Abstract
Background
Acute deterioration in respiratory status commonly occurs in patients who cannot be transported for imaging studies, particularly during surgical procedures and in critical care settings. Transthoracic lung ultrasonography has been developed to allow rapid diagnosis of respiratory conditions at the bedside. Nevertheless, the thorax is not always accessible, especially in the perioperative setting. Transesophageal lung ultrasonography (TELU) can be used to circumvent this problem.
Purpose
The aim of this narrative review is to provide a complete description of the TELU technique by summarizing the existing literature on the subject and describing our own experience that extrapolates from transthoracic lung ultrasonography.
Principal findings
The use of TELU can provide point-of-care real-time information for quickly establishing the etiology of acute hypoxemia. The transesophageal probe is placed in close proximity to the posterior regions of the lungs where lung consolidation and pleural effusions are most often seen; however, most of the artefacts relied on by transthoracic ultrasound have yet to be validated with TELU. Moreover, the relative invasiveness of TELU compared with transthoracic ultrasonography may limit its use to specific situations when the probe is already in place, as during cardiac anesthesia or when the anterior thorax is inaccessible. The main advantage of TELU may lie in the ability to integrate both cardiac and pulmonary assessments in one single examination.
Conclusion
Anesthesiologists and intensivists who already use transesophageal echocardiography on a regular basis should consider adding TELU to their clinical assessment of hypoxemia and related pulmonary pathologies. Nevertheless, the literature specifically supporting TELU is relatively limited, and further validation studies are needed.
Résumé
Contexte
Des détériorations aiguës de l’état respiratoire de patients qui ne peuvent être transportés pour des examens d’imagerie sont fréquentes, particulièrement lors d’interventions chirurgicales ainsi que dans le contexte des soins intensifs. L’échographie pulmonaire transthoracique a été mise au point afin de permettre de diagnostiquer rapidement la cause d’une détérioration respiratoire au chevet du patient. Or, le thorax n’est pas toujours accessible, particulièrement dans un contexte périopératoire. L’échographie transœsophagienne pulmonaire (ETOP) peut alors être utilisée pour pallier ce problème.
Objectif
L’objectif de ce compte rendu narratif est de proposer une description complète de la technique d’ETOP en résumant la littérature existante sur le sujet et en décrivant notre expérience, qui extrapole de la littérature portant sur l’échographie transthoracique.
Constatations principales
L’utilisation de l’ETOP permet d’obtenir des informations au chevet en temps réel afin d’établir rapidement l’étiologie de l’hypoxémie aiguë. La sonde transœsophagienne est située à proximité des régions postérieures des poumons, où les consolidations pulmonaires et les épanchements pleuraux sont les plus souvent observés. Toutefois, la plupart des artéfacts sur lesquels s’appuie l’échographie transthoracique doivent encore être validés pour l’ETOP. De plus, le côté relativement invasif de l’ETOP, comparativement à l’échographie transthoracique, pourrait limiter son utilisation à des situations particulières dans lesquelles la sonde est déjà en place, comme c’est le cas en anesthésie cardiaque ou lorsque le thorax antérieur est inaccessible. L’avantage principal de l’ETOP pourrait résider dans sa capacité à intégrer les évaluations cardiaques et pulmonaires en un seul examen.
Conclusion
Les anesthésiologistes et les intensivistes qui utilisent déjà l’échocardiographie transœsophagienne de façon régulière devraient envisager d’ajouter l’ETOP à leur évaluation clinique de l’hypoxémie et des pathologies pulmonaires associées. Toutefois, la littérature appuyant spécifiquement l’ETOP étant relativement limitée, davantage d’études de validation sont nécessaires.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Acute deterioration in respiratory status commonly occurs in patients who cannot be transported for imaging studies, particularly during surgical procedures and in critical care settings. Accordingly, bedside assessment using transthoracic lung ultrasonography was developed to allow for rapid diagnosis of respiratory conditions at the bedside, and there has been a growing interest in this new imaging technique.1 International consensus recommendations have been published to guide clinicians in the use of ultrasound (US) to evaluate the lung.2 Nevertheless, the thorax is not always directly accessible for conventional transthoracic ultrasonography, especially in the perioperative setting. To circumvent this problem, transesophageal windows can be used to image the lung in an analogous manner to direct transthoracic approaches. Few reports have been published addressing the specific aspects of transesophageal lung ultrasonography (TELU).3-15
The aim of this narrative review is to provide a comprehensive description of the TELU technique by summarizing the existing literature on the subject and describing our own experience that extrapolates from the transthoracic lung ultrasonography literature. In order to identify pertinent literature published on TELU, we searched PubMed, Google Scholar, and EMBASE™ to find relevant articles using multiple research strategies, including a combination of [“ultrasonography” or “transesophageal echocardiography”] and [“lung”, “lung diseases”, “pleural effusion”, “pneumonia”, “pneumothorax”, “consolidation”, or “atelectasis”] or specific lung ultrasonography terminology such as “B-lines”, “Lung Rockets”, “Lung Sliding”. We used Web of Science® for backward and forward citation tracking of selected articles.
Indications and contraindications
The main indication for TELU is the evaluation of acute hypoxemia in patients in settings where transthoracic ultrasonography or other bedside imaging techniques are either suboptimal or not available. Notably, it can be used in any setting where a transesophageal echocardiography (TEE) probe is already in place. These situations include the intraoperative setting or when patients present with conditions that might limit conventional transthoracic lung US imaging, including morbid obesity, significant subcutaneous emphysema, thoracic burns, or the presence of other thoracic wounds or dressings (Table 1). Transesophageal lung ultrasonography shares the same contraindications and complications of TEE that have already been extensively reported.16
Physics principles underlying lung US
Transthoracic lung ultrasonography relies not only on accurate images of true lung tissues but also on the careful interpretation of artefacts. These artefacts usually originate at the pleural interface and thus are more difficult to appreciate with TELU than with the transthoracic approach. Indeed, with the close proximity of the pleura to the esophagus, the probe provides a sectorial image with poor resolution in the near field where the pleural line is situated and where most artefacts are generated. Moreover, as we discuss later in this article, it is unlikely that the posteriorly generated artefacts of TELU can be used in the same way as the anterior artefacts of the traditional transthoracic US approach. As these artefacts can still be observed with TELU, we will briefly review them in this section, bearing in mind that their clinical utility has yet to be evaluated.
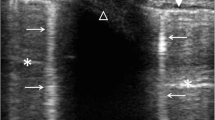
“Lung sliding” refers to the characteristic sliding motion of the visceral and parietal pleura against each other during movement of the lung with inflation and deflation.17 “Lung pulse” represents smaller faster rhythmic movements of the pleural interface synchronous with the patient’s electrocardiographic tracing induced by pulsatile blood flow through the pulmonary vessels.18 This is best appreciated during periods of apnea. Lung sliding and lung pulse of the left posterior lung can be observed most easily in a longitudinal plane of the descending aorta adjacent to the lateral aortic wall. “A-lines” are normal horizontal repetitions of the pleural line generated by reverberation19 (Fig. 1). Indeed, when the US beam reaches the pleural interface, it is completely reflected back towards the probe because of the strong acoustic impedance of the air contained in the lung. The probe captures most of the returning US, but part of it is also reflected back towards the probe-patient interface. This residual US beam is again reflected by the pleural interface, which generates another, albeit weaker, artefactual pleural line called “A-line”. As the time delay between US emission and reception is used to determine a structure’s depth, the distance between each reverberation line will be equal to the distance between the probe and the first pleural line.
In contrast, “B-lines”,19 also known as “comet tails” or “lung rockets”, appear as shiny vertical lines that arise from the pleural interface and move along with the parenchymal pleura throughout the respiratory cycle (Fig. 2). It is thought that they result from an increased lung density that in essence allows US to penetrate the visceral pleura. This may happen with decreased lung aeration (atelectasis) or increased interstitial fluid (pulmonary edema) or tissue (pulmonary fibrosis). In its most extreme form, the complete de-aeration of lung parenchyma allows imaging of true lung tissue, which sports a liver-like echotexture. Nevertheless, a focal area of increased lung density surrounded by residual air will allow the US beam to self-propagate and generate multiple successive reflections, resulting in hyperechoic laser-like vertical lines originating from the visceral pleura and extending all the way down the US field. The B-lines erase all other images in the US field and do not fade. Z-lines are also hyperechoic vertical lines, but they do not erase other artefacts and tend to fade gradually. Their origin is not completely understood. They are thought to be a normal finding and do not have any known clinical utility. With TELU, we look at the posterior lung zones where lung density is often increased as a result of decreased aeration in supine mechanically ventilated patients. Thus, B-lines should not be interpreted automatically as extravascular lung water (Table 2).
Ultrasonographic diagnosis of specific lung pathologies
Pleural effusions
Rapid diagnosis of pleural fluid collections (effusions) in the operating room (OR) and in the intensive care unit (ICU) can be life-saving, as in the case of massive hemothorax.10 Ultrasonography is a quick and sensitive tool to detect the presence of pleural fluid at the bedside, but it also allows for a thorough qualitative and semi-quantitative assessment. Effusions make surrounding structures, such as the ribs and the diaphragm, visible. Moreover, the passively de-aerated lung may be seen “moving freely” in the effusion, resulting in what is known as “lung flapping” or the “jellyfish sign” (Video 1, available as Electronic Supplementary Material).20 Pleural fluid should be carefully differentiated from ascites by locating the diaphragm, liver, and spleen and from pericardial effusion by locating the pericardium and descending aorta. The reported sensitivity of TELU for the detection of a pleural effusion is 97% and the specificity is 100% using computed tomography (CT) as a gold standard.7 The median volume at which an effusion becomes detectable is 125 mL on the left and 225 mL on the right.11 The aorta offers a convenient acoustic window that greatly facilitates the visualization of left-sided pathologies. Right-sided pathologies, on the other hand, are always more difficult to detect. This is due to the position of the esophagus which lies slightly on the left side of the vertebral column. This results in an acoustic shadow created by the vertebral bodies, thus preventing the US beam from reaching the more posterior portion of the right lung. In our experience, right-sided effusions as large as 300 mL have been completely missed.
Effusions should be qualitatively characterized as simple or complex.20 Simple effusions appear as anechoic and homogeneous free-flowing fluid (Fig. 3). Complex effusions are more heterogeneous and may exhibit various sonographic features such as septated loculations (Fig. 4), gelatinous and tissue-like echotexture, fibrin strands, and floating echogenic debris (called the “plankton sign”) (Video 2, available as Electronic Supplementary Material). Simple effusions can be transudates or exudates, but complex effusions should be considered exudates unless proven otherwise.21
The clinical context is often most helpful in determining the etiology of the effusion. It should also be pointed out that the appearance of a hemothorax is highly variable. Depending on the acuity of the hemothorax and whether there was a preexisting pleural effusion, it may display a gelatinous tissue-like echotexture (clot), a heterogeneous pattern with fibrin and debris, or even a relatively hypoechoic and homogeneous aspect (Fig. 5). Effusions with a tissue-like density may be difficult to differentiate from consolidated lung. Colour Doppler may then be of significant assistance by highlighting the blood vessels contained in a consolidated lung in contrast with a hemothorax where no blood vessels will be seen.
Finally, a semi-quantitative evaluation of the pleural effusion can be carried out as it can have important management implications. Many methods have been proposed for this purpose.4,7,11,13,14 The most practical approach, in our opinion, uses the maximal surface area of the effusion on a transverse plane (CSAmax). At an electronic multiplane angle of 0°, the effusion is scanned up and down in order to find its maximal surface area, which is usually located at a depth of about 30 cm from the incisors. The image is frozen and the surface area is measured by manually tracing its contour on screen (Fig. 6). This procedure, by itself, can provide an approximate estimate of the volume of the effusion (Table 3).
Cappers’s quantification method. At an electronic multiplane angle of 0°, the effusion is scanned up and down in order to find its maximal surface area, which is usually located at a depth of about 30 cm from the incisors. The image is frozen and the surface area is measured by manually tracing its contour on screen (CSAmax). The axial length (AL) is then measured by subtracting the depth of the probe at the proximal limit (Dproximal) of the effusion from the depth of the distal limit (Ddistal). The volume of the effusion is estimated by the product of CSAmax and AL.11
For a more precise estimation, the axial length (AL) of the effusion may be measured by subtracting the depth of the probe at the proximal limit (Dproximal) of the effusion from the depth of the distal limit (Ddistal).
The volume of the effusion (VE) is then estimated by multiplying CSAmax by the AL.11
For example, an effusion seen from a depth of 30-45 cm with a CSAmax of 35 cm2 would be estimated to contain 525 mL of fluid [i.e., (45-30) ⋅ 35].
Lung consolidation
Pneumonia, atelectasis, pulmonary contusion, neoplasm, and pulmonary infarction all result in a similar pattern of consolidation. The absence of alveolar air abolishes A-lines and B-lines and produces a tissue-like echotexture, sometimes called “hepatization” (Fig. 7). A sonographic air bronchogram may be seen as hyperechoic bubbles casting the bronchial tree (Fig. 8). When these bubbles move to and fro with respiration, the phenomenon is called a dynamic air bronchogram (Video 3, available as Electronic Supplementary Material). It is a demonstration of airway patency and thus rules out obstructive atelectasis. In a transthoracic echocardiographic study, this sign was shown to have a 94% specificity and a 97% positive predictive value for the diagnosis of pneumonia, defined as bronchoscopic confirmation of airway patency with positive bronchoalveolar lavage specimens.22 Although this study used a transthoracic approach, its findings likely also apply to TELU. Nevertheless, it may be difficult to distinguish pneumonia from atelectasis solely on the basis of ultrasonographic findings as the dynamic air bronchogram has poor sensitivity (61%). Compounding the issue is the frequent occurrence of some degree of atelectasis, which is an almost universal finding in patients receiving mechanical ventilation. Once again, the clinical context is the most useful element to establish a specific etiology.
Ultrasonography may help to diagnose some complications of pneumonia such as a parapneumonic effusion, empyema, and lung abscess. Transesophageal lung ultrasonography may also help to evaluate the extent of atelectasis. The surface area of consolidation in the left lung in the transverse plane as evaluated by TELU correlated well with the area measured by CT.5,6,8 This may help to optimize ventilation and oxygenation in patients with acute respiratory distress syndrome (ARDS) by quantifying lung recruitment with increasing positive end-expiratory pressure (PEEP) (Fig. 9) and/or prone positioning.
Alveolar-interstitial syndrome
The interstitial thickening produced by pulmonary edema or fibrosis results in the appearance of vertical B-lines described previously.23 (Fig. 2) In an acute setting, pulmonary edema is almost always responsible for the appearance of B-lines. This extravascular lung water (EVLW) may be the product of increased hydrostatic capillary pressure, as in left ventricular failure, or increased capillary permeability, as in ARDS.20 Cardiogenic edema usually results in a B-line distribution that is gravity dependent, bilateral, and homogeneous. A noteworthy exception is mitral regurgitation, which can be strikingly localized, as an eccentric regurgitation jet can cause selective congestion in the lung tissue corresponding to the single pulmonary vein receiving the regurgitant jet.9 On the other hand, ARDS is characterized by a patchy distribution of B-lines and areas of reduced or absent lung sliding.24 The number of B-lines seems to be proportional to the amount of EVLW. Indeed, in an animal model with acute lung injury induced by oleic acid, a strong correlation was found between the number of B-lines and the wet-to-dry ratio of the lung tissue.25 The B-lines respond very quickly to changes in EVLW and thus allow real-time follow-up of fluid or diuretic therapy.26 In our experience, left-sided B-lines are present on the pre-procedure TELU exam in a significant proportion of cardiac surgery cases. While others have also reported the presence of this artefact using TEE,15 the exact meaning of their presence remains unknown. We should be cautious before extrapolating the associations and scores described with transthoracic imaging to TELU.
While the transthoracic approach allows interrogation of a wide surface of the pleural interface, where B-lines originate, the transesophageal approach allows interrogation of only the pleura immediately apposed to the posterior mediastinum. As there is often a gravitational gradient in edema distribution, this could potentially render TELU oversensitive. Further clouding the issue, atelectasis, a common occurrence in the dependent lung zones of patients under general anesthesia, has also been associated with the presence of B-lines.
Pneumothorax
As air tends to accumulate in the non-dependent area of the thorax, which is inaccessible to TELU in patients in the supine position, it is highly unlikely that a transesophageal approach could be of any diagnostic value for non-tension pneumothorax. A speculative exception, however, might be in patients in the prone position. Nevertheless, the cardiac consequences of increased intrathoracic pressures, such as collapse of the right atrium27 or diastolic obstruction of the right ventricular outflow tract, may be observed. In transthoracic imaging, a pneumothorax is characterized by the absence of lung sliding, B-lines, and lung pulse. Their absence has a 100% positive predictive value.28 The identification of a net transition point between absent and present lung sliding, termed “lung point”, is pathognomonic with a positive predictive value of 100%.29 None of these signs have been validated with TELU, however, and future validation is unlikely.
Lung examination
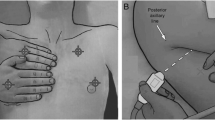
Any standard 2-8 MHz multiplane transesophageal probe can be used for TELU. Pending studies comparing various imaging settings, we recommend using a frequency of 4 MHz with no post-processing. Harmonic imaging, automatic tissue optimization, and any other form of post-processing should be turned off as they can suppress the artefacts that are relied on for image interpretation. The depth should be set at approximately 20 cm. We propose a systematic approach to the examination as has been similarly established for transthoracic lung US studies.2,30 We separate each lung along the craniocaudal axis into apical, middle, and basal regions. The origin of the left subclavian artery is used as a landmark to identify the apical regions. The superior pulmonary veins are used to mark the middle regions. Finally, the inferior vena cava right atrial junction is used to identify the basal regions. From each of these landmarks identified at 0° on the multiplane probe, a 90° electronic rotation of the transducer plane allows for scanning the lungs in a longitudinal axis. (Fig. 10A) From a cardiocentric starting position at 12:00, the TEE probe is rotated counter-clockwise to examine the left lung, with continued rotation to examine the right lung until a full rotation is completed. As anatomical lung segments cannot be readily identified, the position of the US beam is used to report our findings as accurately as possible. To indicate the position of the US beam, the position of the knob on the handle of the probe is used as the hand of a clock. The anterior region of the right lung is situated at 2:00, the lateral at 3:00, and the posterior at 4:00. Similarly, the anterior region of the left lung is at 10:00, the lateral at 9:00, and the posterior at 8:00 (Fig. 10B; Video 4, available as Electronic Supplementary Material).
TELU Examination technique. (A) Lung zones in the coronal plane. The origin of the left subclavian artery is used as a landmark to identify the apical regions. The superior pulmonary veins are used to mark the middle regions. The insertion of the inferior vena cava in the right atrium is used to identify the basal regions. (B) Lung zones in the transverse plane. The position of the knob on the handle of the probe is used as the hand of a clock in order to indicate the position of the ultrasound beam. The anterior region of the right lung is situated at 2:00, the lateral at 3:00 and the posterior at 4:00. Similarly, the anterior region of the left lung is at 10:00, the lateral at 9:00 and the posterior at 8:00. The 3D lung model was generated using a Vimedix Simulator (CAE Healthcare, Montreal, QC, Canada) with the permission of CAE Healthcare
Integrated cardiopulmonary approach to hypoxemia and other common problems in the OR or ICU
The majority of episodes of hypoxemia are of primary pulmonary etiology; however, the differential diagnosis also includes various cardiac pathologies. Cardiogenic pulmonary edema, secondary to left ventricular failure or valvulopathy, and intracardiac or intrapulmonary shunt may occur in some patients. Pulmonary embolism can also be associated with severe hypoxemia. Whether with a transthoracic or a transesophageal approach, the addition of information gathered by TELU to the elements provided by echocardiography allows a point-of-care integrated approach to the acutely hypoxemic patient (Table 4). The approach described in Table 4 reflects specific elements of the literature as well as the experience of the authors. The diagnostic accuracy, sensitivity, and specificity of TELUS remain to be formally validated.
Moreover, one can track the effect of specific ventilator strategies on lung aeration31 while also looking at the hemodynamic impact of this strategy, in real-time, at the bedside. Carefully integrating lung aeration data with right ventricular and left ventricular performance indicators may help find the “sweet spot” in terms of PEEP settings, especially in severe ARDS patients with cor pulmonale. While assessment of lung aeration has been validated using only a transthoracic approach, its principles should also apply to TELU, albeit limited to the posterior lung zones. Combined cardiopulmonary bedside ultrasonography performed during the weaning process may help differentiate between the multiple processes that hinder weaning patients from mechanical ventilation. Diaphragmatic dysfunction induced by mechanical ventilation or iatrogenic phrenic nerve injury is an underappreciated cause of weaning failure.32 Diminished or paradoxical diaphragmatic motion may be observed easily with transthoracic US but less so with TELU. Moreover, ultrasonography may allow clinicians to observe de-recruitment with the lung aeration score, which is derived from the presence of B-lines and atelectasis.33 A complete description of the lung aeration score is beyond the scope of this review as it was validated only with transthoracic imaging. We refer the interested reader to the excellent review by Bouhemad et al. 30 Cardiogenic pulmonary edema can also be responsible for unsuccessful weaning. During the transition from positive pressure ventilation to spontaneous unassisted breathing, left ventricular diastolic dysfunction may be unmasked by increased venous return,34 and systolic dysfunction may be unmasked by increased left ventricular afterload.35 Ultrasonography can detect deterioration in systolic and diastolic performance as well as the development of B-lines. These processes are often overlooked but easily treatable.
Finally, integrated cardiac and lung ultrasonography could allow for more optimal fluid therapy in hemodynamically unstable patients. The advent of dynamic indicators has brought great improvement in the ability to predict fluid responsiveness. Nevertheless, even the most advanced echocardiographic parameters, such as left ventricular outflow tract velocity time integral variation with respiration or with passive leg raise, are not perfect.36 Absence of B-lines in the anterior thoracic cavity evaluated with a transthoracic approach has been shown to be associated with a normal pulmonary artery occlusion pressure.19 In the context of fluid loading, a dynamic increase in the number of B-lines is thought to represent extravascular lung water and could be added as a safety measure to limit volume expansion before overt pulmonary edema becomes clinically apparent.37 This could be an interesting avenue and should be evaluated prospectively.
Advantages and limitations
The main advantages of TELU include the ability to perform the procedure at the bedside without the need to have access to the patient’s chest, and it may provide real-time feedback for interventions such as effusion drainage and fluid and ventilation management. The probe is closely apposed to the posterior regions of the lungs where pleural effusions, consolidations, and B-lines primarily occur. This approach allows access to the posterosuperior zones, considered the blind spots of transthoracic ultrasonography created by the scapulae.30 The main limitation of TELU is that it has not yet been sufficiently validated. It is more invasive than transthoracic ultrasonography and has significantly less supporting evidence. Transesophageal lung ultrasonography is also less sensitive to right-sided pathologies,11 and the anterior and lateral aspects of the lungs are largely inaccessible. Finally, TELU shares the main limitations of transthoracic US, as it often relies on artefact interpretation to gain insights into the lung and is clearly somewhat dependent on the operator.
Conclusion
Transesophageal lung ultrasonography can provide point-of-care real-time information about the presence of lung consolidation, pleural effusions, and pulmonary edema. Nevertheless, the major advantage of TELU lies in the ability to integrate both cardiac and pulmonary assessments in a single examination. Anesthesiologists and intensivists who already use TEE on a regular basis should definitively add this powerful tool to their clinical assessment. Though a large body of evidence now supports transthoracic lung ultrasonography, there are only few articles validating TELU. Besides pleural effusion and posterior consolidations, most of the approach presented in this article relies on extrapolation from the transthoracic literature and the authors’ experience. This calls not only for studies validating specific aspects of this diagnostic tool but also for broader studies evaluating the usefulness of adding a lung evaluation component to TEE in various settings.
References
Lichtenstein DA. Lung ultrasound in the critically ill. Ann Intensive Care 2014; 4: 1.
Volpicelli G, Elbarbary M, Blaivas M, et al. International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med 2012; 38: 577-91.
Orihashi K, Hong YW, Chung G, Sisto D, Goldiner PL, Oka Y. New applications of two-dimensional transesophageal echocardiography in cardiac surgery. J Cardiothorac Vasc Anesth 1991; 5: 33-9.
Swenson JD, Bull DA. Intraoperative diagnosis and treatment of pleural effusion based on transesophageal echocardiographic findings. Anesth Analg 1999; 89: 309-10.
Tsubo T, Sakai I, Suzuki A, Okawa H, Ishihara H, Matsuki A. Density detection in dependent left lung region using transesophageal echocardiography. Anesthesiology 2001; 94: 793-8.
Tsubo T, Yatsu Y, Suzuki A, et al. Daily changes of the area of density in the dependent lung region—evaluation using transesophageal echocardiography. Intensive Care Med 2001; 27: 1881-6.
Tsubo T, Yatsu Y, Okawa H, Ishihara H, Matsuki A. Transesophageal echocardiography is a sensitive method to evaluate pleural effusion. Anesthesiology 2002; 96: A322.
Tsubo T, Yatsu Y, Tanabe T, Okawa H, Ishihara H, Matsuki A. Evaluation of density area in dorsal lung region during prone position using transesophageal echocardiography. Crit Care Med 2004; 32: 83-7.
Verhaeghen D, Poelaert J, Ama R, Roosens C, Tempe DK, Chaney MA. Case 2-2005: evaluation of the lungs via transesophageal echocardiography. J Cardiothorac Vasc Anesth 2005; 19: 242-9.
Harasawa K, Maruyama T, Morimoto Y. Life-saving detection of right hemothorax by transesophageal echocardiography after femorofemoral bypass. J Cardiothorac Vasc Anesth 2006; 20: 229-31.
Capper SJ, Ross JJ, Sandstrom E, Braidley PC, Morgan-Hughes NJ. Transoesophageal echocardiography for the detection and quantification of pleural fluid in cardiac surgical patients. Br J Anaesth 2007; 98: 442-6.
Yatsu Y, Tsubo T, Ishihara H, Nakamura H, Hirota K. A new method to estimate regional pulmonary blood flow using transesophageal echocardiography. Anesth Analg 2008; 106: 530-4.
Howard A, Jackson A, Howard C, Spratt P. Estimating the volume of chronic pleural effusions using transesophageal echocardiography. J Cardiothorac Vasc Anesth 2011; 25: 229-32.
Ross JJ, Braidley PC, Morgan-Hughes NJ. TEE for estimating pleural effusion volumes. J Cardiothorac Vasc Anesth 2011; 25: e52.
Rehfeldt KH, Bruggink SM, Pulido JN. Transesophageal echocardiographic imaging of ultrasound lung rockets. Anesthesiology 2014; 121: 1335.
Hilberath JN, Oakes DA, Shernan SK, Bulwer BE, D’Ambra MN, Eltzschig HK. Safety of transesophageal echocardiography. J Am Soc Echocardiogr 2010; 23: 1115-27; quiz 1220-1.
Rantanen NW. Diseases of the thorax. Vet Clin North Am Equine Pract 1986; 2: 49-66.
Lichtenstein DA, Lascols N, Prin S, Meziere G. The, “lung pulse”: an early ultrasound sign of complete atelectasis. Intensive Care Med 2003; 29: 2187-92.
Lichtenstein DA, Meziere GA, Lagoueyte JF, Biderman P, Goldstein I, Gepner A. A-lines and B-lines: lung ultrasound as a bedside tool for predicting pulmonary artery occlusion pressure in the critically ill. Chest 2009; 136: 1014-20.
Lichtenstein DA. Lung Ultrasound in the Critically Ill: The BLUE Protocol. Switzerland: Springer International Publishing; 2015 .
Reuβ J. Sonographic imaging of the pleura: nearly 30 years experience. Eur J Ultrasound 1996; 3: 125-39.
Lichtenstein D, Meziere G, Seitz J. The dynamic air bronchogram. A lung ultrasound sign of alveolar consolidation ruling out atelectasis. Chest 2009; 135: 1421-5.
Lichtenstein D, Meziere G, Biderman P, Gepner A, Barre O. The comet-tail artifact. An ultrasound sign of alveolar-interstitial syndrome. Am J Respir Crit Care Med 1997; 156: 1640-6.
Copetti R, Soldati G, Copetti P. Chest sonography: a useful tool to differentiate acute cardiogenic pulmonary edema from acute respiratory distress syndrome. Cardiovasc Ultrasound 2008; 6: 16.
Jambrik Z, Gargani L, Adamicza A, et al. B-lines quantify the lung water content: a lung ultrasound versus lung gravimetry study in acute lung injury. Ultrasound Med Biol 2010; 36: 2004-10.
Shyamsundar M, Attwood B, Keating L, Walden AP. Clinical review: the role of ultrasound in estimating extra-vascular lung water. Crit Care 2013; 17: 237.
Denault A, Ferraro P, Couture P, et al. Transesophageal echocardiography monitoring in the intensive care department: the management of hemodynamic instability secondary to thoracic tamponade after single lung transplantation. J Am Society Echocardiogr 2003; 16: 688-92.
Lichtenstein D, Meziere G, Biderman P, Gepner A. The comet-tail artifact: an ultrasound sign ruling out pneumothorax. Intensive Care Med 1999; 25: 383-8.
Lichtenstein D, Meziere G, Biderman P, Gepner A. The, “lung point”: an ultrasound sign specific to pneumothorax. Intensive Care Med 2000; 26: 1434-40.
Bouhemad B, Mongodi S, Via G, Rouquette I. Ultrasound for “lung monitoring” of ventilated patients. Anesthesiology 2015; 122: 437-47.
Bouhemad B, Brisson H, Le-Guen M, Arbelot C, Lu Q, Rouby JJ. Bedside ultrasound assessment of positive end-expiratory pressure-induced lung recruitment. Am J Respir Crit Care Med 2011; 183: 341-7.
Kim WY, Suh HJ, Hong SB, Koh Y, Lim CM. Diaphragm dysfunction assessed by ultrasonography: influence on weaning from mechanical ventilation. Crit Care Med 2011; 39: 2627-30.
Soummer A, Perbet S, Brisson H, et al. Ultrasound assessment of lung aeration loss during a successful weaning trial predicts postextubation distress. Crit Care Med 2012; 40: 2064-72.
Moschietto S, Doyen D, Grech L, Dellamonica J, Hyvernat H, Bernardin G. Transthoracic echocardiography with Doppler tissue imaging predicts weaning failure from mechanical ventilation: evolution of the left ventricle relaxation rate during a spontaneous breathing trial is the key factor in weaning outcome. Crit Care 2012; 16: R81.
Lemaire F, Teboul JL, Cinotti L, et al. Acute left ventricular dysfunction during unsuccessful weaning from mechanical ventilation. Anesthesiology 1988; 69: 171-9.
Seneff MG, Zimmerman JE, Knaus WA, Wagner DP, Draper EA. Predicting the duration of mechanical ventilation. The importance of disease and patient characteristics. Chest 1996; 110: 469-79.
Caltabeloti F, Monsel A, Arbelot C, et al. Early fluid loading in acute respiratory distress syndrome with septic shock deteriorates lung aeration without impairing arterial oxygenation: a lung ultrasound observational study. Crit Care 2014; 18: R91.
Acknowledgements
We sincerely thank Denis Babin and CAE Healthcare for their help with the figures, and Antoinette Paolitto for her help with the submission process.
Funding
Support was provided solely from institutional and/or department sources. Dr. Denault is supported by the Montreal Heart Foundations and the Richard I. Kaufman Endowment Fund in Anesthesia and Critical Care.
Conflicts of interest
Dr. Denault and Dr. Desjardins are bedside ultrasound instructors for CAE Healthcare. Dr. Girard is a consultant for GE Healthcare.
Author contributions
Yiorgos Alexandros Cavayas contributed substantially to all aspects of this manuscript, including conception and design; acquisition, analysis, and interpretation of data, and drafting the article. Martin Girard and André Y. Denault contributed to all aspects of this manuscript, including conception and design; acquisition, analysis, and interpretation of data, and drafting the article. Georges Desjardins contributed to the conception and design of the manuscript.
Editorial responsibility
This submission was handled by Dr. Hilary P. Grocott, Editor-in-Chief, Canadian Journal of Anesthesia.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is accompanied by an editorial. Please see Can J Anesth 2016; 63: this issue.
Electronic supplementary material
Below is the link to the electronic supplementary material.
12630_2016_702_MOESM2_ESM.avi
Video 2. Plankton sign. Right-sided pleural effusion showing free-floating debris. Supplementary material 2 (AVI 2540 kb)
12630_2016_702_MOESM3_ESM.mp4
Video 3. Dynamic air bronchogram. Left-sided consolidation showing rhythmic movement of hyperechoic air bubbles in the bronchi. Supplementary material 3 (MP4 3424 kb)
12630_2016_702_MOESM4_ESM.wmv
Video 4. Examination technique: middle regions. The superior pulmonary veins are identified at 0° (transverse plane). From this position, we make a 90° electronic rotation of the plane in order to scan the lungs in a longitudinal axis. (Fig. 10A) We then rotate the probe counter-clockwise to examine the left lung and then continue to examine the right lung until a full rotation is completed. Supplementary material 4 (WMV 12178 kb)
Rights and permissions
About this article
Cite this article
Cavayas, Y.A., Girard, M., Desjardins, G. et al. Transesophageal lung ultrasonography: a novel technique for investigating hypoxemia. Can J Anesth/J Can Anesth 63, 1266–1276 (2016). https://doi.org/10.1007/s12630-016-0702-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-016-0702-2