Abstract
Purpose
We sought to explore the lived experiences of a professionally diverse sample of healthcare workers (HCWs) in a single intensive care unit (ICU) serving a large and generalizable Canadian population. We aimed to understand how working during the COVID-19 pandemic affected their professional and personal lives, including their perceptions of institutional support, to inform interventions to ameliorate impacts of the COVID-19 and future pandemics.
Methods
In this qualitative descriptive study, 23 ICU HCWs, identified using convenience purposive sampling, took part in individual semistructured interviews between July and November 2020, shortly after the first wave of the pandemic in Ontario. We used inductive thematic analysis to identify major themes.
Results
We identified five major themes related to the COVID-19 pandemic: 1) communication and informational needs (e.g., challenges communicating policy changes); 2) adjusting to restricted visitation (e.g., spending less time interacting with patients); 3) staffing and workplace supports (e.g., importance of positive team dynamics); 4) permeability of professional and personal lives (e.g., balancing shift work and childcare); and 5) a dynamic COVID-19 landscape (e.g., coping with constant change). The COVID-19 pandemic contributed to HCWs in the ICU experiencing varied negative repercussions on their work environment, including staffing and institutional support, which carried into their personal lives.
Conclusion
Healthcare workers in the ICU perceived that the COVID-19 pandemic had negative repercussions on their work environment, including staffing and institutional support, as well as their professional and personal lives. Understanding both the negative and positive experiences of all ICU HCWs working during the COVID-19 pandemic is critical to future pandemic preparedness. Their perspectives will help to inform the development of mental health and wellbeing interventions to support staff during the COVID-19 pandemic and beyond.
Résumé
Objectif
Nous avons cherché à explorer les expériences vécues par un échantillon varié de travailleurs de la santé (TS) dans une seule unité de soins intensifs (USI) desservant une population canadienne vaste et généralisable. Notre objectif était de comprendre comment le travail pendant la pandémie de COVID-19 a affecté leur vie professionnelle et personnelle, y compris leurs perceptions du soutien institutionnel, afin d’éclairer les interventions visant à atténuer les impacts de la COVID-19 et des pandémies futures.
Méthode
Dans cette étude qualitative descriptive, 23 travailleurs de la santé en soins intensifs, identifiés à l’aide d’un échantillonnage raisonné de commodité, ont participé à des entrevues individuelles semi-structurées entre juillet et novembre 2020, peu après la première vague de la pandémie en Ontario. Nous avons utilisé l’analyse thématique inductive pour identifier les principaux thèmes.
Résultats
Nous avons cerné cinq grands thèmes liés à la pandémie de COVID-19 : 1) les besoins en matière de communication et d’information (p. ex., les difficultés à communiquer les changements de politiques); 2) l’adaptation aux visites restreintes (p. ex., le fait de passer moins de temps à interagir avec les patients); 3) le soutien à la dotation en personnel et au milieu de travail (p. ex., l’importance d’une dynamique d’équipe positive); 4) la perméabilité de la vie professionnelle et personnelle (p. ex., l’équilibre entre le travail en quarts et la garde des enfants); et 5) le paysage dynamique de la COVID-19 (p. ex., l’adaptation à des changements constants). La pandémie de COVID-19 a contribué à ce que les travailleurs de la santé de l’USI subissent divers impacts négatifs sur leur environnement de travail, y compris sur la dotation en personnel et le soutien institutionnel, qui se sont répercutés sur leur vie personnelle.
Conclusion
Les travailleurs de la santé de l’USI ont perçu que la pandémie de COVID-19 avait eu des répercussions négatives sur leur environnement de travail, y compris sur la dotation en personnel et le soutien institutionnel, ainsi que sur leur vie professionnelle et personnelle. Il est essentiel de comprendre les expériences négatives et positives de tous les travailleurs de la santé des soins intensifs travaillant pendant la pandémie de COVID-19 pour bien se préparer aux pandémies futures. Leurs points de vue aideront à l’élaboration d’interventions en santé mentale et en bien-être pour soutenir le personnel pendant la pandémie de COVID-19 et au-delà.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Working in an intensive care unit (ICU) is fast-paced and stressful because of high patient acuity, ethical complexities, and intense workloads.1 A recent rapid review of psychological symptoms in physicians across several clinical specialties reported varying degrees of anxiety, stress, and depression during seven infectious disease outbreaks.2 Moreover, current research shows that healthcare workers (HCWs)—those in technical, clinical (e.g., physicians, registered nurses, pharmacists, respiratory therapists, physiotherapists) and support roles (e.g., clerks, porters, sanitation)—in ICUs are at elevated risk of poor health outcomes (e.g., compassion fatigue, burnout) during public health emergencies.3,4,5,6,7,8,9 Many HCWs in Canadian ICUs have recounted traumatic events that occurred during the 2003 Severe Acute Respiratory Syndrome (SARS) epidemic.7,10,11,12 In less than one month, the COVID-19 outbreak surpassed that of SARS (an epidemic that occurred over a nine-month period) in regard to the total number of reported cases13 and broad population restrictions.14,15,16,17,18 The rapidly growing body of evidence spanning the COVID-19 pandemic highlights ongoing mental health impacts on HCWs,3,4,19,20,21,22 including high levels of distress and collective trauma.23,24,25,26 The severity of mental health impacts was moderated by increasing case numbers and the associated restrictions enacted to limit virus transmission.27 Intensive care units in particular had to adapt to real or threatened resource shortages (e.g., personal protective equipment [PPE], hospital beds, and HCWs28) and continual policy changes (e.g., limits on visitation29).
Developing a deeper understanding of the impacts of pandemics on the work and personal lives of HCWs in ICUs is essential to helping healthcare systems navigate health crises, mitigate disastrous long-term implications, and plan for future health threats.10,30 The purpose of this study was to explore the lived experiences and perspectives of a professionally diverse sample of HCWs in a single ICU serving a large and generalizable Canadian population. We aimed to describe their perceptions of their work environment and institutional support, and how their personal and professional lives have been affected by their occupation during the COVID-19 pandemic.
Methods
Study design
We conducted a qualitative descriptive study that used semistructured interviews and adhered to the Consolidated Criteria for Reporting Qualitative Research checklist31 (Electronic Supplementary Material [ESM] eTable 1). The institutional research ethics board of each investigator approved the study (Sinai Health System Research Ethics Board [REB 20-0089, approved April 2020]; Dalhousie University Research Ethics Board [#2020-5172, approved May 2020]; and University of Calgary Conjoint Health Research Ethics Board [#20-0745, approved June 2020]). Participants provided written informed consent at the time of recruitment and oral consent to participate at the time of the interview.
Participant selection
Participants were recruited from a 16-bed ICU in a single hospital serving a metropolitan area of approximately three million residents in Ontario, Canada. Participants were eligible if they were English-speaking adults (≥ 18 yr), able to provide informed consent, and worked as a HCW in the study ICU during the COVID-19 pandemic. To recruit participants within the same wave of the pandemic, we aimed to interview three to five participants comprising five common groups of HCWs at our institution for a total target of 15 to 25 participants, which included 1) allied staff (AS) (e.g., pharmacists, physiotherapists, porters, clerical, environmental service); 2) physicians in training (residents and clinical fellows, MD-Ts); 3) staff physicians (MDs); 4) registered nurses (RNs); and 5) respiratory therapists (RTs). These targets were set to balance recruitment feasibility with data saturation (the point at which no new themes were found during iterative analysis).
Two study research nurses (J. K., C. E. N.) began recruitment on 5 June 2020, approximately six weeks after the first peak of infections in Ontario.32 They randomly approached eligible HCWs in-person in the ICU between 8:00 a.m. and 5:00 p.m. Monday to Friday until data saturation was reached (23 June 2020). A member of the research team (S. S.) was able to obtain consent from and enroll 26 of the 31 HCWs (83%) approached. Another researcher (C. D.) not affiliated with the study ICU emailed consenting individuals to schedule an interview date and time; nonresponders were sent one email reminder approximately one week after the initial email. No additional follow-up was conducted.
Data collection
The primary investigators with expertise in qualitative methods (J. P. L., S. Me.) developed a single guide to conduct 15-min interviews. Content for the interview guide was identified based on the results of two cross-national questionnaires deployed in parallel by our research group surveying COVID-19 effects on hospital HCWs in Ontario26 and ICU HCWs across Canada.33 Interview questions were open-ended and focused on eliciting participant perspectives, experiences, and perceived impacts of working in the ICU during the COVID-19 pandemic. Topics included 1) protocol changes; 2) availability of and training on PPE; 3) personal and professional supports; 4) career reflections; and 5) lessons learned. We piloted the guide with two ICU RNs who were not located at the study site and were not members of the investigative team. We revised the guide (ESM eTable 2) after each pilot interview to improve conversational flow. Three women researchers (C. D., L. K., S. Mi.) trained in qualitative methods conducted the interviews via Zoom audio or telephone, based on participant preference. Researchers recorded participant demographics (age, sex, marital status, children, professional role, years in role, clinical speciality) at the end of each interview. The interviews were audio-recorded and transcribed verbatim by a third-party transcription service (Rev.com, San Francisco, CA, USA). One researcher (C. D.) assigned a unique identifier and deidentified each participant transcript to maintain confidentiality. Three participants accepted the opportunity to member check their interview transcript to ascertain that transcription of their interview was accurate. All participants received a CAD 25 Visa prepaid gift card.
Data analysis
Three researchers (A. D., S. Mi., C. D.) performed data analysis using NVivo 12 (QSR International, Burlington, VT, USA). Applying Braun and Clarke’s approach to inductive thematic analysis,34 two researchers (A. D., S. Mi.) independently reviewed a sampling of data to formulate provisional codes and categories or themes. They then came together to compare and refine codes with oversight from the third researcher (C. D.). The initial researchers (A. D., S. Mi.) independently applied codes to a small sample of complete transcripts (n = 5). The researchers’ coding was compared and discussed with the primary investigator with qualitative expertise (J. P. L.) to create a first draft of the codebook (ESM eTable 3). The researchers (A. D., S. Mi.) then analyzed five additional transcripts using both open coding (applying meaningful descriptors to the data) and axial coding (creating connections between codes), iteratively refining the codebook until all relevant ideas were included. The complete data set was then coded in duplicate (A. D., S. Mi.). Three researchers (A. D., S. Mi., C. D.) met weekly to discuss findings, including reoccurring themes, salient quotes, and connections to previous research. They assessed that no additional interviews were required to produce added information.
Results
Participants
We interviewed 23 of the 26 (88%) consenting participants between 7 July 2020 and 26 November 2020; three did not respond to our request to schedule an interview. Participant interviews lasted a median [interquartile range (IQR)] of 14 [10–17] min. Participants included five AS, five RNs, five MDs, four RTs, and four MD-Ts (Table 1). The median [IQR] age of participants was 38 [35–47] yr; about half (12/23, 53%) were female and one-third (7/23, 36%) had been in their current professional role for less than five years, albeit all RNs interviewed had worked as a nurse for over a decade. Most participants (10/17, 59%; missing data n = 6) had worked during a previous infectious disease outbreak (e.g., SARS, Influenza A virus H1N1), the greatest proportion within the AS HCW group (4/5, 80%).
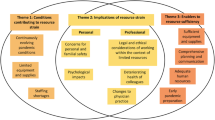
Thematic analysis
We identified five themes that captured the perspectives and experiences of ICU HCWs participating in our study: 1) communications and informational needs; 2) adjusting to restricted visitation; 3) staffing and workplace supports; 4) permeability of professional and personal lives; and 5) dynamic COVID-19 landscape. Illustrative quotations are provided in text and listed in Table 2.
Communications and informational needs
Participants shared their need to receive clear and consistent communication from hospital leadership regarding changes to visitation policies and provision of patient care. One RT (P–15) applauded their department for exceeding their informational needs, particularly as it pertained to screening and wider hospital policies. Nevertheless, this experience was not necessarily common across specialities and roles. One AS (P–19) stated that they were not consulted, hypothesizing that this was because they were not medical professionals. Participants repeatedly described that both the absence of information and contradicting information were a source of burnout and stress. One RT (P–12) articulated how stressful it was to be expected to remember all of the ever-changing policies and procedures. There was consensus that this pressure could be overwhelming at times.
Adjusting to restricted visitation
All participants acknowledged the negative impact of visitor restrictions on ICU patients and their families. Physicians were most vocal about challenges resulting from physical distancing restrictions with the families of their critically ill patients. Most physicians endorsed feeling guilty about limiting the time they spent in the patient’s room (MD, P–17). All HCWs commented that restricted visitation policies had unintended negative consequences on family caregivers, such as grief over their inadequate presence, and sparse involvement in the provision of care. One MD (P–01) shared how the healthcare team worked to communicate with family members, and the importance of providing regular updates to relatives who felt isolated from their loved one because of restricted visitation policies. Physicians shared their distress related “to deny[ing] families the right of a visit to their dying loved one” (MD, P–06), and that families were often forced to rely on technology. Physicians also described their attempts to connect patients with their families in their last moments, and their experiences with complicated grief surrounding end-of-life care (MD, P–17).
Staffing and workplace supports
All HCWs shared their perspectives on their emotional distress while working in an ICU during the COVID-19 pandemic. One AS (P–10) recalled feeling displaced and unwelcomed, encompassing a lack of belonging and hospitality. The same AS (P–10) described feeling unsupported when requests for feedback were not answered. While most participants relied on colleagues as sources of support (RT, P–12), some felt unsupported by colleagues in their work caring for critically ill patients. They described struggling to find people to deploy to the ICU as backup (MD, P–01), and the reluctance of some coworkers to cover their clinical areas because of fears of catching the virus (AS, P–14).
In contrast, some participants described successful efforts by management to ensure adequate staffing and workplace support (RN, P–20). One RT also described how the decision to up-staff their department provided additional support, ensuring enough time given to each patient (RT, P–16). Participants also remarked that access to psychological therapy and open discussions regarding mental health helped to alleviate distress and enhanced perceptions on the value that was placed on their occupational wellbeing (MD, P–05).
Permeability of professional and personal lives
Participants shared that the COVID-19 pandemic blurred the boundaries between their professional and personal lives, with boundaries being rapidly effaced. The safety of family and friends was of utmost concern and participants in our study reduced chances of exposure at all costs (RN, P–20). Reconciling responsibility and risk was difficult for all and one MD described how challenging this was for families, explaining how his loved ones grappled with a desire to be supportive of his professional work while also being unwilling to risk his personal safety (MD, P–06). The COVID-19 pandemic was especially burdensome to HCW families with young children at home, forcing parents to juggle full-time childcare with work responsibilities. This was not only difficult logistically but also challenged family dynamics; for example, as one parent’s work was prioritized over the other’s (MD-T, P–04). Many HCWs also described stigma they experienced from friends outside of the ICU. Some participants described feeling like their friends were avoiding them, contributing to a sense of isolation (RN, P–21). An additional experience felt collectively among HCWs was unease with being depicted as a healthcare hero. They discussed feeling like the title was “unfounded” (MD, P–01), describing the hero-narrative as “propaganda” (MD-T, P–03).
A dynamic COVID-19 landscape
Healthcare workers working in the ICU during the COVID-19 pandemic perceived their experiences as complex and highly stressful. One RN (P–22) remembered feeling anxiety before the pandemic was declared because HCWs were faced with many unknowns regarding transmission. An AS (P–19) described their distress at witnessing public citizens disregarding health guidelines, articulating how this made them question their desire to work in a hospital. Participants shared their experiences with having to process continually changing policies while providing patient care, explaining that anxiety levels dropped somewhat after having patients in the ICU as they were able to visualize what care was needed, eliminating a fear of the unknown (MD-T, P–17).
Nevertheless, it was difficult to establish a routine in the ICU as policies and procedures were constantly evolving (AS, P–14). Some found the changing policies distressing not only for the patient’s safety but also their own (MD-T, P–02). Overall, most HCWs agreed the pandemic noticeably affected their roles, but several commented that they felt more comfortable as time went on (RN, P–23).
Discussion
We conducted a semistructured interview-based study to explore perspectives of HCWs in one ICU on the impact of the COVID-19 pandemic on their work environment, institutional support, and their professional and personal lives. Our findings indicate that practices to control the spread of SARS-CoV-2 changed the provision of care in the ICU, which transformed the way HCWs contributed to the care of critically ill patients. Across professions, HCWs highlighted increased collegiality and teamwork that enhanced respect and mutual support, which may have helped protect against stress related to the increasingly blurred boundaries between their personal and professional lives. Restricted visitation policies in the ICU led to complex situations that had communication and emotional consequences for HCWs, for example, when restricting family members from visiting their loved ones. The unintended negative outcomes of the COVID-19 pandemic on some HCWs hinged on the notion that, despite significant cooperation among colleagues, some HCWs felt excluded by other members of the ICU care team.
Adequate social support promotes wellbeing and prevents burnout,9,35 and social support networks in the workplace enhance mental capacity, particularly in the face of traumatic experiences.36 Our data align with those of earlier reports, showing that all HCWs in the ICU require a safe and supportive workplace to provide quality patient care37,38 because of the uncontrollable nature of acute and critical illness.39 Dedicated efforts to enhance the culture and collegiality of the ICU environment, including formal psychological support40,41,42,43 during the COVID-19 pandemic and beyond, may build mental resiliency and safeguard against fatigue and burnout in ICU HCWs.44
Providing support to family members of ICU patients is central to the practice of critical care medicine,45,46 and has been more challenging in the COVID-19 pandemic.38,47 While some institutions banned visitors altogether, the restricted visitation policies enacted in our institution in response to the COVID-19 pandemic were similar to mandated policies at other Canadian48,49 and American50,51 institutions. They often required families of patients to choose who would visit their loved one and who would stay behind,44,52 increasing distress among families and challenging HCWs to effectively communicate critical information to loved ones.52 Intensive care unit visitation restrictions placed an overwhelming mental health toll on HCWs,35,38 who grappled with fatigue while comforting dying, often isolated patients, navigating unfamiliar virtual modalities, and caring for their own colleagues who fell ill.6,53 Previous work found that insomnia, anxiety, depression, post-traumatic stress disorder, and burnout were prevalent among HCWs in ICUs throughout the pandemic.38,54,55 Transformative change in the ICU may include establishing care principles to ease the emotional burden of ICU HCWs during times of restricted visitation.56 Our findings will complement research on the impact of the COVID-19 pandemic on patients and families and will help to inform HCWs and organizations about how to better care for patients, with attention to promoting patient- and family-centered care.6,57
The COVID-19 pandemic necessitated reengineering the workplace environment, which affected not only the provision of services but also the general culture of the ICU.58 Most research to date has reported on short-term impacts of the COVID-19 pandemic on HCWs, and has rarely included the perspectives of a professionally diverse sample of HCWs (i.e., including nonclinical staff). Longer-term consequences of the pandemic are unknown.39,59,60,61 Additional communication for HCWs in ICUs that emphasizes transparency, respect, humanization, and dignity62 might come in the form of long-term support plans delivered by ICU policy liaison teams to help facilitate communication between HCWs and patients’ families.63,64,65,66 As well, policy liaison teams for HCWs and psychologists available for mental health support may help to ameliorate the impact on ICU HCWs during the COVID-19 pandemic and beyond.29,67 Past research has also highlighted the value of providing training courses along with sufficient PPE to help reduce anxiety around viral transmission felt by HCWs concerned about infecting their loved ones.38,57 Digital transformation for bridging gaps in connection,52 particularly regarding the emergence of remote monitoring technologies,56 is an attractive area for future research. Widespread adoption of things like telemedicine68 and the use of artificial intelligence as a diagnostic tool69 would help make healthcare more accessible to Canadians.
Our study has several strengths including an interview guide codesigned with a PhD researcher and clinician and pilot tested with critical care nurses. We sampled participants across a variety of occupations and conducted interviews individually. This allowed HCWs time and space to share their perspectives and offer important insights on the challenges and psychological burden they experienced.
There are limitations to consider when interpreting the findings of our study. First, the study sample was dependent on the availability of frontline HCWs in the ICU during the pandemic. This might have resulted in selection bias toward individuals with more time and perhaps better mental health. Second, we only sent one reminder as we were cautious to not overburden individuals already under increased personal and professional strain. For these reasons, it is possible that important perspectives were missed. Third, this was a single-center qualitative study with 23 HCWs; although the statistical generalizability (whether the results from a representative sample of participants can be applied to a wider population or different contexts of these findings) of our findings is limited,70 alignment with earlier research3,26 suggests good transferability (the extent to which results can be applicable in other contexts/ situations/times/populations).71 Finally, our small sampling frame was not diverse enough to explore the role of sociocultural factors (e.g., gender, ethnicity) or additional professional factors (e.g., work experience) in ICU HCW’s experiences. The extensive damage inflicted by historical pandemics on society, the economy, and health was due to characteristics of the pathogen and lack of public health resources at the time. These risks are not comparable with those posed by the COVID-19 pandemic; these risks arise not from the pathogen, but rather from indirect effects of control measures on health and core societal activities.
Conclusion
Healthcare workers in the ICU perceived that the COVID-19 pandemic had negative repercussions on their work environment, including staffing and institutional support, as well as their professional and personal lives. Continually changing institutional policies meant that ICU HCWs had to care for critically ill patients while understanding and adapting to policies that changed the way they contributed to the care of critically ill patients. Further research with larger and more diverse samples of ICU HCWs is required to validate these findings.
References
Marshall JC, Bosco L, Adhikari NK, et al. What is an intensive care unit? A report of the task force of the World Federation of Societies of Intensive and Critical Care Medicine. J Crit Care 2017; 37: 270–6. https://doi.org/10.1016/j.jcrc.2016.07.015
Fiest KM, Parsons Leigh J, Krewulak KD, et al. Experiences and management of physician psychological symptoms during infectious disease outbreaks: a rapid review. BMC Psychiatry 2021; 21: 91. https://doi.org/10.1186/s12888-021-03090-9
Ardebili ME, Naserbakht DM, Colleen D, Alazmani-Noodeh F, Hakimi H, Ranjbar H. Healthcare providers experience of working during the COVID-19 pandemic: a qualitative study. Am J Infect Control 2021; 49: 547–54. https://doi.org/10.1016/j.ajic.2020.10.001
Baldwin S, George J. Qualitative study of UK health professionals' experiences of working at the point of care during the COVID-19 pandemic. BMJ Open 2021; 11: e054377. https://doi.org/10.1136/bmjopen-2021-054377
De Kock JH, Latham HA, Leslie SJ, et al. A rapid review of the impact of COVID-19 on the mental health of healthcare workers: implications for supporting psychological well-being. BMC Public Health 2021; 21: 104. https://doi.org/10.1186/s12889-020-10070-3
Mehta S, Machado F, Kwizera A, et al. COVID-19: a heavy toll on health-care workers. Lancet Respir Med 2021; 9: 226–8. https://doi.org/10.1016/s2213-2600(21)00068-0
Maunder R. The experience of the 2003 SARS outbreak as a traumatic stress among frontline healthcare workers in Toronto: lessons learned. Philos Trans R Soc Lond B Biol Sci 2004; 359: 1117–25. https://doi.org/10.1098/rstb.2004.1483
Shaukat N, Ali DM, Razzak J. Physical and mental health impacts of COVID-19 on healthcare workers: a scoping review. Int J Emerg Med 2020; 13: 40. https://doi.org/10.1186/s12245-020-00299-5
Alharbi J, Jackson D, Usher K. Compassion fatigue in critical care nurses. An integrative review of the literature. Saudi Med J 2019; 40: 1087–97. https://doi.org/10.15537/smj.2019.11.24569
Maunder RG, Lancee WJ, Balderson KE, et al. Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerg Infect Dis 2006; 12: 1924–32. https://doi.org/10.3201/eid1212.060584
Koh D, Lim MK, Chia SE, et al. Risk perception and impact of severe acute respiratory syndrome (SARS) on work and personal lives of healthcare workers in Singapore: what can we learn? Med Care 2005; 43: 676–82. https://doi.org/10.1097/01.mlr.0000167181.36730.cc
Rankin J. Godzilla in the corridor: the Ontario SARS crisis in historical perspective. Intensive Crit Care Nurs 2006; 22: 130–7. https://doi.org/10.1016/j.iccn.2005.10.001
Hewings-Martin Y. How do SARS and MERS compare with COVID-19? 2020. Available from URL: https://www.medicalnewstoday.com/articles/how-do-sars-and-mers-compare-with-covid-19 (accessed October 2022).
Capano G, Howlett M, Jarvis DS, Ramesh M, Goyal N. Mobilizing policy (in)capacity to fight COVID-19: understanding variations in state responses. Policy Soc 2020; 39: 285–308. https://doi.org/10.1080/14494035.2020.1787628
Cheng V, Wong SC, Chuang V, et al. The role of community-wide wearing of face mask for control of coronavirus disease 2019 (COVID-19) epidemic due to SARS-CoV-2. J Infect 2020; 81: 107–14. https://doi.org/10.1016/j.jinf.2020.04.024
Delen D, Eryarsoy E, Davazdahemami B. No place like home: cross-national data analysis of the efficacy of social distancing during the COVID-19 pandemic. JMIR Public Health Surveill 2020; 6: e19862. https://doi.org/10.2196/19862
Fafard P, Wilson LA, Cassola A, Hoffman SJ. Communication about COVID-19 from Canadian provincial chief medical officers of health: a qualitative study. CMAJ Open 2020; 8: E560–7. https://doi.org/10.9778/cmajo.20200110
Government of Canada. Summary of evidence supporting COVID-19 public health measures, 2021. Available from URL: https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/health-professionals/public-health-measures-mitigate-covid-19.html (accessed October 2022).
Chen Q, Liang M, Li Y, et al. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry 2020; 7: e15–6. https://doi.org/10.1016/s2215-0366(20)30078-x
da Silva FC, Barbosa CP. The impact of the COVID-19 pandemic in an intensive care unit (ICU): psychiatric symptoms in healthcare professionals. Prog Neuropsychopharmacol Biol Psychiatry 2021; 110: 110299. https://doi.org/10.1016/j.pnpbp.2021.110299
Huang JZ, Han MF, Luo TD, Ren AK, Zhou XP. Mental health survey of 230 medical staff in a tertiary infectious disease hospital for COVID-19 [Chinese]. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi 2020; 38: 192–5.
Kentish-Barnes N, Morin L, Cohen-Solal Z, Cariou A, Demoule A, Azoulay E. The lived experience of ICU clinicians during the coronavirus disease 2019 outbreak: a qualitative study. Crit Care Med 2021; 49: e585–97. https://doi.org/10.1097/ccm.0000000000004939
Janiri D, Carfì A, Kotzalidis GD, et al. Posttraumatic stress disorder in patients after severe COVID-19 infection. JAMA Psychiatry 2021; 78: 567–9. https://doi.org/10.1001/jamapsychiatry.2021.0109
Stanley BL, Zanin AC, Avalos BL, Tracy SJ, Town S. Collective emotion during collective trauma: a metaphor analysis of the COVID-19 pandemic. Qual Health Res 2021; 31: 1890–903. https://doi.org/10.1177/10497323211011589
Demertzis N, Eyerman R. Covid-19 as cultural trauma. Am J Cult Sociol 2020; 8: 428–50. https://doi.org/10.1057/s41290-020-00112-z
Honarmand K, Yarnell CY, Young-Ritchie C, et al. Personal, professional, and psychological impact of the COVID-19 pandemic on hospital workers: a cross-sectional survey. PLoS One 2022; 17: e0263438. https://doi.org/10.1371/journal.pone.0263438
Haldane V, De Foo C, Abdalla SM, et al. Health systems resilience in managing the COVID-19 pandemic: lessons from 28 countries. Nat Med 2021; 27: 964–80. https://doi.org/10.1038/s41591-021-01381-y
Parsons Leigh J, Kemp LG, de Grood C, et al. A qualitative study of physician perceptions and experiences of caring for critically ill patients in the context of resource strain during the first wave of the COVID-19 pandemic. BMC Health Serv Res 2021; 21: 374. https://doi.org/10.1186/s12913-021-06393-5
Moss SJ, Krewulak KD, Stelfox HT, et al. Restricted visitation policies in acute care settings during the COVID-19 pandemic: a scoping review. Crit Care 2021; 25: 347. https://doi.org/10.1186/s13054-021-03763-7
Shreffler J, Petrey J, Huecker M. The impact of COVID-19 on healthcare worker wellness: a scoping review. West J Emerg Med 2020; 21: 1059–66. https://doi.org/10.5811/westjem.2020.7.48684
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 2007; 19: 349–57. https://doi.org/10.1093/intqhc/mzm042
Krusina A, Chen O, Varela LO, et al. Developing a data integrated COVID-19 tracking system for decision-making and public use. International Journal of Population Data Science 2020; 5. https://doi.org/10.23889/ijpds.v5i1.1389
Mehta S, Yarnell CY, Shah S, et al. The impact of the COVID-19 pandemic on intensive care unit workers: a nationwide survey. Can J Anesth 2022; 69: 472–84. https://doi.org/10.1007/s12630-021-02175-z
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006; 3: 77–101. https://doi.org/10.1191/1478088706qp063oa
Li L, Ruan H, Yuan WJ. The relationship between social support and burnout among ICU nurses in Shanghai: a cross-sectional study. Chin Nurs Res 2015; 2: 45–50. https://doi.org/10.1016/j.cnre.2015.04.003
Labrague LJ. Psychological resilience, coping behaviours and social support among health care workers during the COVID-19 pandemic: a systematic review of quantitative studies. J Nurs Manag 2021; 29: 1893–905. https://doi.org/10.1111/jonm.13336
Rosen MA, DiazGranados D, Dietz AS, et al. Teamwork in healthcare: key discoveries enabling safer, high-quality care. Am Psychol 2018; 73: 433–50. https://doi.org/10.1037/amp0000298
Mortensen CB, Zachodnik J, Caspersen SF, Geisler A. Healthcare professionals’ experiences during the initial stage of the COVID-19 pandemic in the intensive care unit: a qualitative study. Intensive Crit Care Nurs 2022; 68: 103130. https://doi.org/10.1016/j.iccn.2021.103130
Eftekhar Ardebili M, Naserbakht M, Bernstein C, Alazmani-Noodeh F, Hakimi H, Ranjbar H. Healthcare providers experience of working during the COVID-19 pandemic: a qualitative study. Am J Infect Control 2021; 49: 547–54. https://doi.org/10.1016/j.ajic.2020.10.001
Landa-Ramírez E, Domínguez-Vieyra NA, Hernández-Nuñez ME, Díaz-Vásquez LP, Santana-García IA. Psychological support during COVID-19 death notifications: clinical experiences from a hospital in Mexico. Psychol Trauma 2020; 12: 518–20. https://doi.org/10.1037/tra0000679
Lissoni B, Del Negro S, Brioschi P, et al. Promoting resilience in the acute phase of the COVID-19 pandemic: psychological interventions for intensive care unit (ICU) clinicians and family members. Psychol Trauma 2020; 12: S105–7. https://psycnet.apa.org/doi/https://doi.org/10.1037/tra0000802
Viaux S, Maurice P, Cohen D, Jouannic JM. Giving birth under lockdown during the COVID-19 epidemic. J Gynecol Obstet Hum Reprod 2020; 49: 101785. https://doi.org/10.1016/j.jogoh.2020.101785
Tomlin J, Dalgleish-Warburton B, Lamph G. Psychosocial support for healthcare workers during the COVID-19 pandemic. Front Psychol 2020; 11: 1960. https://doi.org/10.3389/fpsyg.2020.01960
Labrague LJ, De Los Santos JA. COVID-19 anxiety among front-line nurses: predictive role of organisational support, personal resilience and social support. J Nurs Manag 2020; 28: 1653–61. https://doi.org/10.1111/jonm.13121
Davidson JE, Aslakson RA, Long AC, et al. Guidelines for family-centered care in the neonatal, pediatric, and adult ICU. Crit Care Med 2017; 45: 103–28. https://doi.org/10.1097/ccm.0000000000002169
Brown SM, Azoulay E, Benoit D, et al. The practice of respect in the ICU. Am J Respir Crit Care Med 2018; 197: 1389–95. https://doi.org/10.1164/rccm.201708-1676cp
Andrist E, Clarke RG, Harding M. Paved with good intentions: hospital visitation restrictions in the age of coronavirus disease 2019. Pediatr Crit Care Med 2020; 21: e924–6. https://doi.org/10.1097/pcc.0000000000002506
Alberta Health Services. AHS COVID-19 provincial guidance for designated support and visitor access in acute, ambulatory and emergency/urgent care. Available from URL: https://www.albertahealthservices.ca/assets/healthinfo/ipc/hi-ipc-covid19-infosht-visiting-pts-pandemic.pdf (accessed October 2022).
Fraser Health Authority. Visitor guidelines during COVID-19, 2022. Available from URL: https://www.fraserhealth.ca/health-topics-a-to-z/coronavirus/accessing-fraser-health-services/visitor-guidelines#.YM05ny1b1mA (accessed October 2022).
University of Michigan Health. Family and visitors, 2022. Available from URL: https://www.mottchild ren.org/mott-patient-visitor-guide/family-visitors (accessed October 2022).
New York Presbyterian Hospital. Patient safety: general visitation guidelines, 2022. Available from URL: https://www.nyp.org/coronavirus-information/coronavirus-visitor-policy-change (accessed October 2022).
Wendlandt B, Kime M, Carson S. The impact of family visitor restrictions on healthcare workers in the ICU during the COVID-19 pandemic. Intensive Crit Care Nurs 2022; 68: 103123. https://doi.org/10.1016/j.iccn.2021.103123
Romero-García M, Delgado-Hito P, Gálvez-Herrer M, et al. Moral distress, emotional impact and coping in intensive care unit staff during the outbreak of COVID-19. Intensive Crit Care Nurs 2022; 70: 103206. https://doi.org/10.1016/j.iccn.2022.103206
Azoulay E, Pochard F, Reignier J, et al. Symptoms of mental health disorders in critical care physicians facing the second COVID-19 wave: a cross-sectional study. Chest 2021; 160: 944–55. https://doi.org/10.1016/j.chest.2021.05.023
Azoulay E, De Waele J, Ferrer R, et al. Symptoms of burnout in intensive care unit specialists facing the COVID-19 outbreak. Ann Intensive Care 2020; 10: 110. https://doi.org/10.1186/s13613-020-00722-3
Arabi YM, Azoulay E, Al-Dorzi HM, et al. How the COVID-19 pandemic will change the future of critical care. Intensive Care Med 2021; 47: 282–91. https://doi.org/10.1007/s00134-021-06352-y
Raphael JL, Kessel W, Patel M. Unintended consequences of restrictive visitation policies during the COVID-19 pandemic: implications for hospitalized children. Pediatr Res 2021; 89: 1333–5. https://doi.org/10.1038/s41390-021-01439-0
Lord H, Loveday C, Moxham L, Fernandez R. Effective communication is key to intensive care nurses' willingness to provide nursing care amidst the COVID-19 pandemic. Intensive Crit Care Nurs 2021; 62: 102946. https://doi.org/10.1016/j.iccn.2020.102946
Stall NM, Johnstone J, McGeer AJ, Dhuper M, Dunning J, Sinha SK. Finding the right balance: an evidence-informed guidance document to support the re-opening of canadian nursing homes to family caregivers and visitors during the coronavirus disease 2019 Pandemic. J Am Med Dir Assoc 2020; 21: 1365–70. https://doi.org/10.1016/j.jamda.2020.07.038
Tupper SM, Ward H, Parmar J. Family presence in long-term care during the COVID-19 pandemic: call to action for policy, practice, and research. Can Geriatr J 2020; 23: 335–9. https://doi.org/10.5770/cgj.23.476
Zeh RD, Santry HP, Monsour C, et al. Impact of visitor restriction rules on the postoperative experience of COVID-19 negative patients undergoing surgery. Surgery 2020; 168: 770–6. https://doi.org/10.1016/j.surg.2020.08.010
Adams JG, Walls RM. Supporting the health care workforce during the COVID-19 global epidemic. JAMA 2020; 323: 1439–40. https://doi.org/10.1001/jama.2020.3972
Belli LF. Recommendations for communicating bad news by phone during the SARS-CoV-2 pandemic [Spanish]. Rev Panam Salud Publica 2020; 44: e69. https://doi.org/10.26633/rpsp.2020.69
Griffin KM, Karas MG, Ivascu NS, Lief L. Hospital preparedness for COVID-19: a practical guide from a critical care perspective. Am J Respir Crit Care Med 2020; 201: 1337–44. https://doi.org/10.1164/rccm.202004-1037cp
Janssen DJA, Ekström M, Currow DC, et al. COVID-19: guidance on palliative care from a European Respiratory Society international task force. Eur Respir J 2020; 56: 2002583. https://doi.org/10.1183/13993003.02583-2020
Honarmand K, Mehta S. Consequences of visitor restriction policies in the intensive care unit during the COVID-19 pandemic. Can J Anesth 2021; 68: 1465–70. https://doi.org/10.1007/s12630-021-02048-5
Larkin H. Navigating attacks against health care workers in the COVID-19 era. JAMA 2021; 325: 1822–4. https://doi.org/10.1001/jama.2021.2701
Nittari G, Savva D, Tomassoni D, Tayebati SK, Amenta F. Telemedicine in the COVID-19 era: a narrative review based on current evidence. Int J Environ Res Public Health 2022; 19: 5101. https://doi.org/10.3390/ijerph19095101
Bohr A, Memarzadeh K. The rise of artificial intelligence in healthcare applications. Artif Intell Health 2020; 25–60. https://doi.org/10.1016/B978-0-12-818438-7.00002-2
Smith B. Generalizability in qualitative research: misunderstandings, opportunities and recommendations for the sport and exercise sciences. Qual Res Sport Exerc Health 2018; 10: 137–49. https://doi.org/10.1080/2159676X.2017.1393221
Korstjens I, Moser A. Series: practical guidance to qualitative research. Part 4: trustworthiness and publishing. Eur J Gen Pract 2018; 24: 120–4. https://doi.org/10.1080/13814788.2017.1375092
Author contributions
Sangeeta Mehta and Jeanna Parsons Leigh conceived of the study. All authors contributed to the study design. Sara J. Mizen, Alexandra Dodd, and Chloe de Grood conducted the analyses. Sara J. Mizen, Stephana Julia Moss, Rebecca Brundin-Mather, and Jeanna Parsons Leigh prepared the initial manuscript draft. All authors substantively revised the manuscript.
Acknowledgements
We would like to thank Jessica Kayitesi and Catherine Eta-Ndu for recruiting participants, and Laryssa Kemp for helping to conduct participant interviews.
Disclosures
The authors declare that they have no competing interests.
Funding statement
This work was supported by the Canadian Institutes of Health Research Canadian 2019 Novel Coronavirus (COVID-2019) Rapid Research Funding Opportunity – Operating Grant (grant number RN420046–439965) to Jeanna Parsons Leigh. The funders had no role in the study design or in the submission of this manuscript. They did not take part in the collection or analysis of data or in the assessment of outcomes.
Editorial responsibility
This submission was handled by Dr. Stephan K. W. Schwarz, Editor-in-Chief, Canadian Journal of Anesthesia/Journal canadien d’anesthésie.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Parsons Leigh, J., Mizen, S.J., Moss, S.J. et al. A qualitative descriptive study of the impact of the COVID-19 pandemic on staff in a Canadian intensive care unit. Can J Anesth/J Can Anesth 70, 384–394 (2023). https://doi.org/10.1007/s12630-022-02377-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-022-02377-z