Abstract
Background
Preoperative and postoperative anemia have been identified individually as potential risk factors for postoperative complications after coronary artery bypass grafting (CABG) surgery. Their interrelationship with acute kidney injury (AKI) and long-term mortality, however, has not been clearly defined and was the purpose of this study.
Methods
We retrospectively evaluated 6,130 adult patients undergoing CABG surgery performed at a single large academic medical center. Preoperative and postoperative hemoglobin concentrations were used as continuous predictors of postoperative AKI and mortality. Additionally, sex-specific preoperative (< 13 g·dL−1 in men and < 12 g·dL−1 in women) and postoperative anemia (the median of the lowest in-hospital values) were used as categorical predictors. AKI was defined according to the Kidney Disease: Improving Global Outcomes (KDIGO) Clinical Practice Guidelines, when serum creatinine rose ≥ 50% during the period between day of surgery and postoperative day ten, or when a 0.3 mg·dL−1 (26.5 μmol·L−1) increase was detected in a rolling 48-hr window from the day of surgery to the tenth postoperative day. The association of preoperative and postoperative hemoglobin levels and anemia patterns with postoperative AKI and mortality were assessed via univariable and multivariable Cox proportional hazard analyses with time-varying effects for postoperative serum hemoglobin concentrations.
Results
The median preoperative and median minimum postoperative serum hemoglobin concentrations were 13.1 g·dL−1 and 8.8 g·dL−1, respectively. The incidence of AKI was 58%. Overall, 1,880 (30.7%) patients died an average of 6.8 yr after surgery. After adjusting for differences in baseline and clinical characteristics, on any given day, patients with preoperative anemia (multivariable hazard ratio [HR], 1.23; 95% confidence interval [CI], 1.13 to 1.33; P < 0.001) and those with a combination of preoperative and postoperative anemia (multivariable HR, 1.24; 95% CI, 1.09 to 1.40; P < 0.0008) were at an elevated risk for developing postoperative AKI and mortality (preoperative anemia: multivariable HR, 1.29; 95% CI, 1.15 to 1.44; P < 0.001; preoperative and postoperative anemia: multivariable HR, 1.50; 95% CI, 1.25 to 1.79; P < 0.001).
Conclusions
Our findings suggest that preoperative anemia alone and preoperative anemia combined with postoperative anemia are associated with AKI and mortality after CABG surgery.
Résumé
Contexte
L’anémie préopératoire et l’anémie postopératoire ont toutes deux été identifiées en tant que facteurs de risque potentiels de complications postopératoires après une chirurgie de pontage aortocoronarien (PAC). Leurs liens réciproques avec l’insuffisance rénale aiguë (IRA) et la mortalité à long terme, toutefois, n’ont pas été clairement définies et constituent les objectifs principaux de cette étude.
Méthode
Nous avons évalué rétrospectivement 6130 patients adultes subissant une chirurgie de PAC dans un seul centre médical universitaire d’envergure. Les concentrations d’hémoglobine préopératoires et postopératoires ont été utilisées comme prédicteurs continus d’IRA et de mortalité postopératoires. En outre, l’anémie préopératoire spécifique selon le sexe (< 13 g·dL−1 chez les hommes et < 12 g·dL−1 chez les femmes) et l’anémie postopératoire (les médianes des valeurs hospitalières les plus basses) ont été utilisées comme prédicteurs catégoriques. L’IRA était définie selon les Directives de pratique cliniques KDIGO (Kidney Disease: Improving Global Outcomes), soit lorsque la créatinine sérique s’élevait de ≥50% pendant la période entre le jour de la chirurgie et le dixième jour postopératoire, ou lorsqu’une augmentation de 0,3 mg·dL−1 (26,5 μmol·L−1) était dépistée dans une fenêtre dynamique de 48 h entre le jour de la chirurgie et le dixième jour postopératoire. L’association des taux d’hémoglobine préopératoires et postopératoires et des profils d’anémie avec l’IRA et la mortalité postopératoires a été évaluée à l’aide d’analyses univariée et multivariée de régression à effet proportionnel de Cox avec des effets de variation en fonction du temps pour les concentrations postopératoires d’hémoglobine sérique.
Résultats
Les concentrations d’hémoglobine sérique préopératoires médianes et postopératoires médianes minimales étaient de 13,1 g·dL−1 et de 8,8 g·dL−1, respectivement. L’incidence d’IRA était de 58 %. Au total, 1880 (30,7 %) patients sont décédés en moyenne 6,8 ans après la chirurgie. Après ajustement pour tenir compte des différences de caractéristiques de base et cliniques, quel que soit le jour, les patients atteints d’anémie préopératoire (rapport de risque [RR] multivarié, 1,23; intervalle de confiance [IC] 95 %, 1,13 à 1,33; P < 0,001) et ceux présentant une anémie préopératoire et postopératoire (RR multivarié, 1,24; IC 95 %, 1,09 à 1,40; P < 0,0008) couraient un risque élevé de manifester une IRA et une mortalité postopératoires (anémie préopératoire : RR multivarié, 1,29; IC 95 %, 1,15 à 1,44; P < 0,001; anémie préopératoire et postopératoire : RR multivarié, 1,50; IC 95 %, 1,25 à 1,79; P < 0,001).
Conclusion
Nos résultats suggèrent que l’anémie préopératoire seule et l’anémie préopératoire combinée à l’anémie postopératoire sont associées à l’IRA et à la mortalité après une chirurgie de PAC.
Similar content being viewed by others
Acute kidney injury (AKI) after cardiac surgery remains a common, serious postoperative complication that affects 30-52% of these patients, with as many as 3% requiring renal replacement therapy.1,2 Postoperative AKI after cardiac surgery has been associated with a markedly reduced survival rate, increased utilization of health care resources, and increased likelihood for patients to be discharged to extended-care facilities.2,3,4 The pathophysiology of postoperative AKI is complex, involving many factors (e.g., advanced age, preexisting renal dysfunction, diabetes mellitus, ischemia-reperfusion injury, altered regional blood flow with vasomotor dysfunction, inflammatory responses, anemia, thrombocytopenia).1,5,6,7,8 Indeed, the interrelation among cellular inflammatory responses, anemia, and platelet activation/aggregation is now recognized as a hallmark feature of AKI.9,10,11 This is particularly relevant to anemic patients undergoing cardiac surgery with cardiopulmonary bypass (CPB), whereby low levels of circulating hemoglobin can promote hypoxic tissue injury characterized by medullary hypoxia, vasoconstriction, glomerular sequestration of activated platelets and inflammatory cells, and proximal tubular epithelial cell stress.12
Although most of these risk factors are not modifiable, there is a current focus on variables that could be optimized preoperatively to decrease the risk of postoperative AKI.13 Indeed, several studies investigated and confirmed the association between preoperative anemia and postoperative AKI and mortality after cardiac surgery.14,15 It has been shown that preoperative and intraoperative anemia are interrelated risk factors for postoperative AKI after cardiac surgery.16,17 Finally, sustained postoperative anemia for more than 50 days after coronary artery bypass grafting (CABG) surgery was found to be associated with an increased incidence of cardiovascular events and all-cause mortality.18 These studies,14,15,16,17,18 however, suffered from limitations such as inclusion of a relatively low risk cohort for postoperative AKI, methodological approaches,18 and inconsistent criteria used for defining postoperative AKI.13,15 Importantly, the incremental influence of the patient’s preoperative anemia status together with postoperative anemia on his or her risk of postoperative AKI and mortality have not been addressed.14,15,17,18 Therefore, the objective of our study was to determine whether preoperative and postoperative anemia are independently associated with postoperative AKI and mortality in patients undergoing CABG surgery.
Methods
Study population
The Institutional Review Board for Clinical Investigations at Duke University Medical Center (Durham, NC, USA) approved this study under 00065492-protocol number on August 31, 2016 and waived the requirement for patient consent.
We conducted this retrospective observational study on consecutive adult patients (> 18 yrs of age) who underwent isolated CABG surgery with CPB at Duke University Medical Center from January 1, 2001 to July 18, 2015. For patients who underwent more than one cardiac surgical procedure during that period, only data from the first operation were evaluated. Of the original 6,921 patients, 6,130 with complete data for preoperative and postoperative hemoglobin concentrations met the criteria for inclusion in the present study. Among these 6,130 patients analyzed and reported in this study, 4,217 had been analyzed and included in a report of a previous publication.1 The purpose of that previous study was to determine whether a decrease in platelet count after CABG surgery was independently associated with increased risk for postoperative AKI and mortality adjusted for a set of clinical predictors, including preoperative hemoglobin and postoperative minimum hemoglobin concentrations. The relations of preoperative and postoperative anemia with AKI and mortality were not studied.
Data collection
A standard set of perioperative data was collected from the Duke University Medical Center databases. They included the Duke Perioperative Electronic Database (Innovian® Anesthesia, Draeger Medical Inc., Telford, PA, USA); Cardiac Surgery Quality Assurance Database; Duke Databank for Cardiovascular Diseases; the Duke MAESTRO CARE (Medical Application Environments Supporting Transformation of Research and Operations: http://www.dukehealth.org/maestrocare), and Duke Health’s platform-based electronic health record (© 2016 Epic Systems Corporation, Verona, WI, USA; http://www.epic.com).
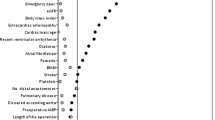
Clinical risk factors
The clinical risk factors for postoperative AKI and all-cause mortality included patient characteristics based on the definitions used by the European System for Cardiac Operative Risk Evaluation (EuroSCORE) scoring system,19 preoperative and intraoperative cardiovascular medication use, CPB and aortic cross-clamp times, intraoperative insertion of the intra-aortic balloon pump, intraoperative and postoperative blood transfusions within two days of surgery, and preoperative and postoperative serum creatinine values, hemoglobin concentrations, and platelet counts. During the study period, the decision for intraoperative and postoperative blood transfusion was guided by laboratory testing consistent with the recommendations of the American Society of Anesthesiologists “Practice Guidelines for Blood Component Therapy”, adopted in 199520 and updated in 200621 and 201522 as appropriate.
Serum creatinine was measured preoperatively and for the first ten days postoperatively per institutional protocol, as described previously.23 Preoperative serum creatinine values were defined by measures recorded before the index CABG procedure on the day that was closest to, but not on, the day of surgery.23
Per institutional protocol, serum hemoglobin concentrations were measured preoperatively and for the first ten days postoperatively or until discharge, whichever came first. We evaluated the effects of preoperative and postoperative minimum serum hemoglobin concentrations as continuous variables. A previous study indicated sex differences in tolerance to perioperative anemia.24 Thus, sex-specific preoperative anemia was defined using the World Health Organization definition of anemia as serum hemoglobin concentration < 13 g·dL−1 in men and < 12 g·dL−1 in women (http://www.who.int/vmnis/indicators/haemoglobin.pdf/; accessed October 2, 2016). The threshold for sex-specific postoperative anemia was defined using the median of the lowest (nadir) in-hospital values measured during the first ten postoperative days or until the day of hospital discharge. Subsequently, patients were categorized according to the presence of preoperative and postoperative anemia. We used the unrestricted postoperative nadir hemoglobin value because we were aiming to include the complete follow-up of all patients in order to define the sex-specific threshold for postoperative anemia. That single sex-specific anemia threshold value was then applied on a day-to-day basis in the modeling by comparing each day’s hemoglobin to the sex-specific threshold value we derived (see Statistics section for more details). It allowed us to use a single, consistent sex-specific threshold for defining anemia on each postoperative day, rather than a different threshold on each day.
Classification of outcomes
The primary outcome of interest was occurrence of AKI within the first ten postoperative days. Acute kidney injury was defined and categorized according to the Kidney Disease: Improving Global Outcomes (KDIGO) Clinical Practice Guidelines25 with modification due to the absence of urine output data. Postoperative AKI was ascertained when the serum creatinine level rose ≥ 50% between the day of surgery and postoperative day ten or when a 0.3 mg·dL−1 (26.5 μmol·L−1) increase was detected in a rolling 48-hr window from the day of surgery to the tenth postoperative day. We also stratified postoperative AKI as follows: stage I = risk: meets AKI criteria but not as pronounced as in stages II and III; stage II = injury: 2.0- to 2.9-fold rise in serum creatinine (i.e., 100-200% increase) within ten days; (3) stage III = failure: ≥ 3.0-fold rise in serum creatinine (i.e., ≥ 200% increase) within ten days, or ≥ 4 mg·dL−1 [353.6 μmol·L−1] increase in a rolling 48-hr window.1,25
The secondary outcome was long-term all-cause mortality. Survival information was obtained from the death registry in Epic©, which is part of the Duke University Health System’s electronic medical records-keeping system. Survival data for all patients who undergo cardiac surgery at Duke University Health System are regularly updated in the Epic© death registry, provided by return hospital encounters, the National Death Index (http://www.cdc.gov/nchs/ndi/index.htm),1,26 Duke Tumor Registry, Social Security Death Index, in-patient death, and vital status verified via direct patient contact through billing services. The Epic© death registry to verify vital status was interrogated as of June 30, 2016.
Statistical analysis
Continuous variables are presented as medians [interquartile range (IQR)] and categorical variables as group frequencies and percentages by the preoperative and postoperative anemia patterns. Kruskal-Wallis or Chi-square tests were used for descriptive comparisons, as appropriate.
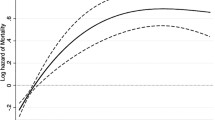
The association of preoperative and postoperative hemoglobin levels and anemia patterns with postoperative AKI defined as a binary outcome variable was assessed using univariable and multivariable Cox proportional hazard analyses with time-varying effects for postoperative serum hemoglobin concentration values. We used the Kaplan-Meier method to graphically evaluate and a test of time interaction effects to determine whether the hazard function for each variable met the proportional hazard and linearity assumptions of the Cox model. Given the day-to-day variations in postoperative serum hemoglobin concentrations in our study, we used extended Cox regression analysis with time-varying covariates and hazard ratios (HRs) to model the effects of day-to-day variations in postoperative hemoglobin concentrations on the risk for postoperative AKI.27–29 We defined the time-varying anemia pattern and hemoglobin variables in our proportional hazards models based on the most recent daily minimum hemoglobin concentration relative to the time being evaluated. Patients who died prior to experiencing AKI were included in the analysis, but their follow-up times were censored at the time of death. The resulting HR estimates for the effect of serum hemoglobin concentrations in these models should be interpreted as comparisons of the hazard for two patients with different serum hemoglobin concentrations on the same day after surgery.
In a subsequent analysis, we investigated the association between daily postoperative anemia patterns and serum hemoglobin concentrations and the severity of AKI using the Fine-Gray method of proportional hazard models for the subdistribution of stage I, II, and III AKI.30 With the Fine-Gray method, the subdistribution hazard for a given subevent is defined as the hazard for a patient who either suffers the sub-event or not, and expands the risk set at a given time to include both those who have experienced a different sub-event and those who are currently event-free. This analysis allowed us to estimate the effect of daily postoperative anemia patterns and serum hemoglobin on the absolute risk of AKI stage and to estimate the cumulative impact of daily postoperative anemia patterns and serum hemoglobin on patient AKI severity.31 As in the primary analysis, we used a time-varying effect for day-to-day variations in postoperative serum hemoglobin concentrations (both categorical and continuous).
Univariable and multivariable Cox proportional hazard regression models were next applied to evaluate the unadjusted and adjusted prognostic importance of preoperative and postoperative hemoglobin levels – categorized as preoperative, postoperative, and combined preoperative and postoperative anemia – and postoperative AKI with respect to event-free survival. Using the Kolmogorov-type supremum test and graphical evaluation of the hazard function over time, we evaluated the proportional hazard and linearity assumptions of the Cox model. We used time-varying covariates or spline functions to address violations as appropriate, the details of which are given in the Supplemental Methods (available as Electronic Supplementary Material). We again defined the time-varying anemia pattern and serum hemoglobin concentration variables in our proportional hazards models based on the most recent daily minimum serum hemoglobin concentrations relative to the time being evaluated. This step was taken to prevent the possibility of anemia pattern and/or serum hemoglobin concentration variables that occurred/were recorded after the onset of postoperative AKI being considered as predictors of postoperative AKI. For all time points after discharge or on postoperative day ten, whichever came first, the time-varying serum hemoglobin concentration model term was based on the last recorded daily minimum value. Additionally we evaluated postoperative AKI status as a time-varying covariate in the models. As inclusion of time-varying covariates precludes evaluation of the discriminatory ability and calibration of the final multivariable Cox regression model, we used the full set of clinical variables to adjust for all variables that could bias the estimate of the association between preoperative and postoperative anemia and mortality.
Interaction analyses were also performed to determine whether an association between an anemia pattern and perioperative packed red blood cell transfusion existed in relation to postoperative AKI and long-term mortality. Sensitivity analyses were also performed to determine whether exclusion of patients with preoperative elevated serum creatinine concentration > 2 mg·dL−1 affected the observed association among preoperative and postoperative anemia patterns and postoperative AKI, and long-term mortality. Hazard ratios and corresponding 95% confidence limits are reported. All analyses were performed using SAS Version 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
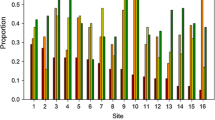
The overall median preoperative serum hemoglobin concentration was 13.1 [IQR, 11.7-14.3] g·dL−1, 13.6 [IQR, 12.4-14.7] g·dL−1 in men and 11.9 [IQR, 10.7-12.9] g·dL−1 in women. The overall median postoperative minimum serum hemoglobin concentration was 8.8 [IQR, 8.1-9.6] g·dL−1, and the sex-specific median of postoperative minimum serum hemoglobin concentration was 8.8 [IQR, 8.1-9.6] g·dL−1 in men and 8.6 [IQR, 8.0-9.5] g·dL−1 in women. Table 1 shows the demographic and clinical characteristics of the study cohort according to preoperative and postoperative anemia patterns. There were several notable differences between the groups, including age, sex, medical history, comorbidities, previous and intraoperative cardiovascular medication use, and intraoperative characteristics.
Postoperative acute kidney injury
Given the definition we used for AKI, which had to occur within ten days after surgery, ten patients who died within ten days before developing AKI were censored at the time of death but were included in the analysis for postoperative AKI. According to the KDIGO criteria,25 the overall incidence of postoperative AKI was 58% (n = 3,544), of which 89.7% (n = 3,179), 7.4% (n = 263), and 2.9% (n = 102) met the criteria for stages I, II, and III AKI, respectively. The incidence of AKI was 64% (764/1,197) in patients with preoperative anemia, 56% (894/1,595) in those with postoperative anemia, and 71% (895/1,253) in those with combined preoperative and postoperative anemia. In contrast, in patients without preoperative and postoperative anemia, the incidence was 48% (991/2,085). Several preoperative and intraoperative variables in the univariable analysis were significantly associated with an increased risk for postoperative AKI (Supplemental Table 1; available as Electronic Supplementary Material). When categorized based on the preoperative hemoglobin concentration and daily postoperative nadir hemoglobin concentration, preoperative anemia (univariable HR, 1.60; 95% CI, 1.49 to 1.72; P < 0.001) and the presence of preoperative and postoperative anemia (univariable HR, 1.64; 95% CI, 1.47 to 1.85; P < 0.001) were associated with postoperative AKI, whereas postoperative anemia alone (univariable HR, 1.06; 95% CI, 0.93 to 1.20; P = 0.39) was not. Furthermore, the preoperative hemoglobin concentration (univariable HR, 1.15; 95% CI, 1.13 to 1.17; P < 0.001) and the daily postoperative hemoglobin concentration (univariable HR, 1.03; 95% CI, 1.01 to 1.06; P = 0.02) – defined as continuous variables – also showed that for every 1 g·dL−1 decrease in hemoglobin concentration there was increased risk for postoperative AKI.
After adjusting for differences in baseline and clinical characteristics, on any given day patients with preoperative anemia and those with a combination of preoperative and postoperative anemia had an elevated hazard for developing postoperative AKI (Table 2). Multivariable analysis that incorporated preoperative serum hemoglobin levels and daily postoperative serum hemoglobin levels as continuous variables showed that, for every 1 g·dL−1 decrease in preoperative serum hemoglobin concentration, the risk for postoperative AKI increased by 11% (multivariable HR, 1.11; 95% CI, 1.08 to 1.13; P < 0.001). In contrast, for every 1 g·dL−1 decrease in postoperative serum hemoglobin concentration, the risk for postoperative AKI did not change significantly (multivariable HR, 0.98; 95% CI, 0.95 to 1.01; P = 0.15).
Finally, a series of subdistribution Cox proportional hazard models were analyzed to study the association of the anemia pattern with AKI severity. After adjusting for other clinical variables, patients with combined preoperative and postoperative anemia – defined as categorical predictors – were significantly more likely to progress to postoperative AKI stage I (multivariable HR, 1.15; 95% CI, 1.01 to 1.32; P = 0.04) and stage II (multivariable HR, 1.93; 95% CI, 1.28 to 2.90; P = 0.002), though had no increased risk of developing AKI stage III (multivariable HR, 1.70; 95% CI, 0.87 to 3.34; P = 0.12) (Table 3; see also the full multivariable results in Supplemental Table 2; available as Electronic Supplementary Material).
Long-term mortality
Patients were followed until June 30, 2016, with a median duration of follow-up of 6.8 [IQR, 3.3-10.8] yrs. During the full follow-up period, the incidence of overall, all-cause mortality was 30.7% (1,880/6,130), and the 30-day mortality was 1.5% (89/6,130).
The anemia patterns as univariable and multivariable predictors of long-term mortality are shown in Table 4 (full multivariable results are available in Supplemental Table 3; available as Electronic Supplementary Material). Again, many preoperative and intraoperative characteristics were associated with an increased risk for long-term mortality. The univariable analysis showed that preoperative anemia and a combination of preoperative and postoperative anemia, compared with no anemia, were associated with higher risk for long-term mortality, whereas postoperative anemia, compared with no anemia, conferred a lower risk for long-term mortality (Supplemental Table 3; available as Electronic Supplementary Material). After adjusting for differences in baseline and clinical characteristics, preoperative anemia (multivariable HR, 1.29; 95% CI, 1.15 to 1.44; P < 0.001) and a combination of preoperative and postoperative anemia (multivariable HR, 1.50; 95% CI, 1.25 to 1.79; P < 0.001), compared with no anemia, remained associated with increased risk for long-term mortality. Multivariable analysis that incorporated preoperative serum hemoglobin levels and postoperative nadir serum hemoglobin levels as continuous variables showed that lower preoperative serum hemoglobin levels were associated with a significantly increased risk for long-term mortality (multivariable HR, 1.14; 95% CI, 1.10 to 1.17; P < 0.001). In contrast, lower postoperative nadir serum hemoglobin levels were not significantly associated with a decreased risk for mortality (multivariable HR, 0.97; 95% CI, 0.94 to 1.01; P = 0.10).
Interaction and sensitivity analyses
We also investigated the relationship between intraoperative and postoperative packed red blood cell transfusion with preoperative and postoperative anemia patterns relative to postoperative AKI. Here, we found no evidence of a statistically significant effect between intraoperative and postoperative packed red blood cell transfusion and preoperative anemia (P = 0.27), postoperative anemia (P = 0.31), or preoperative and postoperative anemia (P = 0.82). These results indicated that there was no evidence of an interaction between intraoperative and postoperative packed red blood cell transfusions and the preoperative and postoperative anemia patterns for predicting postoperative AKI. Similarly, we found no evidence that there was an interaction between intraoperative and postoperative packed red blood cell transfusions and preoperative anemia (P = 0.358), postoperative anemia (P = 0.74), or preoperative and postoperative anemia (P = 0.16) for predicting long-term mortality. Finally, we explored the interactions between preoperative anemia (P = 0.99), postoperative anemia (P = 0.68), preoperative and postoperative anemia (P = 0.61), and postoperative AKI. We found no evidence of an interaction between postoperative AKI and anemia patterns regarding long-term mortality.
Among the 6,130 subjects studied, 0.15% (n = 369) had elevated preoperative serum creatinine concentrations (> 2 mg·dL−1). To determine whether the association between preoperative and postoperative anemia patterns and AKI persisted, we repeated the analysis excluding patients with an elevated preoperative serum creatinine concentration. We found that the association between preoperative anemia (multivariable HR, 1.23; 95% CI, 1.13 to 1.34; P < 0.001), a combination of preoperative and postoperative anemia (multivariable HR, 1.25; 95% CI, 1.09 to 1.43; P = 0.001), and postoperative AKI remained statistically significant. Similarly, the association between preoperative anemia (multivariable HR, 1.30; 95% CI, 1.16 to 1.46; P < 0.001), a combination of preoperative and postoperative anemia (multivariable HR, 1.44; 95% CI, 1.18 to 1.75; P < 0.001), and long-term mortality remained statistically significant. Interestingly, for the patients with elevated preoperative serum creatinine concentrations, there was no significant association between preoperative and postoperative anemia patterns or postoperative AKI and long-term mortality.
Discussion
In this retrospective study of consecutive patients who underwent CABG surgery with CPB, we demonstrated a relationship between preoperative and postoperative anemia patterns and AKI. Importantly, we found that preoperative anemia alone and preoperative with postoperative anemia had an incremental effect on AKI severity. We also observed that preoperative anemia and a combination of preoperative and postoperative anemia were associated with long-term mortality.
Mechanisms of AKI
The mechanisms of AKI in patients undergoing cardiac surgery involve many factors, including reduced renal perfusion pressure, pro-inflammatory mediators initiated by CPB, pigment nephrotoxicity due to hemolysis, preexisting contrast nephrotoxicity due to preoperative coronary angiography, and microembolism, each of which may contribute to nephron ischemia-reperfusion injury.32 This ischemia-reperfusion injury is more pronounced at the corticomedullary junction and in the medullary zone of the nephron, areas that are more vulnerable to ischemia because of their low partial pressure of oxygen and high metabolic demand.33
Acute kidney injury in the setting of cardiac surgery unfolds in four phases: initiation, extension, maintenance, recovery.34 All patients undergoing cardiac surgery with CPB develop some degree of ischemia-reperfusion injury to the kidneys that leads to the initiation phase of AKI. Preoperative anemia could contribute to progression to the extension phase of AKI, although this mechanism is poorly understood.35 Indeed, the relation between anemia and kidney injury is complex. For instance, patients with chronic kidney dysfunction develop multifactorial anemia resulting from iron-restricted erythropoiesis, reduced erythropoietin production by the kidneys, shortened red blood cell life-span, and increased blood loss.36 The consequent reduction in oxygen delivery to the kidneys exacerbates the ischemic and hypoxic injury to the metabolically active nephrons.37 In the context of cardiac surgery with CPB, anemia is likely to become more severe owing to hemodilution and blood loss, further compromising the nephrons. In a large-animal model, Patel et al.12 characterized this hypoxic injury as renal endothelial dysfunction, loss of nitric oxide bioavailability, vasoconstriction, medullary hypoxia, cortical adenosine triphosphate depletion, glomerular sequestration of activated platelets and inflammatory cells, and proximal tubule epithelial cell stress. Notably, patients with preoperative anemia who are undergoing cardiac surgery and those who develop postoperative anemia are more likely to receive red blood cell transfusion, which, in turn, has been associated with a higher risk for postoperative AKI.38 Our study also found an association between intraoperative and postoperative (within two days of surgery) red blood cell transfusion and the risk for postoperative AKI.
Preoperative anemia, AKI, and mortality
Our findings support the results of several previous studies that showed an association between preoperative anemia and postoperative AKI and mortality. In a study of 3,286 patients who underwent cardiac surgery, Karkouti et al.16 found that patients with preoperative anemia had a significantly higher incidence of postoperative AKI (10.6%) than non-anemic patients (3.6%). Likewise, the incidence of the composite outcome of stroke, postoperative AKI, and death was elevated in patients with preoperative anemia (15.8% vs 5.0%). Argalious et al.,39 who studied 10,648 consecutive patients undergoing cardiac surgery, also found that a lower preoperative hematocrit was associated with a significantly higher risk for postoperative AKI. De Santo et al.15 reported that, among 1,047 CABG surgery patients, those with preoperative anemia had a twofold increased risk for postoperative AKI compared with patients without preoperative anemia. Also, those who developed postoperative AKI had an almost 13-fold increased risk for hospital mortality than patients without postoperative AKI. Finally, in a series of 182,599 patients who underwent isolated CABG surgery with CPB, Williams et al. 40 found that those with a preoperative hematocrit < 42% had higher incidences of renal failure (7.8% vs 2.0%) and operative mortality (3.4% vs 1.1%) than patients whose preoperative hematocrit was > 42%.
Postoperative anemia, AKI, and mortality
Although the interrelations among preoperative anemia, AKI, and mortality with CABG surgery are well known, no study has yet investigated a potential association between postoperative anemia per se and AKI or mortality. The few studies that did explore an association between postoperative anemia and postoperative non-renal major vascular outcomes yielded conflicting findings. For example, Spiess et al.,41 who studied 2,417 patients undergoing CABG surgery with or without other concurrent cardiac procedures, observed that, compared with patients who had medium (25-33%) or low (≤ 24%) hematocrit values on admission to the intensive care unit, those with the highest hematocrit (Hct) (≥ 34%) had a significantly higher rates of myocardial infarction (highest Hct, 8.3%; medium Hct, 5.5%; low Hct, 3.6%) and mortality (highest Hct, 11.7%; medium Hct, 7.4%; low Hct, 5.7%). Given the retrospective design of that study, the investigators were unable to address mechanisms most likely to explain the association between low hematocrit values immediately after surgery and the lower myocardial infarction and mortality rates. Of note, the above findings were not influenced by transfusion. In contrast, Oliver et al. 42 conducted a study of 1,216 consecutive patients who underwent cardiac surgery and found that minimum postoperative serum hemoglobin concentrations in the first and second quartiles (hemoglobin levels < 8.10 and < 8.91, respectively) were linked to a higher risk for organ failure, extended intensive care unit stay, and mortality than those with hemoglobin concentrations in the two upper quartiles.
In the current study, we investigated preoperative and postoperative anemia in the context of a homogeneous cohort of patients undergoing CABG surgery only, focusing primarily on the potential effects of postoperative anemia on AKI and long-term mortality. Indeed, we demonstrated a significant relationship between the combination of preoperative and postoperative anemia and AKI and long-term mortality. However, there was a lack of significant association between postoperative anemia alone and AKI and long-term mortality. These latter observations may indicate that postoperative acute anemia without preexisting preoperative anemia is a less important risk factor for both AKI and long-term mortality. Most frequently, postoperative anemia is well tolerated, and patients generally recover from it without significant end-organ injury. In contrast, preexisting (preoperative) anemia is often a reflection of chronic disease that, when combined with other comorbid conditions (e.g., peripheral vascular disease, heart failure, diabetes mellitus), influences long-term mortality after CABG surgery.
Clinical implications
Our findings have important clinical implications because the preoperative period offers the opportunity to identify and effectively treat anemia, thereby possibly mitigating the risks of postoperative AKI and long-term mortality. Preoperative measures, including the use of intravenous iron and/or erythropoietin, may prove beneficial in reducing risks associated with preoperative anemia and the need for red blood cell transfusions. Nevertheless, there is little or no current evidence relative to cardiac surgery that this practice is beneficial.43 Future pragmatic trials are required to determine whether interventions that would minimize preoperative and postoperative anemia can ameliorate risks of AKI and/or mortality in the context of cardiac surgery. Opting for a minimally invasive approach to CABG surgery, improving oxygen delivery to the kidneys, minimizing the deleterious effects of CPB, and ascertaining the safe threshold for postoperative anemia could markedly reduce the possibility of fatal and non-fatal ischemic complications.44
Limitations
Our study has some limitations. First, the data on predictors of postoperative AKI and long-term mortality were not collected prospectively. Second, given the retrospective nature of our study, we were unable to determine causality, and we could determine only the associations between anemia, AKI, and survival following CABG surgery. Furthermore, a portion of the data reported in this study had been used for analysis in a previously published study from our group.1 Of note, however, no prior report by our group and/or by other independent groups investigated the interrelations of preoperative and postoperative anemia with AKI and mortality. Third, survival data in our study were obtained from the death registry in Epic©, which contains data from several sources. Consequently, there is a possibility that the mortality status for some of the studied patients may have been missed, although the incidence of long-term mortality reported in our study was similar to that reported by The Society of Thoracic Surgeons data registry.45 Fourth, the generalizability of our observations and findings to other centers could be limited because our study was performed in a single tertiary center. Nevertheless, the frequency of patients with preoperative anemia and postoperative anemia,14,15,16,17,18 postoperative AKI,46 and long-term mortality45 observed in our study were similar to those reported from large-scale retrospective studies. Fifth, most of the patients with preoperative and postoperative anemia received red blood cell transfusions. The fact that preoperative anemia, the combination of preoperative and postoperative anemia, and transfusion of blood products emerged as independent predictors of AKI and mortality suggests additive roles rather than confounding effects. Finally, our study included data from CABG surgery patients over a 14-yr period. Our analyses suggest that changes in patient management during that period resulted in improved overall survival. In contrast, however, a more recent year of surgery was not associated with a lower risk of postoperative AKI, which is consistent with published reports in cardiac surgery showing no improvements in postoperative renal outcomes over the past four decades. Despite adjustment for the year of surgery and other potential clinical- and procedure-related risk factors, the association between preoperative and postoperative anemia and AKI and mortality remained unchanged.
Conclusions
Our findings suggest that preoperative and postoperative anemia, and preoperative anemia combined with postoperative anemia, are interrelated risk factors for AKI following CABG surgery. We also observed that preoperative anemia and the combination of preoperative and postoperative anemia are associated significantly with long-term mortality. These findings suggest that strategies aimed at preventing anemia preoperatively as well as postoperatively may have an impact on reducing the risk of postoperative AKI and long-term mortality.
References
Kertai MD, Zhou S, Karhausen JA, et al. Platelet counts, acute kidney injury, and mortality after coronary artery bypass grafting surgery. Anesthesiology 2016; 124: 339-52.
Mangano CM, Diamondstone LS, Ramsay JG, Aggarwal A, Herskowitz A, Mangano DT. Renal dysfunction after myocardial revascularization: risk factors, adverse outcomes, and hospital resource utilization. The Multicenter Study of Perioperative Ischemia Research Group. Ann Intern Med 1998; 128: 194-203.
Loef BG, Epema AH, Smilde TD, et al. Immediate postoperative renal function deterioration in cardiac surgical patients predicts in-hospital mortality and long-term survival. J Am Soc Nephrol 2005; 16: 195-200.
Landoni G, Zangrillo A, Franco A, et al. Long-term outcome of patients who require renal replacement therapy after cardiac surgery. Eur J Anaesthesiol 2006; 23: 17-22.
Aronson S, Fontes ML, Miao Y. Mangano DT; Investigators of the Multicenter Study of Perioperative Ischemia Researc Group; Ischemia Research and Education Foundation. Risk index for perioperative renal dysfunction/failure: critical dependence on pulse pressure hypertension. Circulation 2007; 115: 733-42.
Bellomo R, Auriemma S, Fabbri A, et al. The pathophysiology of cardiac surgery-associated acute kidney injury (CSA-AKI). Int J Artif Organs 2008; 31: 166-78.
Lema G, Meneses G, Urzua J, et al. Effects of extracorporeal circulation on renal function in coronary surgical patients. Anesth Analg 1995; 81: 446-51.
Loutzenhiser R, Griffin K, Williamson G, Bidani A. Renal autoregulation: new perspectives regarding the protective and regulatory roles of the underlying mechanisms. Am J Physiol Regul Integr Comp Physiol 2006; 290: R1153-67.
Mathew JP, Rinder CS, Howe JG, et al. Platelet PIA2 polymorphism enhances risk of neurocognitive decline after cardiopulmonary bypass. Multicenter Study of Perioperative Ischemia (McSPI) Research Group. Ann Thorac Surg 2001; 71: 663-6.
Rinder CS, Fontes M, Mathew JP, Rinder HM, Smith BR; Multicenter Study of Perioperative Ischemia Research Group. Neutrophil CD11b upregulation during cardiopulmonary bypass is associated with postoperative renal injury. Ann Thorac Surg 2003; 75: 899-905.
Rinder CS, Mathew JP, Rinder HM, et al. Platelet PIA2 polymorphism and platelet activation are associated with increased troponin I release after cardiopulmonary bypass. Anesthesiology 2002; 97: 1118-22.
Patel NN, Lin H, Toth T, et al. Reversal of anemia with allogenic RBC transfusion prevents post-cardiopulmonary bypass acute kidney injury in swine. Am J Physiol Renal Physiol 2011; 301: F605-14.
Karkouti K, Wijeysundera DN, Yau TM, et al. Acute kidney injury after cardiac surgery: focus on modifiable risk factors. Circulation 2009; 119: 495-502.
Kulier A, Levin J, Moser R, et al. Impact of preoperative anemia on outcome in patients undergoing coronary artery bypass graft surgery. Circulation 2007; 116: 471-9.
De Santo L, Romano G, Della Corte A, et al. Preoperative anemia in patients undergoing coronary artery bypass grafting predicts acute kidney injury. J Thorac Cardiovasc Surg 2009; 138: 965-70.
Karkouti K, Wijeysundera DN, Beattie WS; Reducing Bleeding in Cardiac Surgery (RBC) Investigators. Risk associated with preoperative anemia in cardiac surgery: a multicenter cohort study. Circulation 2008; 117: 478-84.
Karkouti K, Grocott HP, Hall R, et al. Interrelationship of preoperative anemia, intraoperative anemia, and red blood cell transfusion as potentially modifiable risk factors for acute kidney injury in cardiac surgery: a historical multicentre cohort study. Can J Anesth 2015; 62: 377-84.
Westenbrink BD, Kleijn L, de Boer RA, et al. Sustained postoperative anaemia is associated with an impaired outcome after coronary artery bypass graft surgery: insights from the IMAGINE trial. Heart 2011; 97: 1590-6.
Roques F, Nashef SA, Michel P, et al. Risk factors and outcome in European cardiac surgery: analysis of the EuroSCORE multinational database of 19030 pateints. Eur J Cardiothorac Surg 1999; 15: 816–22; discussion 822–3
American Society of Anesthesiologists Task Force on Blood Component Therapy. Practice guidelines for blood component therapy: a report by the American Society of Anesthesiologists Task Force on Blood Component Therapy. Anesthesiology 1996; 84: 732-47.
American Society of Anesthesiologists Task Force on Perioperative Blood Transfusion and Adjuvant Therapies. Practice guidelines for perioperative blood transfusion and adjuvant therapies: an updated report by the American Society of Anesthesiologists Task Force on Perioperative Blood Transfusion and Adjuvant Therapies. Anesthesiology 2006; 105: 198-208.
American Society of Anesthesiologists Task Force on Perioperative Blood Management. Practice guidelines for perioperative blood management: an updated report by the American Society of Anesthesiologists Task Force on Perioperative Blood Management. Anesthesiology 2015; 122: 241–75.
Sickeler R, Phillips-Bute B, Kertai MD, et al. The risk of acute kidney injury with co-occurrence of anemia and hypotension during cardiopulmonary bypass relative to anemia alone. Ann Thorac Surg 2014; 97: 865-71.
Karkouti K, Wijeysundera DN, Yau TM, McCluskey SA, van Rensburg A, Beattie WS. The influence of baseline hemoglobin concentration on tolerance of anemia in cardiac surgery. Transfusion 2008; 48: 666-72.
Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group. KDIGO clinical practice guideline for acute kidney injury. Kidney Inter Suppl 2012; 2: 1-138.
Lobato RL, White WD, Mathew JP, et al. Thrombomodulin gene variants are associated with increased mortality after coronary artery bypass surgery in replicated analyses. Circulation 2011; 124(11 Suppl): S143-8.
Beyersmann J, Wolkewitz M, Schumacher M. The impact of time-dependent bias in proportional hazards modelling. Stat Med 2008; 27: 6439-54.
Klein JP, Moeschberger ML. Survival Analysis: Techniques for censored and truncated data. New York: Springer; 2003 .
Therneau TM, Grambsch PM. Modelling Survival Data: Extended the Cox Model. New York: Springer-Verlag; 2000 .
Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 1999; 94: 496-509.
Austin PC, Lee DS, Fine JP. Introduction to the analysis of survival data in the presence of competing risks. Circulation 2016; 133: 601-9.
Kumar AB, Suneja M. Cardiopulmonary bypass-associated acute kidney injury. Anesthesiology 2011; 114: 964-70.
Stafford-Smith M, Grocott HP. Renal medullary hypoxia during experimental cardiopulmonary bypass: a pilot study. Perfusion 2005; 20: 53-8.
Basile DP, Anderson MD, Sutton TA. Pathophysiology of acute kidney injury. Compr Physiol 2012; 2: 1303-53.
Ho J, Lucy M, Krokhin O, et al. Mass spectrometry-based proteomic analysis of urine in acute kidney injury following cardiopulmonary bypass: a nested case-control study. Am J Kidney Dis 2009; 53: 584-95.
Babitt JL, Lin HY. Mechanisms of anemia in CKD. J Am Soc Nephrol 2012; 23: 1631-4.
Brezis M, Rosen S. Hypoxia of the renal medulla–its implications for disease. N Engl J Med 1995; 332: 647-55.
Karkouti K, Wijeysundera DN, Yau TM, et al. Influence of erythrocyte transfusion on the risk of acute kidney injury after cardiac surgery differs in anemic and nonanemic patients. Anesthesiology 2011; 115: 523-30.
Argalious M, Xu M, Sun Z, Smedira N, Koch CG. Preoperative statin therapy is not associated with a reduced incidence of postoperative acute kidney injury after cardiac surgery. Anesth Analg 2010; 111: 324-30.
Williams ML, He X, Rankin JS, Slaughter MS, Gammie JS. Preoperative hematocrit is a powerful predictor of adverse outcomes in coronary artery bypass graft surgery: a report from the Society of Thoracic Surgeons Adult Cardiac Surgery Database. Ann Thorac Surg 2013; 96: 1628-34; discussion 1634.
Spiess BD, Ley C, Body SC, et al. Hematocrit value on intensive care unit entry influences the frequency of Q-wave myocardial infarction after coronary artery bypass grafting. The Institutions of the Multicenter Study of Perioperative Ischemia (McSPi) Research Group. J Thorac Cardiovasc Surg 1998; 116: 460-7.
Oliver E, Carrio ML, Rodriguez-Castro D, et al. Relationships among haemoglobin level, packed red cell transfusion and clinical outcomes in patients after cardiac surgery. Intensive Care Med 2009; 35: 1548-55.
Munoz M, Acheson AG, Auerbach M, et al. International consensus statement on the peri-operative management of anaemia and iron deficiency. Anaesthesia 2017; 72: 233-47.
Society of Thoracic Surgeons Blood Conservation Guideline Task Force; Ferraris VA, Brown JR, Despotis GJ, et al. 2011 update to the Society of Thoracic Surgeons and the Society of Cardiovascular Anesthesiologists Blood Conservation Clinical Practice Guidelines. Ann Thorac Surg 2011; 91: 944-82.
Shahian DM, O’Brien SM, Sheng S, et al. Predictors of long-term survival after coronary artery bypass grafting surgery: results from the Society of Thoracic Surgeons Adult Cardiac Surgery Database (the ASCERT study). Circulation 2012; 125: 1491-500.
Luo X, Jiang L, Du B, et al. A comparison of different diagnostic criteria of acute kidney injury in critically ill patients. Crit Care 2014; 18: R144.
Acknowledgements
The authors thank Betsy W. Hale, BSc, Alec Graham, BSc (Data Analysts, Department of Anesthesiology, Duke University Medical Center, Durham, NC, USA) and Jonathan Hong (undergraduate student, Duke University Medical Center, Durham, NC, USA) for their help with data retrieval and database building. We also thank Ishwori Dhakal, MSc (Statistician, Department of Anesthesiology, Duke University Medical Center, Durham, NC, USA) and Igor Akushevich, PhD (Senior Research Fellow, Population Research Institute at the Social Science Research Institute and Department of Anesthesiology, Duke University Medical Center, Durham, NC, USA), for their help with statistical analysis. Furthermore, we thank Kathy Gage (Research Development Associate, Department of Anesthesiology, Duke University Medical Center) for her editorial contributions to the manuscript. Finally, we sincerely thank the members of the Clinical Anesthesiology Research Endeavors (CARE) Group for facilitating the conduct of this study (see Electronic Supplementary Material for a listing).
Declaration of interest
None.
Editor responsibility
This submission was handled by Dr. Steven Backman, Associate Editor, Canadian Journal of Anesthesia.
Author contributions
Adriana D. Oprea, J. Mauricio Del Rio, Manuel L. Fontes, and Miklos D. Kertai contributed to conception and design, drafting the article or revising it critically for important intellectual content, interpretation of data, final approval of the version to be published. Mary Cooter and Cynthia L. Green contributed to study design and data analysis, and interpretation of data. Jörn A. Karhausen contributed to drafting the article or revising it critically for important intellectual content. Patrick Nailer contributed to conception and design, data collection, drafting the article or revising it critically for important intellectual content. Nicole R. Guinn, Mihai V. Podgoreanu, Mark Stafford-Smith, and Jacob N. Schroder contributed to drafting the article or revising it critically for important intellectual content.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Oprea, A.D., Del Rio, J.M., Cooter, M. et al. Pre- and postoperative anemia, acute kidney injury, and mortality after coronary artery bypass grafting surgery: a retrospective observational study. Can J Anesth/J Can Anesth 65, 46–59 (2018). https://doi.org/10.1007/s12630-017-0991-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-017-0991-0