Abstract
Purpose
The optimal noninvasive modality for oxygenation support in COVID-19-associated hypoxemic respiratory failure and its association with healthcare worker infection remain uncertain. We report here our experience using high-flow nasal oxygen (HFNO) as the primary support mode for patients with COVID-19 in our institution.
Methods
We conducted a single-centre historical cohort study of all COVID-19 patients treated with HFNO for at least two hours in our university-affiliated and intensivist-staffed intensive care unit (Jewish General Hospital, Montreal, QC, Canada) between 27 August 2020 and 30 April 2021. We report their clinical characteristics and outcomes. Healthcare workers in our unit cared for these patients in single negative pressure rooms wearing KN95 or fit-tested N95 masks; they underwent mandatory symptomatic screening for COVID-19 infection, as well as a period of asymptomatic screening.
Results
One hundred and forty-two patients were analysed, with a median [interquartile range (IQR)] age of 66 [59–73] yr; 71% were male. Patients had a median [IQR] Sequential Organ Failure Assessment Score of 3 [2–3], median [IQR] oxygen saturation by pulse oximetry/fraction of inspired oxygen ratio of 120 [94–164], and a median [IQR] 4C score (a COVID-19-specific mortality score) of 12 [10–14]. Endotracheal intubation occurred in 48/142 (34%) patients, and overall hospital mortality was 16%. Barotrauma occurred in 21/142 (15%) patients. Among 27 symptomatic and 139 asymptomatic screening tests, there were no cases of HFNO-related COVID-19 transmission to healthcare workers.
Conclusion
Our experience indicates that HFNO is an effective first-line therapy for hypoxemic respiratory failure in COVID-19 patients, and can be safely used without significant discernable infection risk to healthcare workers.
Résumé
Objectif
La modalité non invasive optimale pour le soutien en oxygène lors d’insuffisance respiratoire hypoxémique liée à la COVID-19 et son association avec l’infection des travailleurs de la santé restent incertaines. Nous rapportons ici notre expérience avec l’utilisation de canules nasales à haut débit (CNHD) comme principale modalité de soutien pour les patients atteints de COVID-19 dans notre établissement.
Méthode
Nous avons mené une étude de cohorte historique monocentrique de tous les patients atteints de COVID-19 traités par CNHD pendant au moins deux heures dans notre unité de soins intensifs affiliée à l’université et dotée d’intensivistes (Hôpital général juif, Montréal, QC, Canada) entre le 27 août 2020 et le 30 avril 2021. Nous rapportons leurs caractéristiques cliniques et leurs résultats. Les travailleurs de la santé de notre unité ont soigné ces patients dans des chambres individuelles à pression négative en portant des masques KN95 ou N95 ajustés; ils ont subi un dépistage symptomatique obligatoire de l’infection à la COVID-19, ainsi qu’un dépistage en période asymptomatique.
Résultats
Cent quarante-deux patients ont été analysés, avec un âge médian [écart interquartile (ÉIQ)] de 66 [59-73] ans; 71 % étaient des hommes. Les patients avaient un score SOFA (Sequential Organ Failure Assessment) médian [ÉIQ] de 3 [2, 3], un ratio médian [ÉIQ] de saturation en oxygène par oxymétrie de pouls/fraction d’oxygène inspiré de 120 [94-164], et un score 4C (un score de mortalité spécifique à la COVID-19) médian [ÉIQ] de 12 [10–14]. Dans l’ensemble, 48/142 patients (34 %) ont reçu une intubation endotrachéale, et la mortalité hospitalière globale était de 16 %. Un barotraumatisme est survenu chez 21/142 (15 %) patients. Parmi les 27 tests de dépistage symptomatiques et 139 tests asymptomatiques, aucun cas de transmission de COVID-19 liée aux CNHD aux travailleurs de la santé n’a été observé.
Conclusion
Notre expérience indique que les CNHD constituent un traitement de première intention efficace pour l’insuffisance respiratoire hypoxémique chez les patients atteints de COVID-19 qui peut être utilisé en toute sécurité, sans risque d’infection significatif discernable pour les travailleurs de la santé.
Similar content being viewed by others
Introduction
Use of high-flow nasal oxygen (HFNO) therapy has increased rapidly in patients with hypoxemic respiratory failure, and is now widely accepted as a standard of care.1,2 With the onset of the COVID-19 pandemic, clinicians were faced with an onslaught of patients with hypoxemic respiratory failure and concerns about viral aerosolization and potential risk to healthcare workers led to uncertainty about the use of HFNO early in the pandemic.3 Such concerns needed to be balanced by the presumed benefits of HFNO, including its simplicity, patient comfort, facilitation of patient communication, and mobilization while using this modality.4,5
Critical care units around the world have since reported variable success with the use of HFNO;6,7 however, most of these reports were published before results of the Recovery trial showed benefit of steroids in patients with moderate-to-severe COVID-19.8 The recent HENIVOT trial, in which all patients received steroids, randomized patients with COVID-19 and moderate-to-severe hypoxemia to either helmet noninvasive ventilation or HFNO.9 While there was no difference in the primary outcome of days free from respiratory support, as a secondary outcome the authors reported a higher incidence of intubation in the HFNO group, raising questions about the role of HFNO in managing patients with COVID-19-associated respiratory failure.
At our centre, there was initial hesitancy regarding HFNO use during the first wave (5 March to 7 June 2020) because of the potential risk to healthcare workers. Nevertheless, as we gained experience with its use, it became the most frequently used form of initial respiratory support for patients admitted to the intensive care unit (ICU) during the second wave of the pandemic. The helmet interface was not available in our institution and we rarely used continuous or bilevel positive pressure ventilation for these patients given persistent concerns about viral transmission and uncertain clinical benefit in hypoxemic respiratory failure.
We describe here our experience and clinical outcomes with the use of HFNO as the initial support device in patients admitted to our ICU with COVID-19-associated hypoxemic respiratory failure, and report our findings regarding HFNO-associated transmission of COVID-19 to healthcare workers.
Methods
Cohort assembly
A prospective database, with a goal to analyse and improve local clinical practice, was established at the start of the current pandemic to allow for collection and analysis of data on all consecutive patients with a confirmed nasopharyngeal polymerase chain reaction (PCR) test result for SARS-CoV-2. Our ICU is at a university-affiliated tertiary care hospital (Jewish General Hospital, McGill University, Montreal, QC, Canada), and operates using a closed, intensivist-led model. We established the current study cohort from this database using all patients with acute hypoxemic respiratory failure admitted between 27 August 2020 and 30 April 2021. This project was approved by the local Research Ethics Committee of the Centre Intégré Universitaire en Santé et Services Sociaux (CIUSSS) West-Central Montreal, Jewish General Hospital.
Patients were included in the cohort upon admission to the ICU from the emergency department or COVID-19 ward after treatment with any oxygen therapy, if HFNO was used as the first means of supplemental oxygen therapy in the ICU, and if HFNO was utilized for at least two hours. Patients were permitted to receive HFNO in the emergency department after being accepted for admission by the ICU physician, while awaiting transfer to the ICU. Patients were excluded if they were endotracheally intubated within two hours of ICU admission. Patients with a directive not to proceed with intubation were excluded from analysis of our primary outcome, but their clinical outcomes are reported separately.
Clinical interventions
High-flow nasal oxygen therapy was administered to all patients via the high-flow treatment mode on the Dräger Evita Infinity V500 ventilator (Dräger Medical, Lübeck, Germany) using the Optiflow plus nasal cannula (Fisher & Paykel Healthcare Ltd., Auckland, New Zealand). The decision to initiate HFNO was made by the treating intensivist when patients were unable to maintain an oxygen saturation of 90% while receiving a fraction of inspired oxygen (FiO2) of 50% or greater via a venturi mask or a filtered nonrebreather mask. Patients receiving HFNO were permitted to receive additional supplemental oxygen over and above that provided by HFNO, with the use of a filtered nonrebreather mask between 10 and 15 L·min-1 to reach the attained target saturation once on full HFNO support (100% FiO2 and 50 L·min-1 flow), and all patients were encouraged to self-prone as tolerated. All patients were treated in single negative pressure rooms with 12 air changes per hour, and all healthcare workers entering the room used full personal protective equipment, including KN95 or fit-tested N95 masks.
All patients in our cohort were treated with systemic dexamethasone. After an initial quality improvement analysis of our database reported previously,10 our local policy for patients receiving an FiO2 of 70% or greater on HFNO suggested high-dose dexamethasone—20 mg daily for five days—followed by 10 mg daily for five days as used in the DEXA-ARDS study,11 and shown to be beneficial in patients with acute respiratory distress syndrome. The ultimate steroid regimen chosen and all other elements of critical care management, were at the discretion of the attending ICU specialist.
The decision to proceed with endotracheal intubation was made by the treating intensivist, with usual indications based on a marked increase in perceived work of breathing that would benefit from positive pressure ventilation, and/or inability to maintain a sustained oxygen saturation by pulse oximetry (SpO2) at rest over 88% despite HFNO at 100% FiO2 and 50 L·min-1 flow plus a filtered nonrebreather mask.
Data extraction
The complete electronic medical record (Chartmaxx® version 7.00, Quest Diagnostics® Incorporated, Secaucus, NJ, USA) for each patient’s admission was reviewed, and relevant data were extracted using a computerized spreadsheet.
Demographic data and patient comorbidities were extracted from the ICU admission note. Patient vital signs, supplemental oxygenation treatments, and laboratory values were extracted from the critical care flowsheet and electronic laboratory system (OACIS, Telus Health, Montreal, QC, Canada). Treatments received and clinical outcomes were confirmed from the medication administration records and clinical progress notes for each patient.
Severity of hypoxemia for each patient on the first day of ICU admission was expressed as the SpO2 to FiO2 ratio using the combination yielding the lowest sustained (for at least five minutes) value at rest on that day (lower values are indicative of worse oxygenation, with values less than 150 being consistent with severe hypoxemia).12,13
A Charlson comorbidity index, which assigns points for various chronic medical conditions, was calculated for each patient.14 We also derived a 4C score for each patient on their first day of hospital admission. This score assigns points based on the patient’s age, sex, number of comorbidities from the Charlson index, obesity (body mass index greater than 30, or clinician-defined), respiratory rate, room air oxygen saturation, Glasgow Coma Scale, serum urea, and C-reactive protein to predict mortality among hospitalized COVID-19 patients.15 The Sequential Organ Failure Assessment (SOFA) score, which predicts ICU mortality based on patient laboratory and clinical data, was calculated for each patient on their first day of ICU admission.16 For patients who did not have an arterial blood gas value, the three lowest SpO2 values in the first 24 hr of ICU admission were averaged and an imputed partial pressure of oxygen (PaO2) using the technique of Brown et al. was generated for use in calculating the SOFA score.12 Acute kidney injury (AKI) was defined as a 50% increase in the patient’s serum urea or creatinine over baseline, or an increase in creatinine by 26.5 µmol·L-1 over baseline.17
Our unit had mandatory reporting by all healthcare workers of any symptoms potentially attributable to COVID-19 as per the list maintained by the infection prevention and control service of our institution. Mandatory nasopharyngeal SARS-CoV-2 PCR testing was required of all symptomatic healthcare workers, and for a period of one month in October 2020 there was weekly asymptomatic screening of most healthcare workers in our unit at the request of the infection control service. All workers with a positive SARS-CoV-2 PCR test result underwent a structured interview with the occupational health and safety service to elucidate the likely source of infection. Workers were investigated by infection control personnel using a standardized interview procedure, and made determinations of healthcare-associated COVID-19 acquisition based on these results in conjunction with an infectious disease physician.
Data on the frequency of symptomatic and asymptomatic healthcare worker screening was obtained from the occupational health and safety service of our institution, for those who arranged testing through this office. Personnel were permitted, for both symptomatic and requested asymptomatic testing, to undergo testing at a government designated screening centre outside our institution. Information on the number of outside screening tests is unavailable for this report, but all positive tests among healthcare workers had mandatory reporting to our occupational health and safety service for epidemiologic investigation.
Outcomes
The primary outcome of interest was the incidence of endotracheal intubation. The secondary outcome was in-hospital mortality, restricted to patients who died or were discharged from hospital alive at the time of data analysis, though we report a lowest to highest range assuming best and worst outcomes for patients remaining in hospital. Additional outcomes included 28-day mortality, the number of days free from an invasive mechanical ventilator in 28 days (ventilator-free days), ICU and hospital length of stay, incidence of barotrauma (pneumothorax and/or pneumomediastinum), the incidence of new AKI, and need for renal replacement therapy.
Mortality was reported separately for patients who had a pre-existing order not to proceed with endotracheal intubation. The incidence of patient care-related COVID-19 acquisition among ICU healthcare workers is reported.
We explored the relationship between predicted and actual mortality as indicated by the 4C score as a prespecified analysis, and conducted a post hoc, exploratory analysis of patient, clinical, and treatment factors associated with our primary outcome of endotracheal intubation.
Statistical analysis
Descriptive statistics were used to summarize baseline demographic and clinical characteristics as well as laboratory results at admission to the hospital, and on the first ICU day. Continuous variables are presented as mean (standard deviation) or median [interquartile range (IQR)] depending on the distribution of the data. Categorical variables are presented as total number and percentage unless stated otherwise.
We conducted comparisons between groups using the Wilcoxon rank sum test for non-normally distributed continuous data and the Chi square test for categorical variables. All analyses were conducted in a two-tailed fashion with statistical significance set at P < 0.05 and were performed using SAS 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
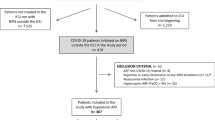
During the study period, 189 patients were admitted to our ICU with COVID-19-associated hypoxemic respiratory failure, of whom 21/189 (11%) had an advanced directive that precluded intubation. Of the remaining 168 patients, 9 (5%) were intubated outside the ICU, 6 (3%) within two hours of admission, 1 was managed with primary noninvasive positive pressure ventilation (NIPPV), and 10 (6%) were treated with low flow oxygen (nasal prongs or venturi mask), leaving N = 142 patients in our cohort (Fig. 1).
Of the 142 patients, 72 (51%) came directly from the Emergency Department and 101 (71%) were male. The median [IQR] age was 66 [59–73] yr, and 44% were classified as obese. Patients had a median [IQR] SpO2/FiO2 ratio of 120 [94–164], and a median [IQR] 4C score of 12 [10–14]. Full demographic, clinical, and treatment information is shown in Table 1.
Endotracheal intubation was performed in 48/142 (34%) patients, with 11 (8%) intubations characterized as emergent for acute hypoxemia, none of which had a peri-intubation complication. Only three patients (2%) received NIPPV; one hypercapnic patient with a neuromuscular disorder, one morbidly obese patient for alveolar recruitment, and one used transiently at the discretion of the treating intensivist.
Intubated patients were older (mean [IQR] age, 70 [61–76] vs 65 [57–71] yr; P = 0.02), had higher SOFA and 4C scores, and had worse oxygenation on the day of ICU admission (median [IQR] SpO2/FiO2 ratio 102 [88–144] vs 126 [108–182]; P < 0.01) compared with those who did not undergo intubation (Table 2).
Hospital mortality information was available for 141/142 (99%) patients and 24 (17%) of these died. Assuming best and worst outcomes for the one remaining patient yields a hospital mortality range of 17–18%. The median [IQR] number of ventilator-free days was 28 [18–28], with median ICU and hospital length of stays of 8 [4–16] and 16 [10–34] days, respectively. Cohort mortality appeared to be well predicted by the 4C score, (Fig. 2) with mortality in our 10–14 subgroup of 17.6% (95% confidence interval [CI], 9.8 to 25.4) and in our > 15 subgroup of 26.7% (95% CI, 10.8 to 42.5) compared with 31% and 62% respectively in the internal validation cohort of the report initially describing the 4C score.15
Barotrauma was noted in 21/142 (15%) patients and new AKI in 46/142 (34%) patients, with 9/142 (7%) requiring acute renal replacement therapy (Table 3).
Patients who were not for intubation (n = 21) were significantly older (median [IQR] age, 85 [76–87] yr; P < 0.01) and had significantly higher median [IQR] 4C scores than the main cohort (16 [13–17] vs 12 [10–14]; P < 0.01). This group also had a significantly higher mortality (67% vs 17%; P < 0.01); nevertheless, the seven patients who survived their ICU stay were discharged alive from hospital.
During the cohort period, there were 27 symptomatic and 139 asymptomatic screening tests conducted in healthcare workers in our unit; however, there were no reported cases of HFNO-associated COVID-19 infection among healthcare workers.
Discussion
The use of HFNO as the initial mode of supplemental oxygen therapy in our ICU for patients with COVID-19-associated hypoxemic respiratory failure was feasible, safe, and associated with intubation and mortality rates similar to other previously published cohorts,6,18 all without the use of noninvasive positive pressure modalities. Since adopting more routine use of HFNO in patients with high FiO2 requirements, we have observed lower intubation rates for similar severity of illness than in the first wave of the pandemic.10
The COVID-19 pandemic has resulted in large numbers of critically ill patients with severe hypoxemic respiratory failure. Use of noninvasive ventilation modalities in hypoxemic respiratory failure has historically been controversial, but reports of reduced intubation rates with HFNO,1,2 and helmet noninvasive ventilation compared with face mask oxygen has led to increasing acceptance of these modalities.19 After hesitancy about HFNO use early in the pandemic related to aerosol generation and infection control issues, there have been many reports of its safe use, especially from early Chinese cohorts.6,7,18 Helmet positive pressure ventilation was the preferred modality of noninvasive oxygenation in Europe, and to date there is only one randomized control trial (RCT) in COVID-19 patients comparing HFNO and helmet positive pressure ventilation.9
Comparing our intubation rate of 34% with other HFNO publications is challenging because of potential differences in patient populations and other ancillary treatments. Early reports of HFNO in COVID-19 cited intubation rates ranging from 40 to 80%.6,7,18 Nevertheless, these publications described patients admitted early in the pandemic to hospitals in China, such that an overwhelmed healthcare system and the lack of routine use of corticosteroids may have affected the overall effectiveness of HFNO. A more recently published Spanish cohort of HFNO treated patients, who were propensity matched on potential confounders with patients undergoing early intubation, reported a comparable incidence of intubation (31%) as our cohort.20 Patients in the HFNO arm of the Spanish cohort were slightly sicker, with a median SOFA of 4 compared with 3 in our cohort, and only 74% of their patients were treated with steroids. Additionally, this Spanish cohort was largely from early on in the pandemic, which may explain why 67% of their patients were intubated early, limiting comparison with our cohort.
In a recent RCT, in which steroid and remdesivir use was nearly universal, patients randomized to HFNO had no difference in the primary outcome of days free from respiratory support, but in a prespecified secondary outcome were found to have a significantly higher intubation rate (51% vs 30%) than patients randomized to helmet noninvasive ventilation.9 Despite patients in our cohort having a higher median SOFA score than those in the HFNO arm of the RCT (3 vs 2), our intubation rate with HFNO was considerably lower and comparable to the noninvasive ventilation arm in their report. The admission characteristics of our cohort were similar to those described in the HFNO arm, although it remains possible that they may have differed with respect to other unmeasured variables. Additionally, we used higher-dose steroids in sicker patients based on our local experience, which may have affected our outcomes.21
The recently developed 4C score is a disease specific prognostic score that can assist clinicians in assessing the prognosis of patients with COVID-19.15 Of interest, mortality across all subgroups of the 4C score was lower in our cohort than in the internal validation cohort from the initial description of this score.15 This finding may reflect selection for admission to our ICU of patients more likely to survive, the fact that our ICU and the Canadian healthcare system in general were never pushed beyond capacity, or possibly an effect of higher-dose corticosteroids.
Barotrauma was seen in 15% of our patients, comparable to the 13% reported in the HFNO arm of the HENIVOT trial.9 Both of these incidences were higher than the noninvasive ventilation arm of the HENIVOT trial, although this difference was not statistically significant in their report.9 If indeed there is a higher incidence of barotrauma in the HFNO group, it may due to self-induced lung injury during laboured spontaneous breathing on HFNO,16 or some other unknown mechanism.
Although limited by a small sample size, we feel that our not-for-intubation cohort provides important information for clinicians about a population rarely described in critical care. While considerably older and sicker than the main cohort, the markedly higher mortality in this group may be helpful information for clinicians, patients, and their families in this pandemic.
Despite initial, and in some cases ongoing, concern about the association of HFNO and nosocomial transmission of COVID-19, we documented no such transmission among any healthcare workers caring for patients in our cohort, in an environment with a robust infection control and screening programme. While this may reflect a true low risk of bioaerosol generation with HFNO,22 we wish to highlight the importance of strict adherence to personal protective equipment, including obligate use of a KN95 or fit-tested N95 masks when entering the room, and our use of Canadian Standards Association compliant single patient negative pressure rooms with 12 air changes per hour. This finding should reassure other centres, with similar approaches to infection control, of the safety of this modality in COVID-19, and other respiratory viral infections.
Our study is limited by single-centre conduct, its retrospective design, and lack of a comparator group, which prohibits establishing causal links between particular exposures and outcomes of interest. Additionally, as with any retrospective study, there is the risk of misclassification for certain variables in the primary record, or missing data. These limitations were mitigated by having the data abstracted by trained researchers and possible discrepancies discussed among the authors. Missing data, such as the unavailability of PaO2 values for certain patients, was handled by imputation using a recognized and accepted method. Finally, we did not have access to the numbers of all screening tests done outside of our institution. Accordingly, we suspect a higher incidence of screening among our healthcare workers than we report here, as many workers chose to be tested at centres closer to their homes when they were symptomatic or when asked to participate in asymptomatic screening. We are very confident, however, that with healthcare worker and public health reporting, that we are not missing any positive COVID-19 cases among our personnel. Strengths of our study include the comprehensive inclusion of all consecutively treated HFNO patients, currently one of the largest cohorts of primary HFNO patients reported, making our findings generalizable to similar centres around the world.
In conclusion, we found that use of HFNO therapy as the primary means of oxygenation for COVID-19-associated respiratory failure was safe and associated with an acceptable incidence of endotracheal intubation and mortality, without the use of other noninvasive respiratory support modalities. Additionally, we report no healthcare worker acquisition of COVID-19 associated with caring for patients using HFNO therapy, further reinforcing the safety of using this modality for patients in the pandemic.
References
Frat JP, Thille AW, Mercat A, et al. High-flow oxygen through nasal cannula in acute hypoxemic respiratory failure. N Engl J Med 2015; 372: 2185-96.
Ferreyro BL, Angriman F, Munshi L, et al. Association of noninvasive oxygenation strategies with all-cause mortality in adults with acute hypoxemic respiratory failure: a systematic review and meta-analysis. JAMA 2020; 324: 57-67.
Agarwal A, Basmaji J, Muttalib F, et al. High-flow nasal cannula for acute hypoxemic respiratory failure in patients with COVID-19: systematic reviews of effectiveness and its risks of aerosolization, dispersion, and infection transmission. Can J Anesth 2020; 67: 1217-48.
Suffredini DA, Allison MG. A rationale for use of high flow nasal cannula for select patients with suspected or confirmed severe acute respiratory syndrome coronavirus-2 infection. J Intensive Care Med 2021; 36: 9-17.
Rochwerg B, Einav S, Chaudhuri D, et al. The role for high flow nasal cannula as a respiratory support strategy in adults: a clinical practice guideline. Intensive Care Med 2020; 46: 2226-37.
Hu M, Zhou Q, Zheng R, et al. Application of high-flow nasal cannula in hypoxemic patients with COVID-19: a retrospective cohort study. BMC Pulm Med 2020; DOI: https://doi.org/10.1186/s12890-020-01354-w.
Xu J, Yang X, Huang C, et al. A novel risk-stratification models of the high-flow nasal cannula therapy in COVID-19 patients with hypoxemic respiratory failure. Front Med (Lausanne) 2020; DOI: https://doi.org/10.3389/fmed.2020.607821.
RECOVERY Collaborative Group; Horby P, Lim WS, et al. Dexamethasone in hospitalized patients with Covid-19. N Engl J Med 2021; 384: 693-704.
Grieco DL, Menga LS, Cesarano M, et al. Effect of helmet noninvasive ventilation vs high-flow nasal oxygen on days free of respiratory support in patients with COVID-19 and moderate to severe hypoxemic respiratory failure: the HENIVOT randomized clinical trial. JAMA 2021; 325: 1731-43.
Yang SS, Lipes J, Dial S, et al. Outcomes and clinical practice in patients with COVID-19 admitted to the intensive care unit in Montreal, Canada: a descriptive analysis. CMAJ Open 2020; 8: E788-95.
Villar J, Ferrando C, Martinez D, et al. Dexamethasone treatment for the acute respiratory distress syndrome: a multicentre, randomised controlled trial. Lancet Respir Med 2020; 8: 267-76.
Brown SM, Grissom CK, Moss M, et al. Nonlinear imputation of Pao2/Fio2 from Spo2/Fio2 among patients with acute respiratory distress syndrome. Chest 2016; 150: 307-13.
Chen W, Janz DR, Shaver CM, Bernard GR, Bastarache JA, Ware LB. Clinical characteristics and outcomes are similar in ARDS diagnosed by oxygen saturation/Fio2 ratio compared with Pao2/Fio2 ratio. Chest 2015; 148: 1477-83.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987; 40: 373-83.
Knight SR, Ho A, Pius R, et al. Risk stratification of patients admitted to hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: development and validation of the 4C Mortality Score. BMJ 2020; DOI: https://doi.org/10.1136/bmj.m3339.
Brochard L, Slutsky A, Pesenti A. Mechanical ventilation to minimize progression of lung injury in acute respiratory failure. Am J Respir Crit Care Med 2017; 195: 438-42.
Kellum JA, Lameire N, KDIGO Guideline Work Group. Diagnosis, evaluation, and management of acute kidney injury: a KDIGO summary (part 1). Crit Care 2013; DOI: https://doi.org/10.1186/cc11454.
Wang K, Zhao W, Li J, Shu W, Duan J. The experience of high-flow nasal cannula in hospitalized patients with 2019 novel coronavirus-infected pneumonia in two hospitals of Chongqing, China. Ann Intensive Care 2020; DOI: https://doi.org/10.1186/s13613-020-00653-z.
Patel BK, Wolfe KS, Pohlman AS, Hall JB, Kress JP. Effect of noninvasive ventilation delivered by helmet vs face mask on the rate of endotracheal intubation in patients with acute respiratory distress syndrome: a randomized clinical trial. JAMA 2016; 315: 2435-41.
Mellado-Artigas R, Ferreyro BL, Angriman F, et al. High-flow nasal oxygen in patients with COVID-19-associated acute respiratory failure. Crit Care 2021; DOI: https://doi.org/10.1186/s13054-021-03469-w.
Yang SS, Lipes J. Corticosteroids for critically ill COVID-19 patients with cytokine release syndrome: a limited case series. Can J Anesth 2020; 67: 1462-4.
Li J, Fink JB, Ehrmann S. High-flow nasal cannula for COVID-19 patients: low risk of bio-aerosol dispersion. Eur Respir J 2020; DOI: https://doi.org/10.1183/13993003.00892-2020.
Author contributions
Blair Carl Schwartz, Dev Jayaraman, and Sandra Dial contributed to all aspects of this manuscript, including study conception and design; acquisition, analysis, and interpretation of data; and drafting and revising the article. Jed Lipes and Stephen Su Yang contributed to acquisition and interpretation of the data. Jed Lipes, Stephen Su Yang, and Evan G. Wong contributed to the conception and design of the study and revising the article.
Acknowledgements
The authors would like to thank Mrs Tharaniya Vallipuram and Dr. Leighanne Parkes for their contributions to this manuscript, and to all healthcare workers in our intensive care unit for their tireless, professional, and compassionate care of our patients during this pandemic
Disclosures
None.
Funding statement
None.
Editorial responsibility
This submission was handled by Dr. Sangeeta Mehta, Associate Editor, Canadian Journal of Anesthesia/Journal canadien d’anesthésie.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Schwartz, B.C., Jayaraman, D., Yang, S.S. et al. High-flow nasal oxygen as first-line therapy for COVID-19-associated hypoxemic respiratory failure: a single-centre historical cohort study. Can J Anesth/J Can Anesth 69, 582–590 (2022). https://doi.org/10.1007/s12630-022-02218-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-022-02218-z