic problems such as galactose intolerance, Lapp lactase deficiency, and glucose–galactose malabsorption; and severe or acute respiratory failure.
Study protocol
No patients received premedication. After the patient arrived in the operating room, we applied standard monitors, including an electrocardiogram, noninvasive blood pressure monitor (NIBP), pulse oximetry device, end-tidal carbon dioxide, and Bispectral Index™ (BIS™; Covidien LLC, Mansfield, MA, USA) monitor. Blood pressure was monitored every minute until five minutes after insertion of an i-gel® SGD (Intersurgical, Wokingham, Berkshire, UK). At the start of preoxygenation, 1 μg·kg−1 of fentanyl was administered as a bolus. Preoxygenation was performed for at least one minute. Then, remimazolam (Byfavo; Hana Pharm Co., Ltd., Seoul, Republic of Korea) of a predetermined dose using Dixon’s up-and-down method was started using a continuous-infusion mode of the anesthesia pump (Injectomat MC Agilia; Fresenius Kabi, Bad Homburg, Hessen, Germany). Patients were asked to count from one at the initiation of remimazolam administration. When they stopped counting, their shoulders were shaken every ten seconds to verify consciousness and a loss of consciousness (LOC) was defined when the patient could not show any movement to the shoulder stimuli. When apnea appeared, ventilation was assisted using 80% oxygen and 20% air before insertion of the i-gel. An i-gel coated with a water-soluble lubricant was inserted 2.5 minutes after the start of remimazolam. An anesthesiologist (J. K.) with experience performing > 300 procedures inserted the i-gel according to the manufacturer’s instructions. The anesthetic agent was switched to sevoflurane after insertion of the SGD and titrated to keep the BIS in the range of 40–60.
Using the modified Dixon’s up-and-down method, we determined the remimazolam dose for each patient using the response of the previous patient.9 Dixon’s up-and-down methodology requires that the starting dose be the minimum dose expected to result in a positive response, which is the successful insertion of the i-gel in this case. Because of the lack of previous research on this topic, we set the remimazolam dose for the first patient at 9 mg·kg−1·hr−1, which is the median value of the induction doses recommended by the manufacturer. Depending on the response of the preceding patient, the infusion rate of remimazolam was increased or decreased by 0.6 mg·kg−1·hr−1, which is 10% of the minimum induction dose. If we judged the preceding patient’s response to be a “failure,” we increased the infusion rate by 0.6 mg·kg−1·hr−1; if we judged the preceding response to be a “success,” we decreased the dose by 0.6 mg·kg−1·hr−1. The success of placement of the SGD was determined using the Muzi score, which is a grading system modified from Scheller et al.10, 11 For the SGD, there were two categories of Muzi score: jaw mobility and coughing/movement. Jaw mobility was evaluated as follows: 1 = fully relaxed, 2 = mild resistance, 3 = tight but opens, and 4 = closed. Coughing/movement was evaluated as follows: 1 = none, 2 = one or two coughs, 3 = three or more coughs, and 4 = bucking or movement. Because the Muzi score did not specify the definition of movement, we added some practical criteria. When the movement occurred at the shoulder, hip, elbow, or knee joints, we gave a score of 4. To achieve a “success” rating for SGD placement, the scores could not exceed 2 for any of the conditions or responses. We defined a “failure” as failure to achieve LOC by 2.5 minutes after the start of remimazolam, or any Muzi score > 2 in response to device insertion.7, 11 Meanwhile, “success” was defined as the absence of the abovementioned reactions. An anesthesiologist unaware of the remimazolam dose inserted the i-gel and evaluated the insertion conditions. For the safety and comfort of the study participants, when the anesthesiologist failed to insert the i-gel, rescue sevoflurane was administrated to induce anesthesia.
From the start of administration of remimazolam until five minutes after i-gel insertion, we recorded the highest and lowest mean blood pressure and heart rate values. Hypotension was defined as a > 20% decrease in mean blood pressure compared with baseline NIBP or a mean blood pressure lower than an absolute value of 65 mm Hg.12 In case of hypotension, 5 mg of ephedrine was injected. Bradycardia was defined as a pulse rate less than 50 beats min−1 and treated at the discretion of the attending anesthesiologist. We recorded BIS before i-gel insertion and documented any events, including spontaneous ventilation, breath-holding, expiratory stridor, or tearing. All patients were interviewed in the recovery room to assess memory recall using the modified Brice questionnaire and postoperative nausea and vomiting (PONV) profile.
Sample size calculation and statistical analysis
This study was a modified Dixon’s up-and-down sequential allocation trial. According to previous studies, without calculating the exact sample size, at least 20–40 patients are required, and the study must have a stopping rule.9 Dixon’s up-and-down method requires at least six independent pairs of failure/success to reliably estimate the ED50 and ED95 of remimazolam.13 In the present study, 30 patients were collected based on Dixon’s method.
We used IBM SPSS Statistics for Windows version 27 (IBM Corp., Armonk, NY, USA) and R statistical software version 3.3.2 (R Foundation for Statistical Computing, Vienna, Austria; http://www.R-project.org/) for statistical analysis. Categorical variables are presented as numbers (%). Continuous variables with normal distribution are presented as mean (standard deviation), and those with skewed distribution are presented as median [interquartile range]. The normality of continuous data was assessed using the Shapiro–Wilk test. The ED50 and ED95 of remimazolam for successful i-gel insertion were calculated using isotonic regression.9 An adjusted response probability was calculated using the pooled adjacent-violators algorithm (PAVA).9 The 95% confidence interval (CI) for isotonic regression was estimated using the recursive algorithm by Morris for ordered-binomial point estimates.14, 15 We used paired t tests or the Wilcoxon signed-rank test to compare blood pressure and heart rate at baseline with their maximal and minimal values during the study period. We used Pearson's correlation to evaluate correlations between doses of remimazolam and time to LOC, the maximum reduction in mean blood pressure, and the maximum reduction in heart rate from baseline to the lowest value. We considered a P value less than 0.05 to indicate statistical significance.
Results
We screened 30 patients consecutively and all of them agreed to participate in this trial. Nevertheless, we excluded two patients because we found that remimazolam was administered longer than intended. Finally, we included 28 patients in the analysis based on Dixon’s method.
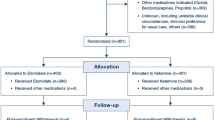
Table 1 presents the preoperative characteristics. Figures 1 and 2 show the up-and-down results in consecutive patients and the PAVA response rate, respectively. The ED50 and ED95 of remimazolam were 8.8 mg·kg−1·hr−1 (95% CI, 6.3 to 10.6) and 10.7 mg·kg−1·hr−1 (95% CI, 10.6 to 11.7 mg·kg−1·hr−1), respectively.
Data of consecutive i-gel insertion over predetermined doses of remimazolam (with the initial remimazolam being 9 mg·kg−1·hr−1 for the first patient). Six pairs of failed insertion-successful insertion sequences were used for statistical analysis with Dixon's up-and-down method. The black horizontal bars represent the mean remimazolam dose of the fail-success pairs.
Thirteen of 28 patients experienced successful insertion of the i-gel. Even in the failure group, we accomplished effective airways on the first attempt in all except two patients.
The induction and recovery profiles are presented in Table 2. Sore throat and traumatic insertion were not reported, even in the “failure” group. No patient experienced intraoperative recall even though some showed BIS values greater than 60 before i-gel insertion (16/28, 57%) and vigorous movements during i-gel insertion (11/28, 39%). A few patients (3/28, 11%) reported PONV, and two of these required antiemetics.
There was a significant reduction in blood pressure and heart rate from baseline. The mean changes in blood pressure and heart rate from baseline to the lowest values were 13.6 mmHg (95% CI, 9.1 to 18.1; P < 0.001) and 9.8 beats min−1 (95% CI, 6.3 to 13.2; P < 0.001), respectively. There was a fair correlation between the maximum decrease of mean blood pressure (%) and the infusion rate of remimazolam (r = 0.46, P = 0.01). The correlation between infusion rate of remimazolam and time to LOC was not significant (P = 0.41), nor was the mean change of heart rate (P = 0.19).
The observed parameters during i-gel insertion conditions and the number of patients who had adverse events are presented in Table 3. A nonfully relaxed jaw was found in 7/13 (54%) in the success group and 14/15 (93%) in the failure group (difference in proportions, 40%; 95% CI, 7 to 65; P = 0.02). Bucking or other movements during SGD insertion only occurred in the failure group (11/15, 73%). Significant respiratory complications, including laryngospasm, bronchospasm, regurgitation, or aspiration, did not occur in any of the patients.
Discussion
This study reports the feasibility of remimazolam as an anesthetic induction agent for SGD insertion in nonparalyzed patients. We found that with 1 μg·kg−1 of fentanyl, the ED50 and ED95 of remimazolam required for successful i-gel insertion without muscle relaxation were 8.8 and 10.7 mg·kg−1·hr−1, respectively. Remimazolam also reduced the mean blood pressure in a dose-dependent manner.
The ED50 and ED95 of remimazolam for i-gel insertion determined by this study were in the dosage range recommended by the manufacturer (6–12 mg·kg−1·hr−1). In current practice, propofol is the induction agent of choice for SGD insertion without NMB, leading to fewer pharyngeal morbidities and upper airway reflexes.16, 17 Also, it has been shown to have a relaxant effect on the jaw.18 In previous studies, nearly all nonparalyzed patients receiving propofol showed a fully relaxed jaw.19, 20 Nevertheless, in the present study, < 50% of the patients (6/13, 46%) showed a fully relaxed jaw for i-gel insertion even in the success group. Although a direct comparison is difficult, remimazolam might be less effective at providing satisfactory conditions for insertion of an SGD. Nevertheless, there was no clinically significant rigidity that made it difficult to insert the i-gel and no patients reported sore throat or experienced a traumatic insertion after the surgery. If remimazolam is contemplated for SGD use without paralysis, more research should be conducted for this use.
As a new agent, the capability to maintain blood pressure is a necessary characteristic to prevent unfavorable end-organ damage. In healthy volunteers, remimazolam had a moderate influence on blood pressure. In a surgical population, remimazolam showed a lower incidence of intraoperative hypotension (systolic blood pressure < 80 mm Hg) than propofol did.4 Nevertheless, in this study, we adopted stricter definitions for a hypotensive episode based on previous research concerning organ injury.12 We observed 13 hypotensive events among 28 patients (46%). Also, correlation analysis revealed a positive correlation between infusion rate of remimazolam and maximum reduction in mean blood pressure (%). Therefore, it is necessary to pay attention to hemodynamic compromise. The results of the hemodynamic effect need to be validated in a large number of patients.
Our study included only women, and none were smokers. According to the Apfel score predicting the risk of PONV,21 at least 39% of the patients were expected to show PONV. Nevertheless, only three (3/28, 11%) reported nausea and two required antiemetics, even though they did not receive prophylactic antiemetics. Preoperative or intraoperative intravenous midazolam has been linked to a significant decrease in overall PONV.22 As one of the benzodiazepines, remimazolam could be considered to have a similar antiemetic effect. Nevertheless, we could not draw a definitive conclusion since our sample size was small. Further evaluations about the effect of remimazolam on PONV are required.
Previous studies compared propofol requirements between different types of SGD with or without the use of opioids.7, 23, 24 The dose requirement differed according to the type of SGD and coadministration of opioid. The depth of insertion and the area of the upper airway stimulated by SGD vary depending on the shape of the SGD and the presence of a cuff.7 The i-gel airway has a relatively small contact area and its cuffless design has less airway stimulation, so the remimazolam requirement may be less than with other SGDs. In addition, the use of opioids affected the condition at the time of SGD insertion and reduced the dose requirement.7, 25, 26 In this study, we used 1 μg·kg−1 of fentanyl as a coadministered drug. We expected the dose of remimazolam required for successful insertion of SGD might exceed the maximum recommended dose without the aid of an opioid. We decided to use opioids in our study design for safety reasons. This may raise concerns that the coinduction dose of fentanyl confounded the interpretation of the ED50 and ED95 requirements of remimazolam to successfully insert the SGD.
Some limitations of our study should be noted. First, our study population was limited to relatively healthy women participants ranging in age from 33 to 65 yr undergoing hysteroscopic procedures under general anesthesia. Remimazolam requirements have been reported to decrease with increasing patient age, although sex-based differences have not yet been established.27, 28 This narrow study population limits the generalizability of the study results. Further research is required for a better understanding of remimazolam in patients with heterogeneous sex and age profiles. Second, one observer (J. K.) determined the composition of the “success” and “failure” groups, and there is a chance that a single observer might have bias. Nevertheless, we tried to make consistent judgements using an objective scoring system to reduce potential bias. Third, the time interval between the fentanyl injection and SGD insertion was not strictly controlled in all participants and the variability in the pharmacodynamic effect of fentanyl may have affected the estimation of the effective dose of remimazolam. The peak effect site concentration of fentanyl occurs 3.6 min after injection.29 We administered the fentanyl bolus at the start of preoxygenation and remimazolam infusion started after about one minute. SGD insertion was performed 2.5 minutes after remimazolam administration. Therefore, the time of SGD insertion and the time of peak effect of fentanyl would have been relatively similar. Nevertheless, it is difficult to say that the use of fentanyl produces the same response in all patients during SGD insertion. Further studies will be needed using remimazolam alone or controlling the administration time and dose of fentanyl. Fourth, our study was conducted only during the anesthesia-induction period and did not determine the dose requirement for the maintenance of general anesthesia. Despite these limitations, our findings might be helpful to generate a hypothesis and provide valuable data for future studies.
In conclusion, the ED50 and ED95 of remimazolam for successful i-gel SGD insertion in nonparalyzed female patients undergoing hysteroscopy were 8.8 and 10.7 mg·kg−1·hr−1, respectively. Remimazolam showed a high incidence of poor jaw relaxation and bucking or other movements during SGD insertion.
References
Keam SJ. Remimazolam: first approval. Drugs 2020; 80: 625–33. https://doi.org/10.1007/s40265-020-01299-8
Sneyd JR, Gambus PL, Rigby-Jones AE. Current status of perioperative hypnotics, role of benzodiazepines, and the case for remimazolam: a narrative review. Br J Anaesth 2021; 127: 41–55. https://doi.org/10.1016/j.bja.2021.03.028
Kim KM. Remimazolam: pharmacological characteristics and clinical applications in anesthesiology. Anesth Pain Med 2022; 17: 1–11. https://doi.org/10.17085/apm.21115
Morita K, Takeda J, Sakamoto A, Yamakage M, Suzuki T. Efficacy and safety of remimazolam versus propofol for general anesthesia: a multicenter, single-blind, randomized, parallel-group, phase IIb/III trial. J Anesth 2020; 34: 543–53. https://doi.org/10.1007/s00540-020-02788-6
Shi F, Chen Y, Li H, Zhang Y, Zhao T. Efficacy and safety of remimazolam tosilate versus propofol for general anesthesia in cirrhotic patients undergoing endoscopic variceal ligation. Int J Gen Med 2022; 15: 583–91. https://doi.org/10.2147/ijgm.s345390
Hirata N, Suzuki T, Morisaki H, Morimatsu H, Sakamoto A. Safety and efficacy of remimazolam in induction and maintenance of general anesthesia in high-risk surgical patients (ASA Class III): results of a multicenter, randomized, double-blind, parallel-group comparative trial. J Anesth 2020; 34: 491–501. https://doi.org/10.1007/s00540-020-02776-w
Tanaka M, Nishikawa T. Propofol requirement for insertion of cuffed oropharyngeal airway versus laryngeal mask airway with and without fentanyl: a dose‐finding study. Br J Anaesth 2003; 90: 14–20.
Cho SA, Sung TY, Cho CK, Jee YS, Kang PS. Optimal propofol dosage for i-gel® insertion in healthy paralyzed patients. Korean J Anesthesiol 2018; 71: 22–9. https://doi.org/10.4097/kjae.2018.71.1.22
Pace NL, Stylianou MP. Advances in and limitations of up-and-down methodology: a précis of clinical use, study design, and dose estimation in anesthesia research. Anesthesiology 2007; 107: 144–52. https://doi.org/10.1097/01.anes.0000267514.42592.2a
Scheller MS, Zornow MH, Saidman LJ. Tracheal intubation without the use of muscle relaxants: a technique using propofol and varying doses of alfentanil. Anesth Analg 1992; 75: 788–93. https://doi.org/10.1213/00000539-199211000-00024
Muzi M, Robinson BJ, Ebert TJ, O'Brien TJ. Induction of anesthesia and tracheal intubation with sevoflurane in adults. Anesthesiology 1996; 85: 536–43. https://doi.org/10.1097/00000542-199609000-00012
Salmasi V, Maheshwari K, Yang D, et al. Relationship between intraoperative hypotension, defined by either reduction from baseline or absolute thresholds, and acute kidney and myocardial injury after noncardiac surgery: a retrospective cohort analysis. Anesthesiology 2017; 126: 47–65. https://doi.org/10.1097/aln.0000000000001432
Lee B, Lee JR, Na S. Targeting smooth emergence: the effect site concentration of remifentanil for preventing cough during emergence during propofol-remifentanil anaesthesia for thyroid surgery. Br J Anaesth 2009; 102: 775–8. https://doi.org/10.1093/bja/aep090
Morris MD. Small-sample confidence limits for parameters under inequality constraints with application to quantal bioassay. Biometrics 1988; 44: 1083–92.
Iasonos A, Ostrovnaya I. Estimating the dose–toxicity curve in completed phase I studies. Stat Med 2011; 30: 2117–29. https://doi.org/10.1002/sim.4206
Chia YY, Lee SW, Liu K. Propofol causes less postoperative pharyngeal morbidity than thiopental after the use of a laryngeal mask airway. Anesth Analg 2008; 106: 123–6. https://doi.org/10.1213/01.ane.0000297292.84620.2c
Scanlon P, Carey M, Power M, Kirby F. Patient response to laryngeal mask insertion after induction of anaesthesia with propofol or thiopentone. Can J Anesth 1993; 40: 816–8. https://doi.org/10.1007/bf03009250
Ummenhofer WC, Kindler C, Tschalèr G, Hampl KF, Drewe J, Urwyler A. Propofol reduces succinylcholine induced increase of masseter muscle tone. Can J Anesth 1998; 45: 417–23. https://doi.org/10.1007/bf03012576
Erhan E, Ugur G, Gunusen I, Alper I, Ozyar B. Propofol—not thiopental or etomidate—with remifentanil provides adequate intubating conditions in the absence of neuromuscular blockade. Can J Anesth 2003; 50: 108–15. https://doi.org/10.1007/bf03017840
Ramaswamy AH, Shaikh SI. Comparison of dexmedetomidine-propofol versus fentanyl-propofol for insertion of laryngeal mask airway. J Anaesthesiol Clin Pharmacol 2015; 31: 217–20. https://doi.org/10.4103/0970-9185.155152
Apfel CC, Läärä E, Koivuranta M, Greim CA, Roewer N. A simplified risk score for predicting postoperative nausea and vomiting: conclusions from cross-validations between two centers. Anesthesiology 1999; 91: 693–700. https://doi.org/10.1097/00000542-199909000-00022
Grant MC, Kim J, Page AJ, Hobson D, Wick E, Wu CL. The effect of intravenous midazolam on postoperative nausea and vomiting: a meta-analysis. Anesth Analg 2016; 122: 656–63. https://doi.org/10.1213/ane.0000000000000941
Ashay NA, Wasim S, Anil TB. Propofol requirement for insertion of I-gel versus laryngeal mask airway: a comparative dose finding study using Dixon's up-and-down method. J Anaesthesiol Clin Pharmacol 2015; 31: 324–8. https://doi.org/10.4103/0970-9185.161666
Zaballos M, Bastida E, Agustí S, Portas M, Jiménez C, López-Gil M. Effect-site concentration of propofol required for LMA-Supreme™ insertion with and without remifentanil: a randomized controlled trial. BMC Anesthesiol 2015; 15: 131. https://doi.org/10.1186/s12871-015-0115-8
Park HJ, Lee JR, Kim CS, Kim SD, Kim HS. Remifentanil halves the EC50 of propofol for successful insertion of the laryngeal mask airway and laryngeal tube in pediatric patients. Anesth Analg 2007; 105: 57–61. https://doi.org/10.1213/01.ane.0000266447.23037.e4
Ang S, Cheong KF, Ng TI. Alfentanil co-induction for laryngeal mask insertion. Anaesth Intensive Care 1999; 27: 175–8. https://doi.org/10.1177/0310057x9902700208
Chae D, Kim HC, Song Y, Choi YS, Han DW. Pharmacodynamic analysis of intravenous bolus remimazolam for loss of consciousness in patients undergoing general anaesthesia: a randomised, prospective, double-blind study. Br J Anaesth 2022; 129: 49–57. https://doi.org/10.1016/j.bja.2022.02.040
Liu M, Sun Y, Zhou L, Feng K, Wang T, Feng X. The median effective dose and bispectral index of remimazolam tosilate for anesthesia induction in elderly patients: an up-and-down sequential allocation trial. Clin Interv Aging 2022; 17: 837–43. https://doi.org/10.2147/cia.s364222
Shafer SL, Varvel JR. Pharmacokinetics, pharmacodynamics, and rational opioid selection. Anesthesiology 1991; 74: 53–63. https://doi.org/10.1097/00000542-199101000-00010
Author contributions
Jeayoun Kim designed the study, collected data, interpreted data, and wrote the manuscript. Seungwon Lee designed the study, collected data, analyzed data, and gave critical revision. Youyoung Kim collected data, acquisition of data, and gave revision. Ji Seon Jeong contributed to study conception, interpreted data, and gave critical revision.
Disclosures
The authors declare no conflicts of interest.
Funding statement
This research was supported by Hana Pharm Co., Ltd., Seoul, Republic of Korea. [Grant number, PHO021529]. None of the authors has a personal financial interest in this research. The sponsor was not involved in data analysis or interpretation.
Editorial responsibility
This submission was handled by Dr. Philip M. Jones, Deputy Editor-in-Chief, Canadian Journal of Anesthesia/Journal canadien d’anesthésie.
Author information
Authors and Affiliations
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kim, J., Lee, S., Kim, Y. et al. Remimazolam dose for successful insertion of a supraglottic airway device with opioids: a dose-determination study using Dixon’s up-and-down method. Can J Anesth/J Can Anesth 70, 343–350 (2023). https://doi.org/10.1007/s12630-022-02379-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-022-02379-x