Abstract
Purpose
Older critically ill patients with COVID-19 have been the most vulnerable during the ongoing pandemic, with men being more prone to hospitalization and severe disease than women. We aimed to explore sex-specific differences in treatment and outcome after intensive care unit (ICU) admission in this cohort.
Methods
We performed a sex-specific analysis in critically ill patients ≥ 70 yr of age with COVID-19 who were included in the international prospective multicenter COVIP study. All patients were analyzed for ICU admission and treatment characteristics. We performed a multilevel adjusted regression analysis to elucidate associations of sex with 30-day mortality.
Results
A total of 3,159 patients (69.8% male, 30.2% female; median age, 75 yr) were included. Male patients were significantly fitter than female patients as determined by the Clinical Frailty Scale (fit, 67% vs 54%; vulnerable, 14% vs 19%; frail, 19% vs 27%; P < 0.001). Male patients more often underwent tracheostomy (20% vs 14%; odds ratio [OR], 1.57; P < 0.001), vasopressor therapy (69% vs 62%; OR, 1.25; P = 0.02), and renal replacement therapy (17% vs 11%; OR, 1.96; P < 0.001). There was no difference in mechanical ventilation, life-sustaining treatment limitations, and crude 30-day mortality (50% male vs 49% female; OR, 1.11; P = 0.19), which remained true after adjustment for disease severity, frailty, age and treatment limitations (OR, 1.17; 95% confidence interval, 0.94 to 1.45; P = 0.16).
Conclusion
In this analysis of sex-specific treatment characteristics and 30-day mortality outcomes of critically ill patients with COVID-19 ≥ 70 yr of age, we found more tracheostomy and renal replacement therapy in male vs female patients, but no significant association of patient sex with 30-day mortality.
Study registration
www.ClinicalTrials.gov (NCT04321265); registered 25 March 2020).
Résumé
Objectif
Les patients âgés gravement malades atteints de la COVID-19 ont été les plus vulnérables pendant la pandémie actuelle, les hommes étant plus sujets à l’hospitalisation et aux maladies graves que les femmes. Nous avons cherché à explorer les différences spécifiques au sexe dans le traitement et les devenirs après l’admission à l’unité de soins intensifs (USI) dans cette cohorte.
Méthode
Nous avons effectué une analyse spécifique au sexe chez des patients gravement malades âgés de ≥ 70 ans atteints de COVID-19 qui ont été inclus dans l’étude prospective multicentrique internationale COVIP. Tous les patients ont été analysés pour connaître les détails de leur admission à l’USI et les caractéristiques de leur traitement. Nous avons réalisé une analyse de régression ajustée à plusieurs niveaux pour élucider les associations entre le sexe et la mortalité à 30 jours.
Résultats
Au total, 3159 patients (69,8 % d’hommes, 30,2 % de femmes; âge médian, 75 ans) ont été inclus. Les patients de sexe masculin étaient significativement plus en forme que les patientes, tel que déterminé par l’échelle de fragilité clinique (bonne santé, 67 % vs 54 %; vulnérables, 14 % vs 19 %; fragiles, 19 % vs 27 %; P < 0,001). Les patients de sexe masculin ont plus souvent bénéficié d’une trachéostomie (20 % vs 14 %; rapport de cotes [RC], 1,57; P < 0,001), d’un traitement vasopresseur (69 % vs 62 %; RC, 1,25; P = 0,02) et d’un traitement substitutif de l’insuffisance rénale (17 % vs 11 %; RC, 1,96; P < 0,001). Il n’y avait aucune différence en matière de ventilation mécanique, de limites des traitements de maintien en vie et de mortalité brute à 30 jours (50 % d’hommes vs 49 % de femmes; RC, 1,11; P = 0,19), ce qui est demeuré le cas après ajustement pour tenir compte de la gravité de la maladie, de la fragilité, de l’âge et des limites du traitement (RC, 1,17 ; intervalle de confiance à 95 %, 0,94 à 1,45; P = 0,16).
Conclusion
Dans cette analyse des caractéristiques de traitement spécifiques au sexe et des résultats de mortalité à 30 jours des patients gravement malades atteints de COVID-19 de ≥ 70 ans, nous avons noté un nombre plus élevé de trachéotomies et de traitements substitutifs de l’insuffisance rénale chez les hommes vs les femmes, mais aucune association significative entre le sexe des patients et la mortalité à 30 jours.
Enregistrement de l’étude
www.ClinicalTrials.gov (NCT04321265); enregistré le 25 mars 2020.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The ongoing COVID-19 pandemic poses serious challenges to patients and healthcare systems worldwide. Older patients ≥ 70 yr of age have been disproportionally affected by COVID-19 with severe disease courses and a high risk of mortality.1
Since the beginning of the pandemic, data from across the world have identified patient characteristics associated with risk for adverse clinical outcomes of COVID-19. Age, male sex, comorbidities,2 and severity of disease course3 have been identified as prognostic factors. Nevertheless, data on their validity in older patients with critical illness remain limited. Frailty and associated factors might have an additional important impact on prognosis.4
Prior to the COVID-19 pandemic, patient sex had not been associated with mortality in large observational registries of unselected critically ill patients.5,6 Nevertheless, studies focusing on older patient populations found that male sex was a risk factor for adverse outcomes,7,8 as is also the case in COVID-19.9 Exploring patient sex as a risk factor in older critically ill patients with COVID-19 may thus have implications for treatment and prognosis of the most vulnerable patient subgroup. We hypothesized that older male patients with severe COVID-19 may have a worse prognosis than females.
The COVIP study is an international prospective multicenter study of critically ill patients ≥ 70 yr of age with COVID-19 treated in an intensive care unit (ICU). In this analysis from its database, we aimed to explore sex-specific treatment characteristics and clinical outcomes in critically ill patients with COVID-19 and hypothesized that there are sex-specific differences in treatment and lower mortality in female patients in this population.
Methods
Study design
This work is a secondary analysis of the international prospective multicenter COVIP study, which was initiated on 19 March 2020, and recruited COVID-19 patients ≥ 70 yr admitted to an ICU. The COVIP study was conducted by the Very Old Intensive Care Patients (VIP) project within the European Society of Intensive Care Medicine (www.vipstudy.org) in 376 ICUs in 44 countries, where the study protocol and case report forms are available to download. Ethical approval by an institutional review board was mandatory for study participation in each country. Patients were included after informed consent and consented to publication upon study inclusion. The study was registered at www.ClinicalTrials.gov (ID: NCT04321265; 25 March 2020) and adhered to the European Union General Data Privacy Regulation directive, which is implemented in most participating countries. The study intentionally allowed for coenrolment of study patients in other COVID-19 studies. Other analyses have been previously published from the COVIP database (e.g., the impact of frailty on survival4).
Study population
Each participating center included consecutive patients aged 70 yr or older with COVID-19 (confirmed by a positive SARS-CoV-2 polymerase chain reaction result) at admission to the ICU. Each patient was only included once in the study, regardless of possible readmission, transfer to another ICU, etc. In case of a patient transfer or readmission, data were summed up within a single case, which resulted in a unique electronic database record per patient. Other than duration of symptoms and duration of hospitalization, pre-ICU disease course and possible pre-ICU triage due to resource shortage during pandemic surges were not specifically recorded. The reference date was day 1 of the first ICU admission with all consecutive time points relative to this date.
Data collection
Centers collected data on patient baseline characteristics, ICU admission characteristics, ICU disease course, and clinical outcomes using a uniform electronic case report form (eCRF). No direct patient identifying characteristics like name or other ID were registered in the database. As described previously,10 the eCRF and database runs on secure servers composed and stored in Aarhus University, Denmark. These servers were operated in cooperation between the Information Technology Department and the Department of Clinical Medicine at the University.
Prior diagnoses of diabetes (any type), ischemic heart disease, chronic renal insufficiency (creatinine clearance < 60 mL·min-1), arterial hypertension (any grade), pulmonary disease (any type), and chronic heart failure (any type) were recorded. The frailty level prior to hospital admission for COVID-19 was assessed using the English version of the Clinical Frailty Scale (CFS),11 classifying patients into nine classes from very fit to terminally ill. Patients were grouped as fit (CFS of 1–3), vulnerable (CFS of 4), and frail (CFS of 5–9) for data analysis. The Sequential Organ Failure Assessment (SOFA) score on ICU admission was calculated either manually or using an online calculator in the eCRF as described previously.10,11 Type and duration of organ support were recorded in detail regarding noninvasive and invasive mechanical ventilation, prone positioning, tracheostomy, vasopressor therapy, and renal replacement therapy.
Clinical outcome assessment
The primary endpoint was survival assessed at 30 days after ICU admission, which was either assessed directly from the hospital administration system, or in follow-up by telephone. Secondary outcomes were disease-specific variables of noninvasive ventilation, intubation, tracheostomy, prone positioning, vasopressor therapy, renal replacement therapy, and limitation of life-sustaining therapies such as withholding or withdrawing treatments, which were documented according to international recommendations.12
Statistical analysis
All statistical computations were performed using Stata/BE 17.0 for Mac (Intel 64-bit; StataCorp LLC, College Station, TX, USA). Patients included in the COVIP study between 19 March 2020, and 4 February 2021, were analyzed and grouped into male or female. Patients with missing data for sex or 30-day mortality were excluded, and other missing data were handled using listwise deletion (Electronic Supplementary Material [ESM], eTable 1). Sex-subgroup differences regarding baseline characteristics, ICU admission characteristics, ICU disease course, and clinical outcomes were analyzed. Continuous variables are reported as medians with interquartile range (IQR), and categorical variables as counts with % of total or respective sex subgroup. Normal distribution of continuous variables was empirically tested using the Shapiro–Wilk and Kolmogorov–Smirnov tests. Comparisons were performed using Mann–Whitney U tests (for non-normally distributed variables) and Student’s t tests (normally distributed variables). Categorical variables were compared using Chi-square tests.
Three sequential multilevel logistic regression models were used to evaluate the associations of patient sex with ICU disease course and clinical outcomes. Included variables were selected based on previous literature and our own clinical experience—a detailed description is given in ESM eTable 1. First, a baseline model with male sex as a fixed effect and effects of the singular specific ICU site as a random effect (model 1) was fitted, which corrected for possible bias (recruitment/treatment) on an ICU level that may have occurred between the many countries/ICUs that participated in COVIP. An additional analysis of model 1 was performed to analyze subgroups for sex differences (ESM eFig. 1) on data only adjusted for ICU effects (model 1). Second, adjustment for patient and ICU admission characteristics (age, SOFA score, and frailty; model 2) were added to model 1. Third, adjustment for management strategies (treatment withhold/withdrawal; model 3) were added to model 2. Model 1 and model 2 were used to evaluate the subgroup-specific primary and secondary outcomes, whereas model 3 was only used to evaluate the primary outcome. Odds ratios (ORs) with 95% confidence intervals (CIs) are reported. Sex-specific marginal predicted means for 30-day mortality according to SOFA and CFS scoring at ICU admission were calculated and graphically analyzed. All statistical tests were two-sided, and P < 0.05 was considered statistically significant.
Results
Patient population
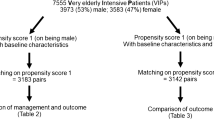
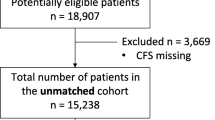
A total of 3,159 critically ill COVID-19 patients were included in this analysis of the COVIP study (Table 1). Details on missing data are provided in ESM eTable 1. Patients were more frequently male (n = 2,205; 69.8%). Median [IQR] age at admission was 75 [72–78] yr and did not differ by sex (P = 0.52).
The following comorbidities were present: arterial hypertension (2,112/3,159; 67%), diabetes mellitus (1,162/3,159; 37%), cardiovascular disease (733/3,159; 23%), chronic pulmonary disease (700/3,159; 22%), chronic kidney disease (541/3,159; 17%), and chronic heart failure (455/3,159; 14%). Male patients had significantly more often cardiovascular disease (27% vs 15%; P < 0.001) and chronic heart failure (16% vs 12%; P = 0.02).
ICU admission characteristics
The median SOFA score at ICU admission was 5 (IQR 3–8), and there was a small but statistically significant difference in SOFA score distribution (P = 0.01) with more severe disease in males. Male patients were significantly fitter at ICU admission than female patients according to CFS (fit: 67% vs 54%; vulnerable 14% vs 19%; frail 19% vs 27%; P < 0.01). Duration of COVID-19 associated symptoms before ICU admission was longer in male patients (7 (IQR 4–10) days vs 6 (IQR 3–9) days; P = 0.02). There was no difference in duration of hospitalization before ICU admission between sexes (Table 2).
ICU treatment characteristics
Sex-specific differences in treatment characteristics were recorded (Table 2). While there was no difference in noninvasive ventilation, the following were significantly more frequent in male patients: mechanical ventilation (1,574/2,205, 72% vs 640/954, 67%; P = 0.01), tracheostomy (439/2,205, 20% vs 130/954, 14%; P < 0.001), and prone positioning (852/2,205, 55% vs 301/954, 48%; P = 0.01). Additionally, male patients were more often given vasopressor therapy (1,513/2,205, 69% vs 588/954, 62%; P < 0.001) and renal replacement therapy (382/2,205, 17% vs 100/954, 11%; P < 0.001).
Regarding limitation of life-sustaining treatments, there was no difference between male and female patients in treatment withholding (631/2,205, 29% vs 254/954, 27%; P = 0.22); however, treatment withdrawal was significantly more common in male patients (427/2,205, 20% vs 154/954, 16%; P = 0.03).
Clinical outcomes
Thirty-day mortality (Table 2) was 50% in male and 49% in female patients (P = 0.75).
Marginal predicted means of 30-day mortality (ESM eFig. 2) according to SOFA and CFS scoring at ICU admission showed a linear increase in mortality with increasing SOFA or CFS.
Multilevel adjusted regression analysis
Details on 30-day mortality and adjustment variables included in the models are given in Table 3 and ESM eTable 2: When adjusting the analysis for the ICU level only (model 1), we found significantly higher odds for tracheostomy (OR, 1.57; 95% CI, 1.27 to 1.95; P < 0.001), vasopressor therapy (OR, 1.25; 95% CI, 1.04 to 1.51; P = 0.02) and renal replacement therapy (OR, 1.96; 95% CI, 1.57 to 2.25; P < 0.001) in male vs female patients. In additional subgroup analyses (ESM eFig. 1), there was a higher risk for mortality (OR ≥ 1) in male vs female patients who were classified as fit (OR, 1.35; 95% CI, 1.09 to 1.69), who were < 80 yr of age (OR, 1.22; 95% CI, 1.03 to 1.43) and in patients with > seven days after symptom onset (OR, 1.51; 95% CI, 1.20 to 2.06). When adjusting the model (model 2) for age, disease severity at ICU admission (SOFA score), and patient frailty (CFS), only tracheostomy (OR, 1.49; 95% CI, 1.17 to 1.88; P = 0.001) and renal replacement therapy (OR, 1.94; 95% CI, 1.49 to 2.51; P < 0.001) were significantly associated with male sex. Additionally, the model found higher 30-day mortality (OR, 1.24; 95% CI, 1.03 to 1.49; P = 0.03) in male vs female patients; however, when additionally adjusting for treatment limitations (Table 3, model 3), this difference in 30-day mortality was no longer statistically significant (OR, 1.17; 95% CI, 0.94 to 1.45; P = 0.16).
Discussion
We present here an analysis of sex-specific treatment characteristics and clinical outcomes in critically ill COVID-19 patients ≥ 70 yr of age from the international multicenter COVIP database. We found (1) a higher prevalence of male sex and slightly greater severity of illness at ICU admission; (2) more tracheostomy and renal replacement therapy in male patients; and (3) no difference between sexes in 30-day mortality.
Patient factors including age, comorbidities,2,13,14 and frailty4,10 as well as disease severity3,15,16 are drivers of short-term mortality in critical illness—with and without COVID-19. Differentiating sex-specific effects in this conundrum of interdependent factors has been challenging in the past: Valentin et al. found no difference in illness-adjusted mortality rates between 25,998 critically ill male (58%) vs female patients6 from Austria, despite more intensive ICU treatment in male patients. At an age cut-off of 45 yr, Samuelsson et al. found no difference in prognosis between sexes in 127,254 patients (57% male) from Sweden, but men also used more ICU resources than women did.5
Nevertheless, more advanced age may have impact on sex-specific prognosis of critical illness, as studies focusing on older (rather than unselected) patients in the ICU found other results. In an analysis from combined data from the VIP1 and VIP2 studies, Wernly et al.8 found higher 30-day mortality in male vs female patients over 80 yr of age after matching and adjusting for baseline characteristics and ICU management. In the FROG-ICU (French and European Outcome reGistry in Intensive Care Units) study, Hollinger et al. found a survival advantage in a subgroup analysis of female patients > 63 yr of age, while there was no difference between sexes in the overall cohort.7 These data hint at an age-dependent effect of patient sex on outcome of critical illness.
In studies of critically ill older patients with COVID-19, 60–70% of patients were male4,17—despite females accounting for a majority of the elderly patients in developed countries. An analysis of over three million global cases of COVID-19 by Peckham et al.9 found a strong worldwide association of male sex with need for ICU treatment (OR, 2.84) and risk of death from COVID-19 (OR, 1.39), despite no difference in the sex-specific risk of contracting COVID-19. In a propensity-score matched analysis of 14,712 patients from the multinational TriNetX network,18 male sex was significantly associated with death from COVID-19, independent of the level of comorbidities.
This increased severity of illness in male patients with COVID-19 may be reflected in the recruitment of critically ill patients in the COVIP study (70% male). We recognized more cardiovascular comorbidities in male patients (Table 1), which was found to be associated with mortality.2 We also found more tracheostomy and renal replacement therapy in male patients than in female patients. Even though the crude differences are small between sexes, these findings confirm previous data on treatment intensity in male compared with female critically ill elderly patients, and extend them to COVID-19, without showing an association with 30-day mortality. Thus, no significant effect of sex on mortality from COVID-19 was detectable during ICU treatment of patients ≥ 70 yr of age. This could be because the excess mortality from COVID-19 in males was determined prior to ICU admission, which highlights the importance of preventive measures and effective early treatments prior to critical illness, especially in men.
Frailty is recognized as an important prognostic factor in critically ill older patients with and without COVID-19. In the VIP2 study, frailty was independently associated with short-term mortality.11 Similarly, six-month mortality in patients > 80 yr with sepsis was predicted by age, SOFA score, and frailty.19,20 In a recent analysis from the COVIP study,4 we confirmed frailty to be associated with lower survival also in COVID-19. Hewitt et al. found frailty to predict COVID-19 outcomes better than either age or comorbidities.21 In the COVIP study, frailty correlated just as well with 30-day mortality as the initial SOFA score at admission (ESM eFig. 2) in both sexes; interestingly, frailty was slightly but significantly lower in male vs female patients, despite worse outcomes in male patients. This is certainly a point that deserves more research.
This is the first and largest primary analysis of sex-specific therapy and 30-day mortality in patients with COVID-19 ≥ 70 yr of age, as the patient group most severely challenged by the ongoing pandemic. A large sample size and high-quality data from prospective assessment in the international COVIP study allowed multilevel adjusted analyses for detection of small sex-dependent effects on treatment intensity and outcomes. Nevertheless, several study limitations of the design need to be considered. The COVIP study does not provide data on pre-ICU triage and admission decisions, which may have introduced bias due to patient selection for ICU admission. Treatment characteristics were recorded as binary variables (yes/no), which may not reflect disease course in all patients appropriately. Standards of care including pharmacological therapies (antivirals, immunomodulators, vaccines, etc.) may have changed during the time of the study; however, this was not assessed in COVIP. Also, no information on ICU recruitment characteristics, occurrence and length of COVID-19 waves with impact on pre-ICU triage, healthcare capacity and healthcare use, data quality, treatment quality, treatment intensity, etc., was available for inclusion in the models. In model 2 and model 3, including the SOFA score as a covariate to adjust for disease severity bears risk for overfitting of treatment variables included in the score (vasopressors, ventilation, renal failure). Because of the design of this analysis, P values were not adjusted for multiple testing.
Conclusion
In this analysis of sex-specific treatment characteristics and 30-day mortality outcomes of critically ill patients with COVID-19 ≥ 70 yr of age, we found a higher prevalence of male sex and more tracheostomy and renal replacement therapy in male patients than in female patients, but no significant association of patient sex with 30-day mortality.
References
Yanez ND, Weiss NS, Romand JA, Treggiari MM. COVID-19 mortality risk for older men and women. BMC Public Health 2020; 20: 1742. https://doi.org/10.1186/s12889-020-09826-8
Gupta S, Hayek SS, Wang W, et al. Factors associated with death in critically ill patients with coronavirus disease 2019 in the US. JAMA Intern Med 2020; 180: 1436–47. https://doi.org/10.1001/jamainternmed.2020.3596
Darmon M, Dumas G. Anticipating outcomes for patients with COVID-19 and identifying prognosis patterns. Lancet Infect Dis 2021; 21: 744–5. https://doi.org/10.1016/s1473-3099(21)00073-6
Jung C, Flaatten H, Fjølner J, et al. The impact of frailty on survival in elderly intensive care patients with COVID-19: the COVIP study. Crit Care 2021; 25: 149. https://doi.org/10.1186/s13054-021-03551-3
Samuelsson C, Sjöberg F, Karlström G, Nolin T, Walther SM. Gender differences in outcome and use of resources do exist in Swedish intensive care, but to no advantage for women of premenopausal age. Crit Care 2015; 19: 129. https://doi.org/10.1186/s13054-015-0873-1
Valentin A, Jordan B, Lang T, Hiesmayr M, Metnitz PG. Gender-related differences in intensive care: a multiple-center cohort study of therapeutic interventions and outcome in critically ill patients. Crit Care Med 2003; 31: 1901–7. https://doi.org/10.1097/01.ccm.0000069347.78151.50
Hollinger A, Gayat E, Féliot E, et al. Gender and survival of critically ill patients: results from the FROG-ICU study. Ann Intensive Care 2019; 9: 43. https://doi.org/10.1186/s13613-019-0514-y
Wernly B, Bruno RR, Kelm M, et al. Sex-specific outcome disparities in very old patients admitted to intensive care medicine: a propensity matched analysis. Sci Rep 2020; 10: 18671. https://doi.org/10.1038/s41598-020-74910-3
Peckham H, de Gruijter NM, Raine C, et al. Male sex identified by global COVID-19 meta-analysis as a risk factor for death and ITU admission. Nat Comm 2020; 11: 6317. https://doi.org/10.1038/s41467-020-19741-6
Flaatten H, De Lange DW, Morandi A, et al. The impact of frailty on ICU and 30-day mortality and the level of care in very elderly patients (≥ 80 years). Intensive Care Med 2017; 43: 1820–8. https://doi.org/10.1007/s00134-017-4940-8
Guidet B, de Lange DW, Boumendil A, et al. The contribution of frailty, cognition, activity of daily life and comorbidities on outcome in acutely admitted patients over 80 years in European ICUs: the VIP2 study. Intensive Care Med 2020; 46: 57–69. https://doi.org/10.1007/s00134-019-05853-1
Guidet B, Hodgson E, Feldman C, et al. The Durban World Congress Ethics Round Table Conference Report: II. Withholding or withdrawing of treatment in elderly patients admitted to the intensive care unit. J Crit Care 2014; 29: 896–901. https://doi.org/10.1016/j.jcrc.2014.08.004
Docking R, Mackay A, Williams C, Lewsey J, Kinsella J, Booth M. Comorbidity and intensive care outcome — a multivariable analysis. J Intensive Care Soc 2014; 15: 205–12.
Simpson A, Puxty K, McLoone P, Quasim T, Sloan B, Morrison DS. Comorbidity and survival after admission to the intensive care unit: a population-based study of 41,230 patients. J Intensive Care Soc 2021; 22: 143–51. https://doi.org/10.1177/1751143720914229
Keegan MT, Gajic O, Afessa B. Severity of illness scoring systems in the intensive care unit. Crit Care Med 2011; 39: 163–9. https://doi.org/10.1097/ccm.0b013e3181f96f81
Lambden S, Laterre PF, Levy MM, Francois B. The SOFA score—development, utility and challenges of accurate assessment in clinical trials. Crit Care 2019; 23: 374. https://doi.org/10.1186/s13054-019-2663-7
Blomaard LC, van der Linden CMJ, van der Bol JM, et al. Frailty is associated with in-hospital mortality in older hospitalised COVID-19 patients in the Netherlands: the COVID-OLD study. Age Ageing 2021; 50: 631–40. https://doi.org/10.1093/ageing/afab018
Alkhouli M, Nanjundappa A, Annie F, Bates MC, Bhatt DL. Sex differences in case fatality rate of COVID-19: insights from a multinational registry. Mayo Clin Proc 2020; 95: 1613–20. https://doi.org/10.1016/j.mayocp.2020.05.014
Haas LEM, Boumendil A, Flaatten H, et al. Frailty is associated with long-term outcome in patients with sepsis who are over 80 years old: results from an observational study in 241 European ICUs. Age Ageing 2021; 50: 1719–27. https://doi.org/10.1093/ageing/afab036
Ibarz M, Boumendil A, Haas LEM, et al. Sepsis at ICU admission does not decrease 30-day survival in very old patients: a post-hoc analysis of the VIP1 multinational cohort study. Ann Intensive Care 2020; 10: 56. https://doi.org/10.1186/s13613-020-00672-w
Hewitt J, Carter B, Vilches-Moraga A, et al. The effect of frailty on survival in patients with COVID-19 (COPE): a multicentre, European, observational cohort study. Lancet Public Health 2020; 5: e444–51. https://doi.org/10.1016/s2468-2667(20)30146-8
Author contributions
The COVIP study group is part of the Very Old Intensive Care Patients (VIP) project by the European Society of Intensive Care Medicine (ESICM) and is conducted by an international steering committee, in which all authors contribute to study conduct and Christian Jung serves as principal investigator. This specific analysis was conceived and designed by Christian Jung, Bernhard Wernly, and Georg Wolff; Bernhard Wernly performed primary statistical analyses; Georg Wolff, Bernhard Wernly, and Christian Jung analyzed and interpreted the data and drafted the manuscript; all authors interpreted the data and critically revised the manuscript. All authors read and approved the submitted version of the manuscript.
Disclosures
All authors declare no support from any industry for the submitted work; no financial relationships with any organizations that might have an interest in the submitted work in the previous three years; and no other relationships or activities that could appear to have influenced the submitted work. Joerg C. Schefold reports grants (full departmental disclosure) from Orion Pharma, Abbott Nutrition International, B. Braun Medical AG, CSEM AG, Edwards Lifesciences Services GmbH, Kenta Biotech Ltd, Maquet Critical Care AB, Omnicare Clinical Research AG, Nestle, Pierre Fabre Pharma AG, Pfizer, Bard Medica S.A., Abbott AG, Anandic Medical Systems, Pan Gas AG Healthcare, Bracco, Hamilton Medical AG, Fresenius Kabi, Getinge Group Maquet AG, Dräger AG, Teleflex Medical GmbH, Glaxo Smith Kline, Merck Sharp and Dohme AG, Eli Lilly and Company, Baxter, Astellas, Astra Zeneca, CSL Behring, Novartis, Covidien, Philips Medical, Phagenesis Ltd, Prolong Pharmaceuticals, and Nycomed outside the submitted work. The money went into departmental funds. No personal financial gain applied.
Funding statement
The study is supported in France by a grant from Fondation Assistance Publique-Hôpitaux de Paris pour la recherche. In Norway, the study is supported by a grant from the Health Region West. In addition, the study was supported by a grant from the European Open Science Cloud (EOSC). EOSCsecretariat.eu has received funding from the European Union's Horizon Programme call H2020-INFRAEOSC-05-2018-2019, grant agreement number 831644. The first author was supported by the Forschungskommission of the Medical Faculty of the Heinrich-Heine-University Düsseldorf (No. 2018-32 for a Clinician Scientist Track).
Editorial responsibility
This submission was handled by Dr. Donald E. G. Griesdale, Associate Editor, Canadian Journal of Anesthesia/ Journal canadien d’anesthésie.
Data availability statement
Additional data and materials are available upon request to the corresponding author.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The COVIP study group (https://www.vipstudy.org; covip@med.uni-duesseldorf.de) is part of the Very Old Intensive Care Patients (VIP) project by the European Society of Intensive Care Medicine (ESICM).
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Wolff, G., Wernly, B., Flaatten, H. et al. Sex-specific treatment characteristics and 30-day mortality outcomes of critically ill COVID-19 patients over 70 years of age—results from the prospective COVIP study. Can J Anesth/J Can Anesth 69, 1390–1398 (2022). https://doi.org/10.1007/s12630-022-02304-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-022-02304-2