Abstract
Purpose
Intraoperative hypoglycemia can result in devastating neurologic injury if not promptly diagnosed and treated. Few studies have defined risk factors for intraoperative hypoglycemia. The authors sought to characterize children with intraoperative hypoglycemia and determine independent risk factors.
Methods
This retrospective observational single-institution study included all patients < 18 yr of age undergoing an anesthetic from January 1 2012 to December 31 2016. The primary outcome was blood glucose < 3.3 mmol·L−1 (60 mg·dl−1). Data collected included patient characteristics, comorbidities, and intraoperative factors. A multivariable logistic regression model was used to identify independent predictors of intraoperative hypoglycemia.
Results
Blood glucose was measured in 7,715 of 73,592 cases with 271 (3.5%) having a glucose < 3.3 mmol·L−1 (60 mg·dl−1). Young age, weight for age < 5th percentile, developmental delay, presence of a gastric or jejunal tube, and abdominal surgery were identified as independent predictors for intraoperative hypoglycemia. Eighty percent of hypoglycemia cases occurred in children < three years of age and in children < 15 kg.
Conclusion
Young age, weight for age < 5th percentile, developmental delay, having a gastric or jejunal tube, and abdominal surgery were independent risk factors for intraoperative hypoglycemia in children. Frequent monitoring of blood glucose and judicious isotonic dextrose administration may be warranted in these children.
Résumé
Objectif
L’hypoglycémie peropératoire peut entraîner des lésions neurologiques catastrophiques si elle n’est pas diagnostiquée et traitée rapidement. Très peu d’études ont défini les facteurs de risque d’hypoglycémie peropératoire. Les auteurs ont essayé de caractériser les enfants atteints d’hypoglycémie peropératoire et de déterminer les facteurs de risque indépendants.
Méthode
Cette étude observationnelle rétrospective monocentrique a inclus tous les patients < 18 ans subissant une anesthésie entre le 1er janvier 2012 et le 31 décembre 2016. Le critère d’évaluation principal était une glycémie < 3,3 mmol·L−1 (60 mg·dl−1). Les données colligées comprenaient les caractéristiques des patients, les comorbidités et les facteurs peropératoires. Un modèle de régression logistique multivariée a été utilisé pour identifier les prédicteurs indépendants d’hypoglycémie peropératoire.
Résultats
La glycémie a été mesurée dans 7715 des 73 592 cas, et 271 cas (3,5 %) ont eu un taux de glycémie < 3,3 mmol·L−1 (60 mg·dl−1). Un jeune âge, un poids < 5e percentile pour l’âge, un retard de développement, la présence d’une sonde gastrique ou jéjunale, et une chirurgie abdominale ont été identifiés comme des prédicteurs indépendants d’hypoglycémie peropératoire. Quatre-vingts pour cent des cas d’hypoglycémie sont survenus chez des enfants < trois ans et chez des enfants < 15 kg.
Conclusion
Un jeune âge, un poids < 5e percentile pour l’âge, un retard de développement, la présence d’une sonde gastrique ou jéjunale, et une chirurgie abdominale sont des facteurs de risque indépendants d’hypoglycémie peropératoire chez les enfants. Le monitorage fréquent de la glycémie et l’administration judicieuse de solution dextrosée isotonique pourraient être justifiés chez ces enfants.
Similar content being viewed by others
Intraoperative hypoglycemia can result in devastating neurologic injury if not promptly recognized and treated.1,2,3,4 The continuum of symptoms that children exhibit during hypoglycemia (difficulty feeding, diaphoresis, lethargy, irritability, stupor, seizures, and coma) are predominantly masked by anesthesia. Unless hypoglycemia is actively sought, it cannot be diagnosed under anesthesia, making it imperative to identify at-risk patients preoperatively.5,6,7,8 From the 1970s to the 1990s, the effects of fasting times and various concentrations of intravenous dextrose on intraoperative hypoglycemia were extensively studied in children. These studies yielded conflicting results and no global consensus on recommendations was achieved.9,10,11,12 Other studies have found associations between intraoperative hypoglycemia and various factors including young age, underweight patients, and discontinuation of preoperative dextrose infusion.13,14,15,16,17 Nevertheless, specific independent predictors of hypoglycemia in children have not yet been identified. Despite these data, intraoperative hypoglycemia continues to occur in children with a reported incidence of 0.7–28%.13,18,19,20
The hypothesis of this study was that there are subsets of children at risk of intraoperative hypoglycemia. Our objectives were 1) to describe children who have intraoperative hypoglycemia and 2) to determine independent risk factors for intraoperative hypoglycemia in children.
Methods
This was a single-centre retrospective observational study. University of Michigan Institutional Review Board (IRB) approval was obtained in May, 2017 (IRB# HUM00129121). A waiver of informed HIPAA (Health Insurance Portability and Accountability Act) consent was obtained from the IRB and TRIPOD (Transparent Reporting of a multivariable prediction model for Individual Prognosis Or Diagnosis) reporting guidelines were followed. The study protocol and statistical plan were pre-approved and archived by our institution’s Anesthesia Clinical Research Committee on April 19 2017.
All patients aged < 18 yr who had an anesthetic from January 1 2012 to December 31 2016 were eligible for study inclusion. Data were collected from patient electronic health records, including the perioperative clinical care system (Centricity, General Electric Healthcare, Waukesha, WI, USA). Demographic data collected included age, sex, weight, and height. Weight for age, height for age, weight for height, and associated percentiles were computed using the World Health Organization standards for those < two years of age and the Centers for Disease Control standards for those ≥ two years of age, as appropriate. Other preoperative patient characteristics collected included American Society of Anesthesiologists (ASA) physical status, inpatient status, prematurity, diabetes, history of hypoglycemia, developmental delay, use of heart failure medications, beta blocker use, congenital heart disease, poor feeding, gastrointestinal malabsorption disease, documented presence of a gastric or jejunal tube before the procedure, gastro-esophageal reflux, history of failure to thrive, and recent respiratory infections. Intraoperative variables collected included general anesthesia vs sedation, type of procedure, duration of the anesthetic (anesthesia start to anesthesia end), arterial line use, and emergent surgery. All intraoperative glucose measurements were recorded including those measured using a glucometer, blood gas machine, or in the pathology laboratory.
During the five-year period of this study, it was not routine perioperative practice at our institution to administer intravenous dextrose nor to check blood glucose levels in every pediatric patient. These interventions were done for some neonates, young infants, and other patients at the discretion of the anesthesiologist.
The primary outcome was intraoperative hypoglycemia defined as at least one measured blood glucose less than < 3.3 mmol·L−1 (60 mg·dl−1),13,14,21 from anesthesia start to anesthesia end. Hand-entered blood glucose values < 3.3 mmol·L−1 (60 mg·dl−1) were assessed for validity by comparison with the official laboratory reports whenever available in our electronic medical record. We removed patients’ records from analysis when transcription errors were found. For the purposes of analyses, prematurity was defined as a recorded gestational age < 37 weeks for those ≤ one year of age. Any patient > one year was considered not to be premature.22 Poor feeding was defined as a composite of any recorded notation of poor feeding, poor growth, or poor appetite in the anesthesia history and physical (H&P). Developmental delay was defined as a variable in this study if it was a noted in the anesthesia H&P. Age was categorized as < 30 days, 30 days to < five years, and ≥ five years. The first cut-off was determined by clinical significance, and the second cut-off was determined statistically.
Statistical methods
All analyses were conducted using SAS v. 9.4 (SAS Institute, Cary, NC, USA) and SPSS v. 24 (IBM). The upper cut-off for age and hypoglycemia was determined using Youden’s index. Descriptive statistics were presented for categorical variables as frequencies (percentages) and for continuous variables as means (standard deviations) or medians [interquartile ranges (IQR)], as appropriate. All continuous variables were assessed for normality using the Kolmogorov–Smirnov test. Univariate comparisons between those with and without a glucose drawn intraoperatively and those with and without intraoperative hypoglycemia were computed using Chi squared or Fisher’s exact tests for categorical variables, and independent t tests or Mann–Whitney U tests for continuous variables, as appropriate. The Hodges–Lehman method was used to compute the 95% confidence intervals (CI) of the median. Clinically significant differences were noted on tables with large sample sizes in both groups. A Pareto analysis on age and weight was conducted for those with hypoglycemia. Unadjusted odds ratios were not assessed.
To determine possible independent predictors of hypoglycemia in those who had a glucose drawn, a multivariable logistic regression model was constructed with the dependent variable of any hypoglycemic event. Variables selected a priori for model inclusion were age and weight. Age was grouped as < 30 days, 30 days to < five years, and ≥ five years, and weight for age < 5th percentile (yes vs no) was chosen as the weight parameter. Other variables selected post-hoc for model inclusion based on clinical and statistical significance were ASA status (I and II vs ≥ III), gastric or jejunal tube presence, arterial line use (a proxy for complex patient and/or complicated surgery where blood glucose levels are usually measured), inpatient status, developmental delay, congenital heart disease, failure to thrive, prematurity (defined as above), general anesthesia, poor feeding, abdominal surgery, and anesthesia duration.
Prior to model construction, variables considered for model entry were checked for collinearity using Pearson correlation matrices. Those variables with a correlation > 0.70 were considered collinear, and were either combined into a single composite variable if similar or the variable with the higher unadjusted effect size was retained in the model while the other was removed. The final number of covariates chosen for model inclusion was based on sample size, so as to not over-fit the model based on the 10:1 rule. For this model, missing data were left as missing.
Measures of effect size were reported as adjusted odds ratios (aOR) with 95% CI, and the model’s predictive capability was assessed using the area under the receiver operating characteristics curve c-statistic and associated 95% CI. Model validation was performed using a leave-one-out cross-validation, and the validation c-statistic with 95% CI was reported. Any covariate with a statistically significant aOR at the 0.05 level was considered an independent predictor of a hypoglycemic event given that a glucose was drawn intraoperatively.
A P value of < 0.05 was considered statistically significant for all analyses conducted.
Power analysis
There was no a priori power analysis constructed for this retrospective observational study. Our glucose cohort sample size of 7,715 patients yielded an outcome rate of 3.5% (271 patients), which allowed for up to 27 degrees of freedom in the model without being over-fit based on the 10:1 rule.23
Results
Of 73,647 cases in our institution between January 1 2012 and December 31 2016, there were 7,770 with at least one blood glucose documented intraoperatively (Fig. 1). Using hand-validation by an anesthesiologist, 55 glucose measurements < 3.3 mmol·L−1 (60 mg·dl−1) were found to be transcription errors. Of these, 53 were recorded < 1.1 mmol·L−1 (20 mg·dl−1) and the other two were 1.3 mmol·L−1 (23 mg·dl−1) and 1.5 mmol·L−1 (27 mg·dl−1). All were removed from the analysis. The final glucose cohort consisted of 7,715 cases, of which 271 (3.5%) had a glucose < 3.3 mmol·L−1 (60 mg·dl−1). Figure 2 shows the distribution of the glucose measurements < 3.3 mmol·L−1 (60 mg·dl−1).
Table 1 shows a comparison between those children who had a glucose measured intraoperatively and those who did not. Those who had a glucose drawn were significantly younger (< 30 days of age [12.3% vs 1.8%]), smaller (weight < 5th percentile for age [24.1% vs 13.1%]), and generally sicker (ASA ≥ III [76.8% vs 31.1%]), were an inpatient (35.4% vs 18.1%) and had an arterial line (71.8% vs 2.8%). Additionally, those with a glucose drawn had longer cases (median [IQR] 267 min [166 to 375] vs 90 min [59 to 136]).
Age was significantly associated with the occurrence of hypoglycemia. Indeed, we found a significant inverse relationship between age and the prevalence of hypoglycemia in those patients who had a glucose measured: 8.8% of the 950 infants < 30 days of age, 4.0% of the 3,646 patients between 30 days and five years of age, and 1.3% of the 3,119 patients five years of age or older experienced hypoglycemia (calculated from the age data in Table 2). A Pareto analysis showed that 80% of the hypoglycemia cases were in those < three years of age and in those < 15 kg.
Similar univariate characteristics were seen between those with and without intraoperative hypoglycemia (Table 2). Additionally, those with hypoglycemia were more likely to have ASA status ≥ III, have height < 5th percentile for age, have weight < 5th percentile for age, be an inpatient, be premature, not have diabetes, have developmental delay, have congenital heart disease, feed poorly, have a gastric or jejunal tube, have an arterial line, and have an abdominal procedure. There were no statistically significant differences between those who had intraoperative hypoglycemia and those who did not with regards to sex, history of hypoglycemia, use of heart failure medications, history of failure to thrive, or general anesthesia.
The most common procedures in patients who had a hypoglycemic event were cardiac surgeries (34.7% vs 32.0% in the non-hypoglycemic group, P = 0.36), abdominal surgeries (21.8% vs 10.0% in the non-hypoglycemic group, P < 0.001), non-invasive radiologic procedures (7.4% vs 9.3% in the non-hypoglycemic group, P = 0.30) and cardiac catheterizations (6.6% vs 9.2% in the non-hypoglycemic group, P = 0.16) (Table 3).
During the manual review of the hypoglycemia cohort, details about glucose administration were obtained from the medical records. We found that, of 271 patients with hypoglycemia, 162 (60.0%) had hypoglycemia recorded at induction or within the first hour of the anesthetic once the arterial catheter was placed. Of 271 with a hypoglycemia event at any time during the anesthetic, 54 (20.0%) had some form of dextrose (5%, 10%, or unspecified concentrations of dextrose in total parental nutrition), infusing before and at the time of the hypoglycemia. We were not able to decipher the dose of dextrose infusing nor for how long it had been infusing because documentation was inconsistent.
Treatment of hypoglycemia was variable. Dextrose was added or its concentration increased to treat hypoglycemia in 65.3% of the patients. The exact dose or change in concentration could not be decoded from the records. In 12.2% of cases, the blood tests were drawn on behalf of the primary service while the child was anesthetized but reviewed only by the primary service, not the anesthesia provider, so there was no intraoperative treatment in those patients. And in 22.5% of patients, there was no apparent treatment for hypoglycemia although half of hypoglycemia cases occurred just prior to the patient being placed on cardiopulmonary bypass.
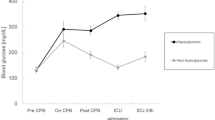
We also identified patients who had hyperglycemia at any point during the anesthetic. We found in those who had a glucose measured, there were 3,081 (39.9%) with at least one glucose > 8.3 mmol·L−1 (150 mg·dl−1), 1,678 (21.8%) with at least one glucose > 11.1 mmol·L−1 (200 mg·dl−1), and 767 (9.9%) with at least one glucose > 13.9 mmol·L−1 (250 mg·dl−1). There were no statistically significant differences in hyperglycemia threshold between those with and without hypoglycemia (glucose > 8.3 mmol·L−1, P = 0.47, glucose > 11.1 mmol·L−1, P = 0.10, glucose > 13.9 mmol·L−1, P = 0.40).
Multivariable model results
Of the 7,715 cases with intraoperative glucose measurements, 6,920 (90%) had non-missing data for all model covariates with 230 hypoglycemic events. Variables with missing data were prematurity (5%), weight for age (3%), failure to thrive (2%), gastric or jejunal tube in place (2%), congenital heart disease (1%), and poor feeding (0.3%). There was no collinearity between covariates, and all were eligible for model entry.
After adjusting for all model covariates, those < 30 days of age had 6.5 times the odds of intraoperative hypoglycemia compared with those ≥ five years of age (95% CI, 3.9 to 10.9; P < 0.001) and those 30 days to less than five years of age had 2.9 times the odds of intraoperative hypoglycemia compared with the older cohort (95% CI, 2.0 to 4.3; P < 0.001; Fig. 3). After adjustment, those < 5th percentile weight for age had two times the odds of intraoperative hypoglycemia compared with those ≥ 5th percentile (95% CI, 1.5 to 2.8; P < 0.001), those who had developmental delay had 1.9 times the odds of intraoperative hypoglycemia as those who did not (95% CI, 1.2 to 3.1; P = 0.006), those with a gastric or jejunal tube had 1.6 times the odds of intraoperative hypoglycemia as those who did not (95% CI, 1.1 to 2.2; P = 0.011), and those having abdominal surgery had 2.3 times the odds of intraoperative hypoglycemia compared with those who did not (95% CI, 1.6 to 3.3; P < 0.001). All other model covariates were not statistically significant (P > 0.05). The model area under the receiver operating characteristic curve c-statistic was 0.75 (95% CI, 0.72 to 0.78). The leave-one-out cross-validation model c-statistic was 0.73 (95% CI, 0.70 to 0.76).
Discussion
This five-year single-centre study examining all patients < 18 yr who had a glucose level less than 3.3 mmol·L−1 (60 mg·dl−1) showed that some children have a higher risk for intraoperative hypoglycemia. We found young age, weight for age less than the 5th percentile, developmental delay, presence of a gastric or jejunal tube, and abdominal surgery to be independent predictors for intraoperative hypoglycemia in children. Additionally, using univariate analyses we found a number of additional factors significantly associated with intraoperative hypoglycemia, including ASA ≥ III, inpatient status, low weight, height for age < 5th percentile, prematurity, poor feeding, not having diabetes, congenital heart disease, and the presence of an arterial line.
Previous studies have varied in their definitions of hypoglycemia. We chose 3.3 mmol·L−1 because clinically, it is the value below which we would treat, and although the specific glucose value below which there is increased risk for brain injury remains unknown, there is evidence that brain glucose utilization becomes limited and symptoms begin to appear in non-anesthetized patients at a glucose of 3.0–3.6 mmol·L−1.6,7,8 Knowing that glucose utilization likely decreases during anesthesia we opted for the middle of that range: 3.3 mmol·L−1. Our data indicate that 80% of the hypoglycemic events occurred in children < three years old and in those < 15 kg. Thomas similarly reported hypoglycemia only in children under 47 months and less than 15.5 kg.13 Other studies14,17 showed an association between children small for age and hypoglycemia. Failure to thrive can be defined as less than the 5th percentile weight for age24 and we found this to be a risk factor for intraoperative hypoglycemia. The correlation between failure to thrive and hypoglycemia is not well understood.25 Other risk factors found in our study—developmental delay and presence of a gastric or jejunal tube—suggest that these may be patients who have potential difficulties obtaining adequate nutrition. Indeed, abdominal surgery, another independent risk factor, may also be related to nutritional status of the patient. Young age was found to be another risk factor for hypoglycemia. Neonates, who may have low glycogen stores, as well as children who are malnourished, may be challenged to mount an adequate response to fasting. There is evidence that children with extreme protein-calorie malnutrition have decreased endogenous glucose production as well as decreased glucose reabsorption.26,27 Nevertheless, it remains uncertain whether these findings can be extrapolated to populations with less severe malnutrition. Of note, a recent study found malnourished children with hypoglycemia had increased risk of mortality compared with those who were not malnourished,25 suggesting that the association between nutritional status and hypoglycemia warrants further investigation. Lastly, hypoglycemia has also been reported to be an independent risk factor for mortality with severity of hypoglycemia being directly correlated with mortality rate in critically ill children.28
It should be emphasized that 20% of the hypoglycemic events occurred in patients who were receiving a dextrose infusion at the time of the event, although we could not decipher the exact dose of dextrose administered. This concurs with recent observational data from Bestor, which showed that seven out of 99 infants under anesthesia had hypoglycemia, some of whom were receiving dextrose infusions of varying concentrations.19 Taken together, these data highlight that administering dextrose does not always reliably eliminate the risk of hypoglycemia. It may therefore be prudent to consider glucose monitoring in at-risk children even if they are receiving a dextrose infusion.
While this was not a primary outcome of our study, we found that a significant number of children experienced intraoperative hyperglycemia. It remains uncertain whether the hyperglycemia occurred because of overzealous dextrose administration, stress response to surgery, or another factor. It is not the practice at our institution to treat intraoperative hyperglycemia with insulin since it has been reported that tight glycemic control can be associated with severe hypoglycemia.29,30
This study was subject to weaknesses and limitations inherent in any historical cohort study. Selection bias may have occurred when a glucose level was measured because the anesthesia provider suspected that the patient might be at risk for hypoglycemia (for example longer surgery, smaller child, complex comorbidities) or when the blood was drawn and measured for other reasons and a glucose was included. Our institutional practice is to obtain arterial access for specific procedures including cardiac surgery, craniotomy, spinal fusion, and neonatal thoraco-abdominal procedures, making it more likely for these patients to have their blood glucose measured as part of other laboratory testing. Because of the retrospective nature of this study, we were unable to determine why glucose levels might have been measured. Nevertheless, even if, hypothetically in the case of severe selection bias, every single glucose level in this study was measured because hypoglycemia was suspected, our data suggest that that conjecture would have been correct a maximum 3.6% of the time (271/7,515 cases). We hope that our findings will help more correctly identify these vulnerable children. We were unable to report the duration of fasting. Nor could we determine incidence of intraoperative hypoglycemia as glucose was only measured in 10.6% of our patients. Some of the covariates were defined by being notations in the anesthesia H&P, rather than more objectively. Moreover, despite the large number of potential covariates we studied, there remains the possibility of unrecognized confounders. The goal of this study was not to characterize the potential clinical sequelae of intraoperative hypoglycemia and we do not know if any of the hypoglycemic episodes detected resulted in clinical harm. Lastly, glucose was not measured intraoperatively in 65,877 patients in this study and hypoglycemia may have gone undetected in some of these patients. Hopefully, our data suggesting that there are factors that may help identify children at risk for intraoperative hypoglycemia will lead to an increased awareness and careful planning for intraoperative glucose management.
We present the largest study to date of risk factors for intraoperative hypoglycemia in children. We have not only reaffirmed the findings of previous investigators, but have identified additional factors associated with intraoperative hypoglycemia in children. Further investigation may be warranted to determine whether children with these factors are at risk for hypoglycemia in other settings. When caring for children who are under the age of five years, who are underweight for their age, have a developmental delay, have a feeding tube and have had abdominal surgery we propose that providers maintain a high level of suspicion for hypoglycemia, and consider measurement of glucose and administration of isotonic dextrose during the perioperative period to avoid hypoglycemia and its entirely preventable negative sequelae.
References
Siesjo BK. Hypoglycemia, brain metabolism, and brain damage. Diabetes Metab Rev 1988; 4: 113-44.
Lucas A, Morley R, Cole TJ. Adverse neurodevelopmental outcome of moderate neonatal hypoglycaemia. BMJ 1988; 297: 1304-8.
Koh TH, Aynsley-Green A, Tarbit M, Eyre JA. Neural dysfunction during hypoglycaemia. Arch Dis Child 1988; 63: 1353-8.
Burns CM, Rutherford MA, Boardman JP, Cowan FM. Patterns of cerebral injury and neurodevelopmental outcomes after symptomatic neonatal hypoglycemia. Pediatrics 2008; 122: 65-74.
Ehrlich RM. Hypoglycaemia in infancy and childhood. Arch Dis Child 1971; 46: 716-9.
Cryer PE, Davis SN, Shamoon H. Hypoglycemia in diabetes. Diabetes Care 2003; 26: 1902-12.
Suh SW, Hamby AM, Swanson RA. Hypoglycemia, brain energetics, and hypoglycemic neuronal death. Glia 2007; 55: 1280-6.
Thornton PS, Stanley CA, De Leon DD, et al. Recommendations from the Pediatric Endocrine Society for Evaluation and Management of Persistent Hypoglycemia in Neonates, Infants, and Children. J Pediatr 2015; 167: 238-45.
Watson BG. Blood glucose levels in children during surgery. Br J Anaesth 1972; 44: 712-5.
Jensen BH, Wernberg M, Andersen M. Preoperative starvation and blood glucose concentrations in children undergoing inpatient and outpatient anaesthesia. Br J Anaesth 1982; 54: 1071-4.
Welborn LG, McGill WA, Hannallah RS, Nisselson CL, Ruttimann UE, Hicks JM. Perioperative blood glucose concentrations in pediatric outpatients. Anesthesiology 1986; 65: 543-7.
Welborn LG, Hannallah RS, McGill WA, Ruttimann UE, Hicks JM. Glucose concentrations for routine intravenous infusion in pediatric outpatient surgery. Anesthesiology 1987; 67: 427-30.
Thomas D. Hypoglycaemia in children before operation: its incidence and prevention. Br J Anaesth 1974; 46: 66-8.
Allison CW, Cater JI, Gray IG, Staziker AC. Pre-operative starvation in children. The role of alanine in blood glucose homeostasis. Anaesthesia 1982; 37: 274-7.
Larsson LE, Nilsson K, Niklasson A, Andreasson S, Ekstrom-Jodal B. Influence of fluid regimens on perioperative blood-glucose concentrations in neonates. Br J Anaesth 1990; 64: 419-24.
Hongnat JM, Murat I, Saint-Maurice C. Evaluation of current paediatric guidelines for fluid therapy using two different dextrose hydrating solutions. Pediatr Anesth 1991; 1: 95-100.
Payne K, Ireland P. Plasma glucose levels in the peri-operative period in children. Anaesthesia 1984; 39: 868-72.
Welborn LG, Norden JM, Seiden N. Effect of minimizing preoperative fasting on perioperative blood glucose hemostasis in children. Pediatr Anesth 1993; 3: 167-71.
Bestor K, Pretorius T. Intraoperative glucose management in children < 1 year or < 10 kg: an observational study. South Afr J Anaesth Analg 2017; 23: 119-22.
Smallshaw K, Woodham V, Seth N, Tooke L, Blaise BJ. Incidence of hypoglycemia in fasted young children referred for elective surgery. Pediatr Anesth 2018; 28: 933-4.
Bowie MD, Mulligan PB, Schwartz R. Intravenous glucose tolerance in the normal newborn infant: the effect of a double dose of glucose and insulin. Pediatrics 1963; 31: 590-8.
Siegel LS. Correction for prematurity and its consequences for the assessment of the very low birth weight infant. Child Dev 1983; 54: 1176-88.
Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol 1996; 49: 1373-9.
Steward DK, Ryan-Wenger NA, Boyne LJ. Selection of growth parameters to define failure to thrive. J Pediatr Nurs 2003; 18: 52-9.
Leite HP, de Lima LF, de Oliveira Iglesias SB, Pacheco JC, de Carvalho WB. Malnutrition may worsen the prognosis of critically ill children with hyperglycemia and hypoglycemia. JPEN J Parenter Enteral Nutr 2013; 37: 335-41.
Bandsma RH, Mendel M, Spoelstra MN, et al. Mechanisms behind decreased endogenous glucose production in malnourished children. Pediatr Res 2010; 68: 423-8.
Bandsma RH, Spoelstra MN, Mari A, et al. Impaired glucose absorption in children with severe malnutrition. J Pediatr 2011; 158(282–7): e1.
Faustino EV, Bogue CW. Relationship between hypoglycemia and mortality in critically ill children. Pediatr Crit Care Med 2010; 11: 690-8.
Agus MS, Steil GM Wypij D, et al. Tight glycemic control versus standard care after pediatric cardiac surgery. N Engl J Med 2012; 367: 1208-19.
Agus MS, Wypij D, Hirshberg EL, et al. Tight glycemic control in critically ill children. N Engl J Med 2017; 376: 729-41.
Financial support and sponsorship
This work was supported by the University of Michigan Department of Anesthesiology, Ann Arbor, Michigan, USA.
Conflicts of interest
Lori Q. Riegger, Aleda M. Leis, Shobha Malviya have no conflict of interests. Kevin K. Tremper is the founder and equity holder in AlertWatch, a quality/safety decision support software company.
Author contributions
Lori Q. Riegger contributed to the study design, data collection, data analysis and interpretation, and writing and editing the manuscript. Aleda M. Leis contributed to the study design, data collection, statistical and data analysis and interpretation, and writing and editing the manuscript. Shobha Malviya contributed to the study design, data analysis, interpretation of data, and writing and editing the manuscript. Kevin K. Tremper contributed to the study design, data interpretation, and editing the manuscript.
Editorial responsibility
This submission was handled by Dr. Philip M. Jones, Associate Editor, Canadian Journal of Anesthesia.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Riegger, L.Q., Leis, A.M., Malviya, S. et al. Risk factors for intraoperative hypoglycemia in children: a retrospective observational cohort study. Can J Anesth/J Can Anesth 67, 225–234 (2020). https://doi.org/10.1007/s12630-019-01477-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-019-01477-7