Abstract
Purpose
Anesthesia is associated with alterations in end-tidal (ET) respiratory gases from the awake state. These alterations result in marked vasoactive changes in regional cerebral blood flow (rCBF). Altered regional cerebrovascular reactivity (rCVR) is linked to neurologic dysfunction. We examined these differences in reactivity from prior work by focusing on the ratio of vasoconstriction with hyperoxia/hypocapnia (HO/hc):vasodilation with hypercapnia (HC) using magnetic resonance imaging pseudo-continuous arterial spin labelling (pCASL) to measure rCBF and compare rCVR The distribution and magnitude of these ratios could provide insights into rCBF during clinical anesthesia and inform future research into the origins of postoperative delirium (POD).
Methods
Ten healthy subjects underwent cerebral blood flow (CBF) studies using pCASL with computer-controlled delivery of ET gases to assess flow effects of hyperoxia, hypercapnia, and hyperoxia/hypocapnia as part of a larger study into cerebrovascular reactivity. The vasoconstrictor stimulus was compared with the vasodilator stimulus by the ratio HO/hc:HC.
Results
Hyperoxia minimally decreased whole brain CBF by − 0.6%/100 mm Hg increase in ETO2. Hypercapnia increased CBF by +4.6%/mm Hg carbon dioxide (CO2) and with HO/hc CBF decreased by − 5.1%/mm Hg CO2. The brain exhibited markedly different rCVR—regional HO/hc:HC ratios varied from 7.2:1 (greater response to vasoconstriction) to 0.49:1 (greater response to vasodilation). Many of the ratios greater than 1, where vasoconstriction predominated, were seen in regions associated with memory, cognition, and executive function, including the entorhinal cortex, hippocampus, parahippocampus, and dorsolateral prefrontal cortex.
Conclusions
In awake humans, marked rCBF changes occurred with alterations in ET respiratory gases common under anesthesia. Such heterogeneous reactivity may be relevant to future studies to identify those at risk of POD.
Résumé
Objectif
L’anesthésie est associée à des altérations des gaz respiratoires télé-expiratoires par rapport à l’état d’éveil. Ces altérations entraînent des changements vasoactifs marqués dans le débit sanguin cérébral régional (DSCR). Une altération de la réactivité cérébrovasculaire régionale (rCVR) est liée au dysfonctionnement neurologique. Nous avons examiné ces différences de réactivité dans des études antérieures en nous concentrant sur le rapport entre la vasoconstriction et l’hyperoxie/hypocapnie (HO/hc):vasodilatation et l’hypercapnie (HC), en utilisant une technique d’imagerie par résonance magnétique dite pCASL (pour pseudo-continuous arterial spin labelling) pour mesurer le DSCR et comparer la rCVR. La distribution et l’ampleur de ces rapports pourraient fournir des renseignements concernant le DSCR pendant l’anesthésie clinique et éclairer la recherche future sur les origines du delirium postopératoire (DPO).
Méthode
Dix volontaires sains ont subi des études de débit sanguin cérébral (DSC) à l’aide d’une pCASL avec un contrôle géré par ordinateur des gaz télé-expiratoires pour évaluer les effets sur le débit de l’hyperoxie, de l’hypercapnie, et de l’hyperoxie/hypocapnie dans le cadre d’une plus grande étude sur la réactivité cérébrovasculaire. Le stimulus vasoconstricteur a été comparé au stimulus vasodilatateur par le rapport de HO/hc:HC.
Résultats
L’hyperoxie a diminué de façon minimale le DSC du cerveau entier de − 0,6 %/100 mmHg en ETO2. L’hypercapnie a augmenté le DSC de +4,6 %/mmHg de dioxyde de carbone (CO2) et avec le HO/hc, le DSC a diminué de − 5,1 %/mmHg CO2. Le cerveau a exhibé une rCVR nettement différente –-les rapports régionaux HO/hc:HC allaient de 7.2:1 (plus grande réponse à la vasoconstriction) à 0.49:1 (plus grande réponse à la vasodilatation). Beaucoup des rapports supérieurs à 1, où la vasoconstriction était prédominante, ont été observés dans les régions associées à la mémoire, à la cognition et à la fonction exécutive, y compris le cortex entorhinal, l’hippocampe, le parahippocampe et le cortex préfrontal dorsolatéral.
Conclusion
Chez une personne éveillée, des changements marqués de DSCR se sont produits lors des changements dans les gaz respiratoires télé-expiratoires survenant communément sous anesthésie. Une telle réactivité hétérogène pourrait être pertinente pour les études futures afin d’identifier les personnes à risque de DPO.
Similar content being viewed by others
Under anesthesia, the basal homeostatic end-tidal (ET) gas tensions for carbon dioxide (CO2) and oxygen (O2) can be markedly altered. End-tidal carbon dioxide (ETCO2) may be both lower (with mechanical ventilation) and higher (during emergence) compared to normal awake conditions, and end-tidal oxygen (ETO2) is usually much higher than when awake due to elevated fractions of inspired oxygen. Both of these ET gases are vasoactive and can alter cerebral blood flow (CBF) globally and result in considerable regional flow heterogeneity. Such alterations in cerebrovascular reactivity (CVR) may have consequences in patients with vulnerable brains-at-risk. Increased understanding of the human regional cerebral blood flow (rCBF) response to alterations in ETCO2 and O2 has occurred over the past decade using advanced magnetic resonance imaging approaches coupled with rigorous control of respiratory gases.1,2,3,4 Especially with CO2, significant regional heterogeneity in CVR and its dynamic responsiveness has been consistently shown in healthy individuals and more marked changes have been seen in aging individuals and individuals with various neurologic diseases including cerebrovascular deficiency, dementia, concussion, multiple sclerosis, sleep apnea, white matter abnormalities, and sickle cell anemia.5,6,7,8,9,10,11,12 Small changes in ETCO2 (5–10 mm Hg) can manifest with marked alterations in CBF in patients at risk of neurologic dysfunction with flow changes resulting in intracranial steal, inverse steal, and oscillations between the two conditions as the ETCO2 fluctuates resulting in dynamic flow dyssynchrony.1,3,13 These flow alterations can occur rapidly, often onsetting within seconds of change in the vasoactive stimulus. These heterogeneous responses have been exploited to aid in diagnosis and to assess therapeutic interventions in various neurologic conditions.5,14 In addition, heterogeneous rCBF becomes even more varied depending on the initial set point prior to further altering CO2.15 On exposure to initial hypercapnia, hypocapnia-induced relative changes in regional cerebrovascular reactivity (rCVR) can differ significantly from the responses seen with normocapnic baseline conditions.
Less well studied are the rCBF responses to hyperoxia16,17,18 and even less well evaluated are the combined effects of hyperoxia and hypocapnia on rCBF.19 The latter combination of ET respiratory gases is common during anesthesia.20,21,22 Situations similar to these experimental conditions, where ETCO2 varies from hypercapnic to hypocapnic tensions and ETO2 is hyperoxic before restoration to an individual’s normocapnic/normoxic baseline, can occur multiple times during the conduct of an anesthetic, suggesting large and potentially deleterious oscillations in rCBF may emerge even during a routine surgical procedure. It remains unclear if such alterations could potentially compromise CBF homeostasis for patients at risk of neurologic complications including postoperative delirium (POD) during anesthesia, where ETCO2 and ETO2 fluctuations exist for hours during a surgical procedure.23
To establish whether fluctuations in ET gases could result in rCBF dyssynchony, we investigated the regional heterogeneity of the CBF response in awake subjects to ET gas alterations commonly seen during anesthesia in a post hoc analysis of our prior work examining these issues.19 Newly examined here is the differential response to vasoconstriction, measured by the rCBF with hyperoxia/hypocapnia (HO/hc) to the response to vasodilation (HC) and the global and regional ratios of vasoconstriction:vasodilation.
Methods
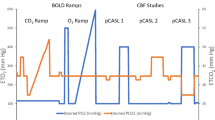
This study was approved by the local institutional review board—the Biomedical Research Ethics Board of the University of Manitoba. Written informed consent was obtained from all participants. Parts of this study were conducted under ClincialTrials.gov NCT02126215, first registered on 29 April 2014 under the first author’s name. This cohort was studied from 1 March 2019 to 7 June 2019. This cross-sectional study is based on prior work measuring rCBF with the MRI pseudo-continuous arterial spin labelling (pCASL) technique.19 New here is the approach to post-hoc analysis comparing the ratio of regional vasoconstrictive to vasodilatory responsiveness with ET gas alterations commonly seen under anesthesia. Participants were healthy volunteers with no known neurologic diagnoses (except migraine headache in one participant). None were receiving psychotropic drugs for a psychiatric condition. Post hoc analysis of prior results of awake human MRI studies of CBF response to computer-controlled alterations in ETO2 and ETCO2 was undertaken.19 These studies had baseline and altered CBF determined by pCASL using a RespirAct™ (Thornhill Research Inc., Toronto, ON, Canada)—a model-based prospective ET gas targeting (MPET) device (U.S. Food and Drug Administration approval pending) to tightly control the ETCO2 and O2 to desired levels.19 This device enables very tight control of ET gases utilizing a closed breathing system with computer-controlled sequencing of ET gases to provide highly reproducible vasoactive stimuli to study CBF dynamics. In the context used in this experimentation, ETO2 could be kept stable or “clamped” while ETCO2 was varied over the range programmed and vice versa. The generation of whole brain CBF and rCBF difference maps based on these rigorously controlled ET conditions for O2 and CO2 as commonly seen during anesthesia was investigated (see eFig. 1 in the Electronic Supplementary Material [ESM] for the protocol). We examined the magnitude and regional distribution of baseline-hyperoxia (BL-HO) CBF differences, hypercapnia-baseline (HC-BL) CBF differences and rCVR (ΔCBF/ΔCO2) and baseline-hyperoxia/hypocapnia (BL-HO/hc) CBF differences and rCVR (ΔCBF/ΔCO2) conditions. Once determined, the regional ratios of the response to the two vasoactive conditions was examined (i.e., regional comparison of HO/hc:HC).
For this study, whole brain CBF was determined using the ASL toolbox (https://cfn.upenn.edu/~zewang/ASLtbx.php)24 following image processing in SPM8 (Statistical Parametric Mapping, version 8) (https://www.fil.ion.ucl.ac.uk/spm/software/download/). Whole brain and regional masks to examine brain-at-risk were constructed using the Wake Forest University Pick Atlas (https://www.nitrc.org/frs/?group_id=46). Regional masks were constructed to examine CBF in multiple regions of interest (n = 19) including entorhinal, hippocampal, inferior temporal, middle temporal, parahippocampal, and Brodmann areas 10 and 11 regions—regions associated with memory, executive function, and cognitive function. These whole brain CBFs and rCBFs were calculated using the post-analysis toolbox, MarsBaR (MARSeille Boîte À Région d’Intérêt) (http://marsbar.sourceforge.net/download.html) and alterations in CBF for various changes in ET respiratory gas values were compared with baseline conditions.
Previously developed mathematical modelling (LabView, National Instruments, TX, USA) was altered to coincide with the baseline whole brain CBF conditions obtained from the imaging described above. The delivery of O2 (DO2) tissue partial pressure of oxygen (PtO2), and oxygen extraction fraction (OEF) was modelled on the baseline whole brain CBF findings (ESM Supplementary Model and eFig 2 and 3). This modelling was adapted from the previously developed mathematical model describing hypocapnia and anemia,25 and the brain response to hypercapnia and hypoxia.26 Whole brain-at-risk for hyperoxia/normocapnia, hyperoxia/hypocapnia, the effect of anemia on CaO2 and CBF, and the influence of anesthesia (both volatile and intravenous agents—increased CBF and decreased CMRO2 for the former and decreased CBF and decreased CMRO2 for the latter) were examined and shown in ESM eTable.
Statistical analysis
Mean values for the CBF conditions were determined based on second level analysis for HC-BL and BL-HO/hc using the SPM8 platform (https://www.fil.ion.ucl.ac.uk/spm/doc/spm8_manual.pdf). Regional reactivity to these conditions was examined by comparison with the null hypothesis (no difference from the canonical response that the general linear model regressed to the delivered ET gas challenge). The data are at the P = 0.005 level for the images displayed.
Results
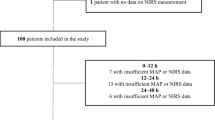
Controlled breathing studies using MPET resulted in the changes in ET gases and CBF shown in the Table 1. There were ten participants—four males and six females with a mean (standard deviation [SD]) age of 49 (12) yr. All ten participants completed the hyperoxia/normocapnia (HO) portion of the study, nine completed the second component of normoxia/hypercapnia (HC) and six completed the final component of hyperoxia/hypocapnia (HO/hc)—five of these had stable hypocapnia for the three-minute imaging period examined. One result was discarded in this ET gas sequence because of artefactual flow results due to a processing failure. In this participant, a ring of abnormal flow was evident as a hyperperfusion halo around the brain periphery that could not be removed with various processing corrections. The raw whole brain baseline mean CBF at normocapnic/normoxic baseline was 38.1 (7.7) mL·100 g−1·min−1 (Fig. 1A). The mean difference maps for HO-BL and HO/hc-BL are shown in Fig. 1B and C, respectively. The whole brain flow difference for HO-BL was − 0.7 (4.4) mL·100 g−1·min−1. Thus, whole brain showed a modest decrease in CBF to hyperoxia. The ETCO2 was very tightly controlled during the hyperoxia studies [mean (SD) decrease, 0.4 (0.7) mm Hg from baseline]. When the decrease in CBF with hyperoxia reported by Watson et al. is corrected for their reported decrease in CO2 during these measurements, we found a decrease in whole brain CBF of 1.8% per 100 mm Hg increase in O2 tension. For the combined vasoconstrictive stimulus, HO/hc-BL, the whole brain flow difference was − 7.6 (7.4) mL·100 g−1·min−1.
(A-C) Mean regional cerebral blood flow (rCBF) images from ten healthy, awake participants showing cerebral blood flow (CBF) at baseline: (A) normocapnia/normoxia; (B) mean CBF difference maps (n = 10) after breathing oxygen (O2) to increase end-tidal O2 (ETO2) to 400 mm Hg. A heterogeneous rCBF is evident; (C) the mean difference map (n = 5) shown following hyperoxia/hypocapnia (breathing O2 to increase ETO2 to 400 mm Hg and the participant voluntarily hyperventilating to decrease end-tidal carbon dioxide by 5 mm Hg below baseline values) indicating marked regional decrease in CBF throughout the entire brain. These CBF images were obtained using a pseudo-continuous arterial spin labelling (pCASL) MRI approach with ET respiratory gases tightly controlled by employing a RespirAct.(4) The colour bar legend is CBF in mL·100 g−1·min−1. The number to the left and below each image is the distance above or below the anterior commissure–posterior commissure (AC-PC) line
Regional differences in HO (n = 10) are shown in Fig. 2 (in orange) with the baseline conditions shown as 100% response (in blue). The horizontal bars show mean values and horizontal lines are SDs. The maximal decrement in rCBF was seen in the thalamus at 95.2% of baseline flow and the maximal increase in rCBF was seen in the insula at 102.9% of baseline. Thus, the regional differences to hyperoxia were very limited. Such was not the case when hypocapnia occurred in concert with HO. The change in rCBF for HO/hc is also shown in Fig. 2 (n = 5; in grey). With this ET alteration superimposed, there were marked rCBF decreases in whole brain and in all regions examined. The smallest decrement was in the insula at 93.5% of baseline and the greatest decrement was in the inferior temporal region at 69.1% of baseline. When rCVR was normalized (100% - ΔrCBF%/ΔCO2), the minimal CVR decrement was 1.6% flow decrement/mm Hg decrease in CO2 for the insula to 7.5% flow decrement/mm Hg decrease in CO2 in the inferior temporal region.
Whole brain and regional cerebral blood flow (rCBF) response at baseline – normoxia/normocapnia (shown as 100%) in blue (n = 10). In orange is the change in rCBF to hyperoxia (HO) at stable normocapnia as a percentage of baseline (n = 10). In grey is the change in rCBF to hyperoxia/hypocapnia (HO/hc); (n = 5). Error bars represent standard deviations for each mean value
For HC-BL (not shown in Fig. 1), the mean whole brain flow difference was an increase of 7.5 (8.3) mL·100 g−1·min−1. Thus, the CVR for HC in whole brain was an increase of 4.8 (2.4) % per mm Hg increase in CO2. Flow increased in all regions. The regional differences to HC (n = 9) are shown in Fig. 3 (in orange) with the baseline conditions shown as 100% response (in blue). The minimal increase in rCBF was seen in the hippocampus at 101.9% of baseline flow and the precuneus showed the maximal increase in rCBF at 127.0% of baseline. When rCVR was normalized for HC (rCBF%/ΔCO2 - 100%) the minimal CVR increase was 0.7% flow increase/mm Hg increase in CO2 for the hippocampus compared with a 6.8% flow increase/mm Hg increase in CO2 in the occipital region. Also shown (as in Fig. 2) is the change in rCBF for HO/hc (n = 5; in grey).
Whole brain and cerebral blood flow (rCBF) response at baseline – normoxia/normocapnia (shown as 100%) in blue (n = 9). In orange is the change in rCBF to hypercapnia (HC) at stable normoxia as a percentage of baseline (n = 9). In grey is the change in rCBF to hyperoxia/hypocapnia (HO/hc; n = 5). Error bars represent standard deviations for each mean value
The statistically significant distribution of increased mean regional flow for HC-BL is shown in Fig. 4A (P = 0.005 to manifest as colourized pixels compared with the null hypothesis). The distribution of altered mean flow for BL-HO/hc is shown in Fig. 4B (P = 0.005 to manifest as colourized pixels compared with the null hypothesis).
The ratios of responses to vasoconstriction:vasodilation measured as HO/hc:HC are shown in Fig. 5. A ratio greater than 1 indicated greater CBF reactivity to vasoconstriction than vasodilation with the same ΔCO2 stimulus (4.1 [1.6] mm Hg increase in CO2 for vasodilation and 4.0 [0.6] mm Hg decrease in CO2 for vasoconstriction). Many of the brain regions with a greater sensitivity to the vasoconstrictive stimulus are associated with executive function, memory, and cognition and were previously identified as Alzheimer’s disease risk regions.27 Other areas with ratios less than 1 have been identified with various regional networks such as the default mode network and salience and executive function networks. The whole brain response was essentially balanced at 1:1 for the vasoconstrictive to vasodilatory stimulus with equal CVR magnitude to the vasoconstrictive stimulus HO/hc and the vasodilator stimulus HC.
Mathematical modelling for whole brain based on the CBF results obtained in this study were used to calculate DO2, OEF, and PtO2 for various conditions as shown in eTable (ESM). This modelling shows that the normal healthy brain is very adaptive with minimal changes in PtO2 for the conditions shown in the awake state and under anesthesia. This is in keeping with similar CVR for whole brain to HC and HO/hc as described above. The important finding in this study is that the whole brain response as depicted in the model and confirmed globally in our investigation does not reflect the wide heterogeneity of the regional response.
Discussion
In this post hoc analysis of our prior work19 to determine differential regional brain cerebrovascular responsiveness using MRI CBF (pCASL) methodology, we have shown marked regional differences in the human brain’s CVR to carefully controlled vasodilatory or vasoconstrictive stimuli by altering ET gases. We examined the regional brain responsiveness to HO, HC, and HO/hc in awake humans. The responsiveness ratios to HO/hc:HC varied over a 15-fold magnitude for the relative CVR to either a vasoconstrictor stimulus of hypocapnia with hyperoxia or a vasodilator stimulus of hypercapnia. These are novel observations based on this analysis approach. Although our study had limited statistical power to separate sex- or age-related regional differences, the range of ET gases studied replicate the ET gases commonly seen during routine anesthesia. We identified regional differences (ratios greater than 1) in areas associated with cognition, executive function, or memory (Fig. 5), including the prefrontal cortex, entorhinal cortex, hippocampus, parahippocampus, inferior temporal cortex, and Brodmann areas 10 and 11.27 In the awake state, the vasoconstrictive stimulus of decreased CO2 combined with high inspired O2 tension showed that these regions are markedly responsive to a reduction in flow compared with the greater flow with increased CO2. Such sensitivity was evident over a modest (4 mm Hg) decrease in CO2 tension. Other regions with a variety of homeostatic functions, such as the insula, responded in the opposite fashion and showed minimal CBF decrease with hypocapnia compared with a vigorous increase in CBF with hypercapnia. Together, these findings suggest that alterations in CO2 and O2 may adversely affect the basal rCBF balance under these “stress” conditions. Prolonged periods of alterations in respiratory gases represented in our study can occur even during routine anesthesia procedures and rCBF heterogeneity to step changes in CO2 has been shown under anesthesia in humans, including both volatile and intravenous agents.28,29 Thus, the dynamic reactivity to changes in ET respiratory gases seen while awake could be reasonably expected to occur during general anesthesia.
Similar to our findings, recent work using the same methodology to rigorously control ET gases as described here has shown rCBF and CVR heterogeneity to changes in CO2.15 Importantly, this publication also showed that the heterogeneity is further altered contingent on the ETCO2 baseline conditions prior to initiating the experimental changes to CO2 tension, where the rCVR to vasoconstriction and vasodilation varied over three-fold to controlled alterations in ETCO2. This work also indicated that the delay in response to the vasoactive stimulus (varying ET tensions of CO2) are dependent on the baseline CO2 tension, showing a response delay to increased CO2 of five to ten seconds with basal hypocapnia compared with 15–20 sec with basal hypercapnia. These variable responses to alterations in CO2 create conditions for intracranial steal and inverse steal regionally, potentially increasing the risk of ischemic flow in susceptible patients.1,3,5 Our CVR results for hypercapnia are similar to those of Halani et al.15 but we found a greater responsiveness to combined hyperoxia/hypocapnia than hypocapnia alone in their study, suggesting an additive or synergistic effect of hyperoxia on hypocapnia-induced vasoconstriction. We did not measure the effect of hypocapnia alone because of the total experimental time required and practical limitations of repeated vigorous hyperventilation, although these data would have allowed us to more precisely determine whether hyperoxia is additive to hypocapnia. Using blood oxygen level-dependent imaging alone, Lui et al.30 have reported similar CVR heterogeneity, and other recent work has shown specific anatomical MRI phenotypes associated with POD.31
In the study by Watson et al., a decrement in CBF of ~4.5% per 100 mm Hg increase in O2 tension was measured. Examining the pure effect of hyperoxia on CBF is problematic as in a freely breathing individual, hyperoxia results in the Haldane effect and increased minute ventilation compared with normoxia, thereby confounding the interpretation of the “pure” hyperoxic effects on CBF.32,33 In this study, we tightly controlled ETCO2 (only a mean 0.4 mm Hg [n = 10] decrease from baseline in CO2 for the hyperoxic measurement period) and were able to show a “pure” effect of hyperoxia on CBF. After correcting for the mean 2.25 mm Hg decrease in CO2 reported by Watson et al., we calculate a CBF change of − 1.8% per 100 mm Hg of O2 tension, much closer to our measurement of − 0.6% per 100 mm Hg O2 tension. Regardless, the flow decrement with hyperoxia is modest compared with that seen for changes in CO2 at normocapnic baseline.
Hypocapnia has been implicated with POD in some studies,22,34 although these results did not provide a mechanistic explanation for the increase in POD with hypocapnia. The current work provides additional insights into why POD occurs more frequently in this context. Additionally, patients undergoing endovascular thrombectomy for stroke with general anesthesia have poorer outcomes if hypocapnic intraoperatively.35 We found marked regional disparity to the HO/hc:HC ratio. If these observations are applied clinically, regions with ratios greater than 1 are preferentially susceptible to the combined vasoconstrictor effects of HO/hc with decreased rCBF. Recent work has indicated that delirium is prolonged with an inverse flow-time responsiveness between precuneus and posterior cingulate and altered responsiveness between the thalamus and caudate nucleus. These imbalances resolve as the episode of delirium eases.36 Consistent with these observations, our flow studies show markedly heterogeneous CVR between these regions in the face of changes in ETCO2 and O2. Our previous modelling has shown that under normal conditions, the whole brain is remarkably tolerant to the perturbations in ET gases; however, the additional data presented here suggest that large differences can occur on a regional level (see data and references presented in the ESM).
This study has a number of limitations, including a small number of participants to examine awake human rCBF changes caused by rigorous manipulation of ET gases. As such, it is a surrogate for the clinical alterations in ET gases that can occur under anesthesia, and there were no neurologic complications observed in any participants in this study. Any one experimental alteration in ET gases from baseline was limited to a short three-minute increment, with prompt restoration to baseline conditions, which may not be representative of much greater periods of time under anesthesia. In addition, the changes in ETCO2 were modest (total mean ΔCO2 of 8.1 mm Hg), in part for participant comfort, resulting in rCBF changes that may be less pronounced than those under anesthesia. The HO/hc:HC ratios presented are based on a small sample size. It is likely that these ratios may differ in a larger cohort, especially as the coefficient of variation of the CVR was high in some of the regions examined. Patients at risk of POD due to cerebrovascular dysfunction may be more vulnerable to alternations in regional CBF if intracranial steal results from changes in CO2 tension, a context not captured in our healthy participants. The broad range seen for the ratios presented suggest real differences to CO2 reactivity regionally and is supported by prior studies,15 although the addition of anesthetic agents could influence the ratio balance. Verification of these findings while under anesthesia is logistically difficult but possible at a few specialized centres. Importantly, basal CBFs have been shown under anesthesia with the same approach to control ET gases as used here.28,29
Conclusions
True diagnostic assessment of the risk of altered ET respiratory gases under anesthesia requires establishing an atlas of patients imaged before surgery to determine CBF signatures correlated to POD. Such an approach has been successfully accomplished to determine CBF biomarkers in other conditions.6,37 A preliminary study has been undertaken and has indicated that the imaging approach has merit.23 We have shown the feasibility of a vasoactive reactivity test showing regional CVR heterogeneity in awake, healthy adults. These findings raise questions about the role of ET gas management in clinical practice that should be addressed in future studies. Outcome correlations based on altered regional CVR vasoconstriction:vasodilation ratios may offer new insights into mechanisms of POD and potentially permit preoperative risk assessment.
References
Sobczyk O, Crawley AP, Poublanc J, et al. Identifying significant changes in cerebrovascular reactivity to carbon dioxide. Am J Neuroradiol 2016; 37: 818-24.
Fierstra J, Sobczyk O, Battisti-Charbonney A, et al. Measuring cerebrovascular reactivity: what stimulus to use? J Physiol 2013; 591: 5809-21.
Duffin J, Sobczyk O, McKetton L, et al. Cerebrovascular resistance: the basis of cerebrovascular reactivity. Front Neurosci 2018; 1: 409.
Slessarev M, Han J, Mardimae A, et al. Prospective targeting and control of end-tidal CO2 and O2 concentrations. J Physiol 2007; 581(Pt 3): 1207-19.
Sam K, Poublanc J, Sobczyk O, et al. Assessing the effect of unilateral cerebral revascularisation on the vascular reactivity of the non-intervened hemisphere: a retrospective observational study. BMJ Open 2015; 5:
Shafi R, Poublanc J, Venkatraghavan L, et al. A Promising subject-level classification model for acute concussion based on cerebrovascular reactivity metrics. J Neurotrauma 2021; 38: 1036-47.
McKetton L, Sobczyk O, Duffin J, et al. The aging brain and cerebrovascular reactivity. Neuroimage 2018; 181: 132-41.
Fisher JA, Iscoe S, Duffin J. Sequential gas delivery provides precise control of alveolar gas exchange. Respir Physiol Neurobiol 2016; 225: 60-9.
Sam K, Peltenburg B, Conklin J, et al. Cerebrovascular reactivity and white matter integrity. Neurology 2016; 87: 2333-9.
Leung J, Duffin J, Fisher JA, Kassner A. MRI-based cerebrovascular reactivity using transfer function analysis reveals temporal group differences between patients with sickle cell disease and healthy controls. NeuroImage Clin 2016; 12: 624-30.
Li N, Liu Y, Zhao Y, Wu X, Tong J, Hua Y. Cerebrovascular reactivity in young and old patients with obstructive sleep apnea. Sleep Med 2020; 73: 125-9.
Lattanzi S, Acciarri MC, Danni M, et al. Cerebral hemodynamics in patients with multiple sclerosis. Mult Scler Relat Disord 2020; 44:
Sobczyk O, Battisti-Charbonney A, Fierstra J, et al. A conceptual model for CO2-induced redistribution of cerebral blood flow with experimental confirmation using BOLD MRI. Neuroimage 2014; 92: 56-68.
Fierstra J, Poublanc J, Han JS, et al. Steal physiology is spatially associated with cortical thinning. J Neurol Neurosurg Psychiatry 2010; 81: 290-3.
Halani S, Kwinta JB, Golestani AM, Khatamian YB, Chen JJ. Comparing cerebrovascular reactivity measured using BOLD and cerebral blood flow MRI: the effect of basal vascular tension on vasodilatory and vasoconstrictive reactivity. Neuroimage 2015; 110: 110-23.
Macey PM, Woo MA, Harper RM. Hyperoxic brain effects are normalized by addition of CO2. PLoS Med 2007; 4: e173.
Macey PM, Macey KE, Kumar R, Harper RM. A method for removal of global effects from fMRI time series. Neuroimage 2004; 22: 360-6.
Prisman E, Slessarev M, Han J, et al. Comparison of the effects of independently-controlled end-tidal PCO2 and PO2 on blood oxygen level-dependent (BOLD) MRI. J Magn Reson 2008; 27: 185-91.
Mutch WAC, El-Gabalawy R, Ryner L, et al. Brain BOLD MRI O2 and CO2 stress testing: implications for perioperative neurocognitive disorder following surgery. Crit Care 2020; 24: 76.
Dony P, Dramaix M, Boogaerts JG. Hypocapnia measured by end-tidal carbon dioxide tension during anesthesia is associated with increased 30-day mortality rate. J Clin Anesth 2017; 36: 123-6.
Akkermans A, van Waes JAR, Thompson A, et al. An observational study of end-tidal carbon dioxide trends in general anesthesia. Can J Anesth 2019; 66: 149-60.
Mutch WA, El-Gabalawy R, Girling L, Kilborn K, Jacobsohn E. End-tidal hypocapnia under anesthesia predicts postoperative delirium. Front Neurol 2018; 9: 678.
El-Gabalawy R, Patel R, Kilborn K, et al. A novel stress-diathesis model to predict risk of post-operative delirium: Implications for intra-operative management. Front Aging Neurosci 2017; 9: 274.
Wang Z, Aguirre GK, Rao H, et al. Empirical optimization of ASL data analysis using an ASL data processing toolbox: ASLtbx. Magn Reson Imaging 2008; 26: 261-9.
Duffin J, Hare GMT, Fisher JA. A mathematical model of cerebral blood flow control in anaemia and hypoxia. J Physiol 2020; 598: 717-30.
Duffin J. Fail-safe aspects of oxygen supply. J Physiol 2020; 598: 4859-67.
Sprung J, Kruthiventi SC, Warner DO, et al. Exposure to surgery under general anaesthesia and brain magnetic resonance imaging changes in older adults. Br J Anaesth 2019; 123: 808-17.
Venkatraghavan L, Poublanc J, Bharadwaj S, et al. Noninvasive measurement of cerebral blood flow under anesthesia using arterial spin labeling MRI: a pilot study. J Neurosurg Anesthesiol 2016; 28: 331-6.
Venkatraghavan L, Poublanc J, Han JS, et al. Measurement of cerebrovascular reactivity as blood oxygen level-dependent magnetic resonance imaging signal response to a hypercapnic stimulus in mechanically ventilated patients. J Stroke Cerebrovasc Dis 2018; 27: 301-8.
Liu P, Liu G, Pinho MC, et al. Cerebrovascular reactivity mapping using resting-state BOLD functional MRI in Healthy adults and patients with Moyamoya disease. Radiology 2021; 299: m419-25.
Kant IM, Slooter AJ, Jaarsma-Coes M, et al. Preoperative MRI brain phenotypes are related to postoperative delirium in older individuals. Neurobiol Aging 2021 May; 101: 247-55.
Kety SS, Schmidt CF. The effects of altered arterial tensions of carbon dioxide and oxygen on cerebral blood flow and cerebral oxygen consumption of normal young men. J Clin Invest 1948; 27: 484-92.
Iscoe S, Fisher JA. Hyperoxia-induced hypocapnia: An underappreciated risk. Chest 2005; 128: 430-3.
Joosten A, Rinehart J, Bardaji A, et al. Anesthetic management using multiple closed-loop systems and delayed neurocognitive recovery: a randomized controlled trial. Anesthesiology 2020; 132: 253-66.
Takahashi CE, Brambrink AM, Aziz MF, et al. Association of intraprocedural blood pressure and end tidal carbon dioxide with outcome after acute stroke intervention. Neurocrit Care 2014; 20: 202-8.
Choi SH, Lee H, Chung TS, et al. Neural network functional connectivity during and after an episode of delirium. Am J Psychiatry 2012; 169: 498-507.
Ellis MJ, Mutch WA, Ryner LN, et al. Brain magnetic resonance imaging CO2 stress testing in adolescent postconcussion syndrome. J Neurosurg 2016; 125: 648-60.
Author contributions
W. Alan C. Mutch contributed to conception, experimentation, data collation, data analysis, writing, and final approval. James Duffin contributed to conception, mathematical model, data analysis, writing, and final approval.
Disclosures
None.
Funding statement
Support was provided solely from departmental sources – Anesthesia Oversight Committee at the University of Manitoba.
Editorial responsibility
This submission was handled by Dr. Alana M. Flexman, Associate Editor, Canadian Journal of Anesthesia/Journal canadien d’anesthésie.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Mutch, W.A.C., Duffin, J. Differential regional cerebral blood flow reactivity to alterations in end-tidal gases in healthy volunteers. Can J Anesth/J Can Anesth 68, 1497–1506 (2021). https://doi.org/10.1007/s12630-021-02042-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-021-02042-x