Abstract
Purpose
Supraglottic airway devices (SGAs) can be used as conduits for intubation, but data and manufacturers’ recommendations for pediatric SGA are incomplete and sometimes misleading. This situation can result in the use of incompatible combinations of SGAs and endotracheal tubes (ETTs). To address this mismatch possibility, we performed an in vitro study to establish an overview of possible combinations of SGAs and ETTs.
Methods
We tested the passage of ETTs through SGAs in vitro and subsequent SGA removal with eight pediatric SGAs and six ETTs of different sizes in vitro. Results were compared with manufacturers’ recommendations. Outcome parameters were the feasibility of passing the ETT through the SGA and then removing the SGA over the ETT.
Results
The Air-Q® and the Air-Q®sp™ SGAs showed the best compatibility with ETTs across all sizes. Whenever intubation was possible, removal was possible for all SGAs with uncuffed ETTs. With many cuffed ETTs, however, SGA removal was impossible because the ETT cuff’s pilot balloon was larger than the inner diameter of the SGA. Thus, although intubation was possible, removal of the SGA was not. The manufacturers’ booklets do not warn of this limitation.
Conclusions
The use of combinations of SGA and ETTs with a size mismatch can lead to airway complications during intubation or to accidental extubation and tearing of the cuff pilot balloon line when removing the SGA. To avoid these problems, we devised a table that simplifies the choice of an appropriate SGA and ETT combination.
Résumé
Objectif
Les dispositifs supraglottiques peuvent être utilisés comme conduits pour l’intubation, mais les données et les recommandations des fabricants concernant les dispositifs supraglottiques pédiatriques sont incomplètes et portent parfois à confusion. Cette situation peut aboutir à l’utilisation de combinaisons incompatibles de dispositifs supraglottiques et de tubes endotrachéaux (TET). Afin d’examiner ces incompatibilités potentielles, nous avons réalisé une étude in vitro pour passer en revue les combinaisons possibles entre dispositifs supraglottiques et TET.
Méthode
Nous avons testé le passage de divers TET dans les dispositifs supraglottiques in vitro et le retrait subséquent de ces dispositifs supraglottiques avec huit dispositifs supraglottiques pédiatriques et six TET de différentes tailles in vitro. Les résultats ont été comparés aux recommandations des fabricants. Les paramètres d’évaluation comprenaient la facilité de passage du TET dans le dispositif supraglottique et le retrait du dispositif par dessus le TET.
Résultats
Les dispositifs supraglottiques Air-Q® et Air-Q®sp™ ont montré la meilleure compatibilité avec les TET de toutes tailles. Lorsque l’intubation était possible, le retrait était possible pour tous les dispositifs supraglottiques avec des TET sans ballonnet. Avec plusieurs des TET à ballonnet, toutefois, le retrait du dispositif supraglottique s’est avéré impossible : en effet, la largeur plus importante du ballonnet du TET par rapport au diamètre interne du dispositif supraglottique a entravé le retrait du dispositif supraglottique. Par conséquent, bien que l’intubation fût possible, le retrait du dispositif supraglottique ne l’était pas. Les manuels des fabricants ne mentionnent pas cette limite.
Conclusion
L’utilisation de combinaisons de dispositifs supraglottiques et de TET de tailles non correspondants peut entraîner des complications au niveau des voies aériennes pendant l’intubation ou une extubation accidentelle et un déchirement du ballonnet lors du retrait du dispositif supraglottique. Afin d’éviter ces problèmes, nous avons mis au point un tableau simplifiant le choix d’une combinaison adaptée entre dispositif supraglottique et TET.
Similar content being viewed by others
Management of the pediatric airway can be challenging because of specific anatomical features of the pediatric airway, craniofacial syndromes, low functional residual capacity, and the greater oxygen demand of children.1 Additionally, patient cooperation for techniques such as preoxygenation.2 or awake flexible bronchoscopic (FB) intubation (the standard approach in adults with an anticipated difficult airway)3,4 is limited. Thus, hypoxia and insufficient ventilation during anesthesia are more frequent in children than in adults.5 Supraglottic airway devices (SGAs) are the central rescue tools according to the airway guidelines of the Association of Paediatric Anaesthetists,6 and FB intubation through SGAS is recommended in case of failed intubation.6
Case reports and case series have proven the concept of FB intubation via SGAs for difficult pediatric airway management.7,8,9,10,11,12 Some SGAs have also been used for elective FB-guided intubation.13,14 Passage of the endotracheal tube (ETT) through the lumen of the SGA and removal of the SGA after successful intubation, however, can be impeded by a mismatch of the inner diameter of the SGA and the outer diameter of the ETT or the ETT cuff’s pilot balloon. This problem was mentioned by Jagannathan et al. for the Ambu® Aura-i™ size 1.5.13 The authors chose to cut the cuff’s pilot balloon to remove the SGA after intubation and subsequently repair the cuff with a 22G angiocatheter. Similarly, Weiss et al. reported a size mismatch between the cuff’s pilot balloon and the LMA classic™ sizes 1.0 to 2.0 or 2.5.15
Incompatibilities of pediatric SGAs and ETTs might be known to many pediatric anesthesiologists but not to a broader anesthesia community. Although anesthesiologists need to know which combination of pediatric-sized SGAs and ETTs can safely be used for intubation, data regarding the compatibility of SGAs and ETTs for intubation and SGA removal after intubation are largely missing. This in vitro study evaluates 1) the feasibility of passing ETTs through pediatric SGAs, as performed during intubation, and 2) the feasibility of SGA removal over the ETT. Combinations of several pediatric SGAs and pediatric cuffed and uncuffed ETTs were used. The study also provides a reference table facilitating the choice of appropriate SGA-ETT combinations.
Methods
This in vitro study evaluated the feasibility of passing various ETTS through a variety of pediatric SGAs and removing the SGAs over the ETTs, as performed during intubation with pediatric SGAs and subsequent SGA removal. The study was performed at the Department of Anesthesiology and Pain Medicine at the University Hospital Bern, Switzerland. It did not involve any study subjects, and therefore approval from the local institutional review board or registration in an international trials registry was not required.
Procedures and outcome measurements
After generous lubrication (Lary Phary Spray™, Dr. Panzer GmbH, Potsdam, Germany) of the ETTs and SGAs, each tested ETT was passed through each SGA as would be performed for intubation through the SGA. The feasibility of passing the ETT was noted. The SGA was then removed over the ETT as would be performed clinically during removal of the SGA from the patient’s pharynx, leaving the ETT in the trachea. The feasibility of removing the SGA over the ETT was noted. This evaluation was performed independently by two investigators (MKB and LT), each of whom was experienced in the use of SGAs, intubation, and intubation through SGAs.
For each SGA-ETT combination, the outcome parameters were 1) the feasibility of ETT passage through the SGA, as necessary for intubation, and 2) the feasibility of SGA removal over the ETT (i.e., passage of the ETT and the cuff’s pilot balloon through the SGA, as is necessary for SGA removal). The two investigators independently graded each SGA-ETT combination regarding the two outcome parameters. Whenever resistance was felt, requiring more than virtually no force to pass the ETT through the SGA, the respective combination was again tested by both investigators to establish consensus. Use of only minimal pushing without force was allowed for passing the ETT through the SGA and for removing the SGA over the ETT. Results were compared with manufacturers’ recommendations to evaluate the agreement of their recommendations with our results.
Evaluated SGA and ETTS
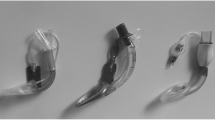
We evaluated eight commonly used single-use, pediatric SGAs (Fig. 1A) and four cuffed and two uncuffed ETTs (Fig. 1B). For all SGA sizes 1.0-2.5 and for all ETTs with an inner diameter of 3.0-5.5 were assessed. We did not physically modify any of the SGAs.
Supraglottic airway devices (SGAs) and endotracheal tubes included in this study. A: From left to right: Air-Q® inflatable, Air-Q®sp, Ambu® AuraGain™, Ambu® Aura-i™ (upper images); Ambu® AuraOnce™, Ambu® AuraStraight™, i-gel®, LMA Unique™ (lower images). Note the different angles of the SGA (all size 1.5). B: From left to right: Mallinckrodt™, Rüschelit™, Microcuff™, Sheridan™ cuffed, Portex™ uncuffed, Sheridan™ uncuffed (all size 3.5)
The SGAs studied included the following: Air-Q® inflatable and Air-Q®sp (self-pressurized, both Cookgas® LLC, St. Louis, USA, distributed by Mercury Medical, Clearwater, FL, USA); Ambu® AuraGain™, Ambu® Aura-i™, Ambu®, AuraOnce™, Ambu® AuraStraight™ (all from Ambu A/S, Ballerup, Denmark); i-gel® (Intersurgical Ltd., Wokingham, Berkshire, UK); LMA Unique™ (Teleflex Medical Europe Ltd., Athlone, Co Westmeath, Ireland). The Air-Q inflatable, Air-Qsp, Ambu AuraGain, and Ambu Aura-i are SGAs that are specifically marketed for tracheal intubation and are used for this purpose.13,14 The four pediatric standard SGAs - Ambu AuraOnce, Ambu AuraStraight, i-gel, LMA Unique - are not specifically marketed for tracheal intubation but are used for this purpose.12,16
The ETTs studied included the cuffed pediatric ETTs Mallinckrodt™ (Covidien, Mansfield, MA, USA), Rüschelit™ (Teleflex Incorporated, Limerick, PA, USA), Microcuff™ (Microcuff GmbH, Weinheim, Germany), and Sheridan™ (Teleflex Incorporated, Limerick, PA, USA) and the uncuffed ETTs Portex™ (Smiths Medical International Ltd., Hythe, UK) and Sheridan™ (Teleflex Inc., Limerick, PA, USA).
Clinically relevant combinations of SGA and ETTS
According to the manufacturers, the choice of the correctly sized SGA is based on the patient’s weight. In contrast, the rule commonly used to choose the correctly sized ETT is based on the patient’s age. Thus, to identify the clinically relevant SGA-ETT combinations, we translated the patient’s weight to his or her age using growth curves from the World Health Organization (Table).Footnote 1 Clinically relevant ETT sizes were then identified for all SGAs. This conversion was accomplished using the following formulas, according to the Resuscitation Council UK Paediatric Advanced Life Support GuidelinesFootnote 2 and departmental guidelines:
Endotracheal tubes within a half-size smaller and a half-size larger than the calculated size were defined as clinically relevant. We then assessed whether passage of the ETT and removal of the SGA were possible with the clinically relevant combinations.
Data analysis and statistics
Results are summarized graphically and are shown in the figures. No statistical tests were necessary or applied. Power calculation was not necessary for this feasibility study.
Results
All possible combinations of the eight SGAs and six ETTs were tested. Results for the combinations recommended by the manufacturers are given in Fig. 2.
Passage of cuffed ETTs through the SGA
Intubation with the cuffed ETTs was possible with all combinations recommended by the manufacturers, except for the LMA Unique, whose manufacturer does not provide recommendations for endotracheal intubation. Nevertheless, passage of the ETTs was possible with this SGA with a wide range of combinations, similar to the other SGAs. The widest range of possible combinations was found with the Air-Q inflatable and the Air-Qsp, which can be used with a size 5.5 ETT in SGAs size 2.0 or larger. This was followed by Ambu AuraGain and Ambu Aura-i, which are also marketed for intubation. With these SGAs, passage of all sizes of tested ETTs was possible with a size 2.5 SGA. The smallest range of possible combinations was found for Ambu AuraStraight, with which only size 1.0 could be used in conjunction with an ETT size 3.0. For standard pediatric SGAs, Ambu AuraOnce and the LMA Unique provided a better range of possible combinations with an ETT (i.e., for SGA sizes 1.0 and 1.5, intubation with ETTs of sizes 3.5 and 4.0, respectively, were recommended).
There was no difference regarding the feasibility of passing an ETT for intubation through the SGA with the various cuffed ETTs. That is, passage of the ETT was possible with all recommended combinations of the four cuffed ETTs tested. The only exception was the LMA Unique, for which there are no manufacturer’s recommendations regarding intubation, and passage of the ETT through the SGA was possible with different ETT sizes depending on the type of ETT used (Fig. 2).
Supraglottic airway device removal after intubation with cuffed ETTS
In contrast to passage of the ETT through the SGA as performed during intubation, passage of the SGA over the ETT as performed during removal of the SGA after successful intubation was not feasible with all SGA-ETT combinations recommended by the manufacturers because the smaller ETTs had an outer diameter of the cuff’s pilot balloon that proved to be larger than the outer diameter of the actual ETT. Therefore, with some of the smaller ETTs the cuff’s pilot balloon became trapped in the airway lumen of the SGA, mostly at the level of the bite block. The only SGAs for which removal was possible with all recommended SGA sizes were Air-Q inflatable and Air-Qsp. In contrast, SGA removal was not possible with Ambu AuraGain, Ambu AuraOnce, or i-gel sizes 1.0 and 1.5, or with Ambu Aura-i, Ambu AuraStraight, or LMA Unique sizes 1.0, 1.5, and 2.0. Here, it was due to differences in the inner diameter of the SGAs, which was largest in Air-Q inflatable and Air-Qsp (Fig. 3). There were no differences with regard to feasibility of SGA removal with the various ETTS.
Passage of uncuffed ETTS through the SGA and removal of the SGA with uncuffed ETTS
Passage of the uncuffed ETTS was possible with all combinations recommended by the manufacturers (Fig. 2). Again, Air-Q inflatable and Air-Qsp offered the broadest range of possibilities. No recommendations regarding intubation are available for LMA Unique, although passage of the ETT was possible with the same combinations as with Ambu AuraGain and Ambu Aura-i (Fig. 2). For all SGAs where passage of the uncuffed ETT for intubation was possible, removal of the SGA was possible as well. For Air-Q and all Ambu SGAs, there were no differences regarding the two uncuffed ETTs. For the LMA Unique size 2.0, passage of the ETT was possible with a size 5.0 Sheridan but not with a size 5.0 Portex.
Comparison of the results with the manufacturers’ recommendations
The manufacturers’ booklets for AirQ inflatable, Air-Qsp, Ambu AuraGain, Ambu Aura-i, Ambu AuraOnce, Ambu AuraStraight, and i-gel included specific instructions regarding intubation with the SGA. The manufacturer’s LMA Unique booklet gives no information about intubation with the SGA. The existing recommendations are shown in Fig. 2 (black: not recommended; all others: recommended). None of the manufacturers specified whether the given recommendations regarding the sizing of the ETTs were for cuffed or uncuffed ETTs.
Recommendations by Ambu on how to perform intubation through the SGA differs among their various SGA models:
-
Ambu AuraGain recommendations are the most specific: Direct flexible scope-assisted tracheal intubation is recommended by railroading the ETT over a flexible fibrescope. Ambu specifies that the ETT should be fully deflated, implying the use of cuffed ETTs. They do, however, also indicate that “for specific combinations of AuraGain and ETT variants for pediatric patients, it is not possible to remove the AuraGain after the ETT is placed through the mask. They state that both cuffed and uncuffed ETTs are compatible with AuraGain but recommend using uncuffed ETTs in pediatrics if the SGA is to be removed after intubation.
-
Ambu Aura-i removal is possible, with no limitations regarding smaller sizes or cuffed ETTs. This contrasts with our study results, which showed that removal of Ambu Aura-i in sizes 1.0, 1.5, and 2.0 is not possible with cuffed ETTs.
-
For Ambu AuraOnce, the manufacturer recommends inserting an exchange catheter through the SGA with fibreoptic guidance, followed by removing the SGA and railroading the ETT over the exchange catheter.
-
For Ambu AuraStraight, direct intubation with a fully deflated ETT and FB guidance is recommended. It is also recommended that the SGA be left in place.
We noted that the manufacturers’ booklets for specific SGAs are not all the same in different languages, and it can be cumbersome to find the relevant information. For example, the German manufacturer’s booklet for Ambu AuraOnce does not indicate compatible ETT sizes, whereas the English version of the booklet does so. The manufacturer’s booklet of i-gel indicates compatible ETT sizes only. It does not indicate whether they are cuffed or uncuffed. Nor does it give further instructions on its use.
Thus, the manufacturer’s recommendations for Ambu Aura-i and i-gel are in conflict with our results: Its recommendations give a false impression that intubation and SGA removal are possible with all recommended sizes, whereas we found that this is not true for Ambu Aura-i sizes 1.0, 1.5, and 2.0 or i-gel sizes 1.0 and 1.5.
Clinically relevant combinations
Clinically relevant SGA-ETT combinations are shown in the Table. The study results are summarized for the clinically relevant SGA-ETT combinations in Fig. 4. Interestingly, several clinically relevant combinations showed limitations with regard to the possibility of passing the ETT or removing the SGA. The only exceptions were Air-Q inflatable and Air-Qsp, with which passage of the ETT and removal of the SGA were feasible with all clinically relevant combinations. All other SGAs displayed limitations, which even included SGA size 2.5 and uncuffed ETTs, indicating that size mismatches are clinically relevant and not limited to small children.
Overview of the possibility of passing cuffed and uncuffed ETTs through various SGAs and of subsequently removing the SGAs over the ETTs. Only the clinically appropriate SGA-ETT combinations are shown. Clinical appropriateness was determined by correlating the SGA size, corresponding weight and age, and corresponding ETT size, as shown in the Table
Discussion
This study assessed combinations of eight pediatric SGAs and six ETTS with regard to passing the ETT through the SGA and removing the SGA over the ETT as performed during intubation through an SGA and subsequent SGA removal. Passage of the ETT through the SGA was possible with many SGA-ETT combinations, but SGA removal proved impossible for many combinations with cuffed ETT because the ETT cuff’s pilot balloon was often larger than the inner diameter of the SGA. This problem was not addressed in many manufacturers’ booklets. We also found that intubation through an SGA or SGA removal is impossible with many clinically relevant SGA- ETT combinations.
Intubation through an SGA is an important technique for difficult airway management in children.17,18,19 Whereas it is usually a straightforward procedure in adults, important limitations are noted in children. For example, the relatively short length of the ETTs in relation to the pediatric SGA could result in the cuff lying at or above the level of the glottis or could lead to ETT dislocation during SGA removal.16,20 Another limitation of intubation through pediatric SGAs is the size mismatches of the inner SGA diameter and the ETT (we provide guidance on possible SGA-ETT combinations in the Table). These mismatches, which inhibit tracheal intubation and/or subsequent SGA removal, are not clearly documented in the manufacturers’ booklets. Thus, prior to anesthesia induction, each SGA-ETT combination must be assessed. Also, a reference table, such as the one in Fig. 2, can be used for guidance, which might be particularly useful for emergency airway management and failed intubation. We strongly recommend that each anesthesia department adapt Fig. 2 for their own purpose and check the compatibility of SGA and ETTs before use. For all combinations, generous lubrication is absolutely necessary.
Our study showed that, for some combinations, intubation was possible but SGA removal was not. The latter could be explained by the inner diameter of the SGA being too small to allow passage of the ETT cuff’s pilot balloon, which often became stuck at the level of the bite block. AirQ® and AirQ®sp had the largest inner diameters (Fig. 3). All other SGAs showed mismatches with the ETTs. This point is particularly important for Ambu® Aura-i, for which the user manual gives misleading information regarding possible combinations. Despite the fact that Ambu Aura-i is specifically designed for intubation, SGA removal was not possible with it in size 1.0, 1.5, or 2.0. In contrast, SGA removal was possible with Ambu AuraOnce size 2.0, which is not specifically marketed as an intubation aid. The problem of the cuff’s pilot balloon not fitting through Ambu Aura-i13 and the classic LMA15 has been mentioned previously but had not been systematically assessed.
For a difficult pediatric airway, the Association of Paediatric Anaesthetists guidelines recommend attempting fibreoptic intubation through an SGA and to leave the SGA in place.6 Deflation of the cuff could possibly avoid pressure necrosis, and the SGA might stabilize the ETT, thereby avoiding accidental extubation. In some cases, SGA removal is needed for longer-term ventilation or for surgical purposes. Even when the cuff’s pilot balloon fits through the SGA, accidental extubation could occur during SGA removal. In this context, a crucial point is the length of the ETT relative to the length of the SGA.20 Because larger (and longer) uncuffed ETTs fit through a specific SGA, the use of uncuffed ETTs for intubation through SGA has been proposed.16 It is known, however, that when using uncuffed ETTs (compared with cuffed ETTs) a higher proportion requires tube exchange.21 This situation is particularly cumbersome in children with a difficult airway. The use of cuffed ETTs in children has become standard and is currently preferred over the use of uncuffed ETTS for most children.21,22,23 The use of a Cook Airway Exchange Catheter (Cook Medical Inc, Bloomington, IN, USA) has been suggested to avoid accidental extubation when removing the SGA.17,19 This technique could also be used in cases in which the cuff’s pilot balloon does not fit through the SGA. In this case, after SGA insertion and intubation with an uncuffed or cuffed ETT, both ETT and SGA are removed over an airway exchange catheter over which a cuffed ETT is then placed. This technique, however, involves several airway manipulations that increase the risk of perforation with the airway exchange catheter.24 An SGA such as Air-Q - which does not require these maneuvers for intubation because its inner diameter is large enough to allow direct intubation with a cuffed ETT - might be advantageous. As an alternative in case of a mismatched SGA and ETT cuff’s pilot balloon, the balloon could be torn off for SGA removal. It has been proposed to then re-inflate the balloon and block the tube by means of an angiocatheter.13 Special repair kits for torn cuff pilot balloon lines exist, but they might be unavailable in an emergency situation. In addition, data on whether they provide a good, long-term seal are limited.
Because this study was performed in vitro, the usefulness of the various SGAs for intubation must be further evaluated in vivo. Each combination must be tested prior to use. Particularly, the question about the best way to remove an SGA after successful intubation remains unanswered. Direct SGA removal with the help of a stabilizer rod and SGA removal with an airway exchange catheter followed by reintubation over the same catheter are options. Furthermore, as already shown,16 the ETT must be long enough to protrude sufficiently from the SGA into the trachea, which depends on an SGA-ETT match and the airway anatomy.
Conclusions
We showed that passage of ETTs through pediatric supraglottic airways as performed during intubation was possible with all recommended SGA-ETT combinations. Removing the SGA, however, was not possible for the smaller SGA sizes when using cuffed ETTs. This limitation of endotracheal intubation via pediatric SGA is not clearly described in all manufacturers’ booklets, and anesthesiologists should be aware of this lack of information. Our study also showed that there are limitations regarding the passage of an ETT and removal of the SGA for clinically relevant SGA-ETT combinations for all SGAs up to size 2.5, except for Air-Q inflatable and Air-Qsp. We provide a reference table for use in clinical practice.
Notes
World Health Organization. Child Growth Standards. Available from URL: http://www.who.int/childgrowth/standards/weight_for_age/en/ (accessed September 2017) and World Health Organization. Growth Reference 5-19 Years. Available from URL: http://www.who.int/growthref/who2007_weight_for_age/en/ (accessed September 2017).
Resuscitation Council (UK). Paediatric Advanced Life Support. Available from URL: https://www.resus.org.uk/resuscitation-guidelines/paediatric-advanced-life-support/, EPALS manual, accessed 2017/03/12.
References
Hardman JG, Wills JS. The development of hypoxaemia during apnoea in children: a computational modelling investigation. Br J Anaesth 2006; 97: 564-70.
Weiss M, Engelhardt T. Cannot ventilate-paralyze! Paediatr Anaesth 2012; 22: 1147-9.
Apfelbaum JL, Hagberg CA, Caplan RA, et al. Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology 2013; 118: 251-70.
Henderson JJ, Popat MT, Latto IP. Pearce AC; Difficult Airway Society. Difficult Airway Society guidelines for management of the unanticipated difficult intubation. Anaesthesia 2004; 59: 675-94.
Morray JP, Geiduschek JM, Caplan RA, Posner KL, Gild WM, Cheney FW. A comparison of pediatric and adult anesthesia closed malpractice claims. Anesthesiology 1993; 78: 461-7.
Black A, Flynn P, Popat M, Smith H, Thomas M, Wilkinson K. Association of Paediatric Anaesthetists of Great Britain and Ireland Paediatric Difficult Airway Guidelines 2015. Available from URL: https://www.das.uk.com/files/APA2-UnantDiffTracInt-FINAL.pdf (accessed September 2017).
Barch B, Rastatter J, Jagannathan N. Difficult pediatric airway management using the intubating laryngeal airway. Int J Pediatr Otorhinolaryngol 2012; 76: 1579-82.
Jagannathan N, Wong DT. Successful tracheal intubation through an intubating laryngeal airway in pediatric patients with airway hemorrhage. J Emerg Med 2011; 41: 369-73.
Cain JM, Mason LJ, Martin RD. Airway management in two of newborns with Pierre Robin Sequence: the use of disposable vs multiple use LMA for fiberoptic intubation. Paediatr Anaesth 2006; 16: 1274-6.
Somri M, Barna Teszler C, Tome R, Kugelman A, Vaida S, Gaitini L. Flexible fiberoptic bronchoscopy through the laryngeal mask airway in a small, premature neonate. Am J Otolaryngol 2005; 26: 268-71.
Ellis DS, Potluri PK, O’Flaherty JE, Baum VC. Difficult airway management in the neonate: a simple method of intubating through a laryngeal mask airway. Paediatr Anaesth 1999; 9: 460-2.
Kim YL, Seo DM, Shim KS, et al. Successful tracheal intubation using fiberoptic bronchoscope via an I-gel™ supraglottic airway in a pediatric patient with Goldenhar syndrome - a case report. Korean J Anesthesiol 2013; 65: 61-5.
Jagannathan N, Sohn LE, Sawardekar A, et al. A randomized trial comparing the Ambu® Aura-i™ with the air-Q™ intubating laryngeal airway as conduits for tracheal intubation in children. Paediatr Anaesth 2012; 22: 1197-204.
Jagannathan N, Kozlowski RJ, Sohn LE, et al. A clinical evaluation of the intubating laryngeal airway as a conduit for tracheal intubation in children. Anesth Analg 2011; 112: 176-82.
Weiss M, Goldmann K. Caution when using cuffed tracheal tubes for fibreoptic intubation through paediatric-sized laryngeal mask airways. Acta Anaesthesiol Scand 2004; 48: 523.
Mauch J, Haas T, Weiss M. Distance from the laryngeal mask grip to endotracheal tube tip. A crucial point during fiberoptic intubation in children (German). Der. Anaesthesist 2012; 61: 123-8.
Weiss M, Engelhardt T. Proposal for the management of the unexpected difficult pediatric airway. Paediatr Anaesth 2010; 20: 454-64.
Johr M, Berger TM. Fiberoptic intubation through the laryngeal mask airway (LMA) as a standardized procedure. Paediatr Anaesth 2004; 14: 614.
Weiss M, Mauch J, Becke K, Schmidt J, Johr M. Fibre optic-assisted endotracheal intubation through the laryngeal mask in children (German). Anaesthesist 2009; 58: 716-21.
Schebesta K, Karanovic G, Krafft P, Rossler B, Kimberger O. Distance from the glottis to the grille: the LMA Unique, Air-Q and CobraPLA as intubation conduits: a randomised trial. Eur J Anaesthesiol 2014; 31: 159-65.
Weiss M, Dullenkopf A, Fischer JE, Keller C, Gerber AC, European Paediatric Endotracheal Intubation Study Group. Prospective randomized controlled multi-centre trial of cuffed or uncuffed endotracheal tubes in small children. Br J Anaesth 2009; 103: 867-73.
Litman RS, Maxwell LG. Cuffed versus uncuffed endotracheal tubes in pediatric anesthesia: the debate should finally end. Anesthesiology 2013; 118: 500-1.
Weiss M, Gerber AC. Safe use of cuffed tracheal tubes in children (German). Anasthesiol Intensivmed Notfallmed Schmerzther 2012; 47: 232-7.
de Almeida JP, Hajjar LA, Fukushima JT, Nakamura RE, Albertini R, Galas FR. Bronchial injury and pneumothorax after reintubation using an airway exchange catheter. Braz J Anesthesiol 2013; 63: 107-12.
Acknowledgements
The authors thank Christine Riggenbach, RN and Christian Rinderer, RN (both Department of Anaesthesiology and Pain Medicine, Inselspital, Bern University Hospital, Switzerland) for their help with the conduction of the study.
Conflicts of interest
None declared.
Editorial responsibility
This submission was handled by Dr. Philip M. Jones, Associate Editor, Canadian Journal of Anesthesia.
Author contributions
Maren Kleine-Brueggeney designed the study, conducted the study, analyzed the data, and wrote the manuscript. Manuel Kotarlic designed the study and helped conduct the study and write the manuscript. Lorenz Theiler designed the study, conducted the study, analyzed the data, and wrote the manuscript. Robert Greif designed the study and helped write the manuscript.
Funding sources
This work was funded by an institutional research grant of the Department of Anaesthesiology and Pain Medicine, Inselspital, Bern University Hospital, University of Bern, Switzerland.
Consultancies
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kleine-Brueggeney, M., Kotarlic, M., Theiler, L. et al. Limitations of pediatric supraglottic airway devices as conduits for intubation - an in vitro study. Can J Anesth/J Can Anesth 65, 14–22 (2018). https://doi.org/10.1007/s12630-017-0992-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-017-0992-z