Abstract
Background
We measured the angular change from the line of vision to the larynx around the upper incisors under defined laryngoscopic forces and investigated its association with the laryngoscopic view.
Methods
Laryngoscopy was performed under general anesthesia with muscle paralysis in male patients with a difficult laryngoscopy (DLG, n = 11) and in male patients matched for age and body mass index with an easy laryngoscopy (ELG, n = 11). A Macintosh blade #3 was used for the procedure. The line of vision was marked on lateral photographs during laryngoscopy by simultaneously delineating two straight lines: a line from the upper incisors to the lowest surface of the laryngoscope blade and a line from the upper incisors to the thyroid notch. The angle difference, defined as the angle between those two lines, was measured at laryngoscopic forces of 10-50 N.
Results
The angle difference was significantly greater in the DLG than in the ELG at 50 N [median, 18.0° (range, 16.5-21.0°) vs 12.0° (12.0-13.5°), respectively; P < 0.001] and at lower forces (10-40 N; P ≤ 0.001). A higher Cormack-Lehane grade was associated with a greater angle difference at 50 N (P < 0.001).
Conclusions
Compared with ELG, DLG is associated with a larger angle difference, i.e., a larger gap between the underside of the blade and the thyroid notch at all laryngoscopic forces (10-50 N). The concept of angle difference, based on the angular change in the line of vision around the upper incisors, may provide a new approach to understanding DLG. This study was registered with the Clinical Research Information Service, registration number KCT0000433.
Résumé
Contexte
Nous avons mesuré la modification de l’angle de la ligne de vision du larynx au niveau des incisives supérieures selon des forces laryngoscopiques déterminées et avons étudié son association avec la vue laryngoscopique.
Méthodes
Une laryngoscopie a été réalisée chez des patients de sexe masculin sous anesthésie générale et curarisation; les patients du groupe à laryngoscopie difficile (LGD, n = 11) ont été appariés pour l’âge et l’indice de masse corporelle avec des patients à laryngoscopie facile (LGF, n = 11). Une lame de Macintosh n° 3 a été utilisée pour la procédure. La ligne de vision a été marquée sur des photographies latérales prises au cours de la laryngoscopie en traçant simultanément deux lignes droites: une ligne partant des incisives supérieures vers la surface la plus basse de la lame du laryngoscope et une ligne partant des incisives supérieures vers l’encoche thyroïdienne. La différence d’angle, définie comme étant l’angle entre ces deux lignes, a été mesurée sous des forces laryngoscopiques de 10 à 50 N.
Résultats
La différence d’angle a été significativement plus grande dans le groupe LGD que dans le groupe LGF à 50 N [respectivement une médiane de 18,0° (amplitude: 16,5-21,0°) contre 12,0° (12,0-13,5°); P < 0,001] et avec des forces plus faibles (10 à 40 N; P < 0,001). Un grade Cormack-Lehane plus élevé a été associé à une plus grande différence d’angle à 50 N (P < 0,001).
Conclusions
Comparativement au groupe à laryngoscopie facile, la laryngoscopie difficile est associée à une plus grande différence d’angle, c’est-à-dire, un plus grand écart entre la face inférieure de la lame et l’encoche thyroïdienne, quelle que soit la force exercée sur le laryngoscope (10 à 50 N). Le concept de différence d’angle, reposant sur la variation d’angle de ligne de vision au niveau des incisives supérieures, pourrait fournir une nouvelle approche pour la compréhension des laryngoscopies difficiles. Cette étude a été enregistrée auprès du Service documentaire de recherche clinique – Numéro d’enregistrement: KCT0000433.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Direct laryngoscopy is performed in an attempt to visualize the larynx and thus facilitate tracheal intubation. The force applied to the laryngoscope blade should be sufficient to lift and move the structures located anteriorly, including the base of the tongue, the epiglottis, and the mandible, out of the operator’s view of the larynx.1 Although some debate exists regarding the optimal head and neck position for successful direct laryngoscopy,2-4 the laryngoscopic view ultimately depends on how effectively the laryngoscope blade displaces the anterior structures and adjusts the line of vision so as to bring the larynx into view. Despite the importance of the laryngoscope blade position in determining the laryngoscopic view, optimal placement has not been well described.
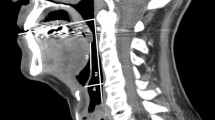
The view obtained with a curved laryngoscope differs from that of a straight-blade laryngoscope. The curved blade is characterized by its curved long axis and its flange,5 while a straight-blade laryngoscope provides a direct line of vision that is parallel to the long axis of the blade. With a curved blade, the operator’s vision is limited in the downward direction by the patient’s upper incisors and in the upward direction by the lowest point on the underside of the curved flange, while the reverse side of the flange comes in contact with the patient’s tongue.5 Consequently, a laryngeal view is possible only if the edge of the upper incisors, the underside of the curved flange, and the laryngeal inlet form a straight line (Fig. 1). An even better view is obtained if the line points more anteriorly in the laryngeal inlet. It follows that the laryngoscopist’s task is to reduce the angle between the line of vision and a hypothetical line joining the edge of the upper incisors to the thyroid notch, which is the superficial landmark outlining the most anterior portion of the larynx. This angle can be decreased by applying an upward force on the blade, thus lifting the anterior structures out of view. When using a defined force on the blade to obtain a laryngoscopic view in different patients, it is also hypothesized that a better view can be obtained in patients with a smaller difference in the angle between the line of vision and the line joining the upper incisors to the thyroid cartilage.
A lateral fluoroscopic view showing the operator’s best line of vision. When the laryngoscopist’s eyes move downward, the line of vision moves upward touching the lowest point on the underside of the curved flange, and laryngoscopic views gradually become better (large dotted line: Cormack-Lehane (CL) grade 3, small dotted line: CL grade 2). Ultimately, the best line of vision (closest to the larynx) would lie on a hypothetical line simultaneously touching the upper incisors and the low point of the flange (solid line: CL grade 1). I = upper incisors; T = thyroid notch. It follows that the best vision is associated with a small angle between the line of vision and the line joining the uppers incisors (I) and the thyroid notch (T)
To clarify the mechanism of difficult laryngoscopy, it is useful to introduce the concept of “angle difference”, which is the angle between the line of vision and the imaginary line joining the edge of the upper incisors and the thyroid notch as they intersect at the upper incisors (Fig. 1). The hypothesis is that this angle difference is greater in patients with a difficult laryngoscopy than in patients with an easy laryngoscopy when determined using a defined laryngoscopic force. The primary objective of this study was to compare the angle difference in patients with anticipated difficult tracheal intubation with the angle difference in subjects with no such difficulty when applying different defined laryngoscopic forces. A secondary objective was to correlate angle difference with laryngoscopic view.
Methods
A controlled non-randomized observational study was performed on 22 non-consecutive American Society of Anesthesiologists (ASA) class I-II male patients who underwent elective surgery under general anesthesia. Ethics approval was given by the Institutional Review Board of Seoul National University Bundang Hospital (protocol approval: October 2010), and written informed consent was obtained from each patient. The study was conducted from December 2010 to June 2011. Exclusion criteria were: 1) ASA class ≥ III, 2) history of cervical herniated intervertebral disc or cervical spine surgery, 3) dentures, 4) history of psychological disease or psychoactive drug use, and 5) craniofacial anomaly. We screened about 1,000 male patients who were scheduled for elective surgery under general anesthesia and ultimately identified 13 patients as potentially difficult laryngoscopies, as indicated by multiple positive predictors such as Mallampati class 3 or 4, thyromental distance ≤ 65 mm, or a small or receding mandible. These patients were classified in the difficult laryngoscopy group (DLG) if their Cormack-Lehane grade was 3 or 4. Otherwise, they were classified into the easy laryngoscopy group (ELG), defined as a Cormack-Lehane grade 1 or 2. The ELG group was comprised of patients without positive predictors matched by age and body mass index to the DLG patients.
Force measurement
To measure the axial force generated during laryngoscopy, we modified the laryngoscope (Welch Allyn, Skaneateles Falls, NY, USA) (Fig. 2) by designing a sheath to cover the entire laryngoscope handle. A transducer (Model 247ST; K-TOYO, Euijeongbu, Korea) that detects the stretching force was placed between the upper end of the handle and the sheath. During laryngoscopy, the axial force loaded on the handle was converted to electrical signals through the transducer. Signals were converted into measured force by a NI cDAQ-9172 data acquisition board (National Instrument, Austin, TX, USA), and values were displayed on a laptop computer. Data collection programs were designed using LabView 8.5 (National Instrument). The data acquisition rate was 10 Hz, and data analysis was performed with MATLAB® (MathWorks, Natick, MA, USA). The laryngoscope was calibrated before every experiment.
Diagram of the laryngoscope designed for this experiment. A sheath was designed to cover the entire laryngoscope handle. A transducer that detects the stretch force was placed between the upper end of the handle and the sheath. During laryngoscopy, the axial forces loaded on the handle were converted to electrical signals through the transducer
Induction of anesthesia
After premedication with midazolam 0.03 mg·kg−1 iv, general anesthesia was induced with intravenous administration of propofol and remifentanil via a target-controlled infusion system with target concentrations of 2-4 μg·mL−1 and 2-5 ng·mL−1, respectively. A neuromuscular blocking agent (rocuronium 0.6 mg·kg−1) was also given. Anesthesia was maintained with sevoflurane and positive-pressure mask ventilation. Oxygen saturation, an electrocardiogram, and noninvasive blood pressure were continuously monitored. Direct laryngoscopy was performed after loss of all four twitches with train-of-four ulnar nerve stimulation.
Experimental procedures and measurements
The study was performed on an operating table with the patient in the supine position. A hard pillow, 7 cm in height, was placed under the patient’s head to achieve the sniffing position during the procedure. The upper incisors were exposed with adhesive silk tape, and the thyroid notch was pointed to by an assistant with a pointer. A goniometer was attached tightly to the patient’s forehead to measure the angle of head extension, and this angle was monitored to maintain steady head extension during the laryngoscopy. After the tip of a curved laryngoscope blade (Macintosh #3, Welch Allyn, Skaneateles Falls, NY, USA) was positioned in the vallecula, the laryngoscope blade was checked and maintained at the same depth, although the blade angle and/or force applied were changed as outlined below. Throughout the laryngoscopic procedure, the operator tried not to touch the patient’s upper incisors and maintained the laryngoscope blade at 1-3 mm from the incisors, particularly while pictures were taken. For photography, a camera (5D Mark II; Canon, Tokyo, Japan) was placed with the lens at the level of the mandible and at a distance of one metre from the patient. Seven digital photographs of the lateral view of the head and neck of each patient were taken in the following conditions:
-
1.
Horizontal sniffing position: facial line was horizontal and head in the sniffing position;
-
2.
Extended sniffing: head was extended maximally in the sniffing position;
-
3.
10 N: laryngoscopic force reached 10 N;
-
4.
20 N: laryngoscopic force reached 20 N;
-
5.
30 N: laryngoscopic force reached 30 N;
-
6.
40 N: laryngoscopic force reached 40 N; and
-
7.
50 N: laryngoscopic force reached 50 N.
The operator’s right hand kept the patient’s head fully extended throughout the experiment, which was verified by maintaining the goniometer angle. The head extension angle was defined as the angle between the horizontal and the extended sniffing position. The operator performed laryngoscopy while an assistant monitored force on a laptop computer. As force was gradually increased, the assistant read the electrical output indicating the force at one to two times per second. When force reached the desired level (10-50 N), the operator maintained the force and the laryngoscopic view for three to six seconds while a straight pin was placed to join the upper incisors and the underside of the blade, and then pictures were taken. The laryngoscopic view at the maximal force (50 N) was recorded with the Cormack-Lehane grade defined as follows: 1: most of the glottis is seen; 2: only the posterior portion of the glottis is seen; 3: only the epiglottis, with no part of the glottis, is visible; and 4: not even the epiglottis is seen.5,6 In previous reports, the maximum laryngoscopic force required for the best laryngoscopic view ranged from 27.1-57.0 N.7-9 Although laryngoscopic forces > 50 N can be generated, the maximum force was limited to 50 N to decrease the risk of tissue trauma.
All measurements were completed within 90 sec and terminated before oxygen saturation decreased to 95%. Tracheal intubation was performed, and positive pressure ventilation was instituted immediately after step 7 above. An anesthesiologist who had completed more than 1,000 direct laryngoscopies over six years performed the laryngoscopies. Another anesthesiologist who was blinded to the purpose of this study printed the photographs to identify the anatomical landmarks for measuring angles and parameters associated with the line of vision.
Measurements of anatomical variables related to the angle difference
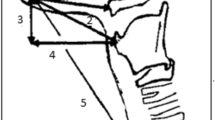
Figure 3 shows the lateral head and neck photographs during direct laryngoscopy. Anatomical landmarks (upper incisors, thyroid notch, and nasal root) were identified and marked on the photographs.
Definitions of the three lines (line to thyroid notch, line of vision, and facial line) and the three angles (thyroid notch angle, vision angle, and angle difference) on a lateral photograph during direct laryngoscopy. N = nasal root, I = upper incisor, T = thyroid notch. Line of vision: an extended line from a rigid straight pin simultaneously touching the upper incisors and the lower surface of the laryngoscopic blade; facial line: a line passing through the nasal root and the upper incisors; line to thyroid notch: a line from the upper incisors to the thyroid notch. Thyroid notch angle: the angle between the facial line and the line to the thyroid notch; vision angle: the angle between the facial line and the line of vision; angle difference: the angle between the line of vision and the line to the thyroid notch (angle difference = thyroid notch angle − vision angle). The laryngoscope blade is depicted as a dotted line. (Permission for publication of the photograph was obtained from the patient)
Three lines originating from the upper incisors were defined as follows:
-
Facial line: a line joining the nasal root and upper incisors;
-
Line to the thyroid notch: a line from the upper incisors to the thyroid notch;
-
Line of vision: a line extending along a rigid straight pin simultaneously touching the upper incisors and the lower surface of the laryngoscope blade.
Three angles were defined as follows:
-
Thyroid notch angle: the angle between the facial line and the line to thyroid notch;
-
Vision angle: the angle between the facial line and the line of vision;
-
Angle difference: the angle between the line of vision and the line to the thyroid notch (angle difference = thyroid notch angle − vision angle).
The facial line was used as an axis for angular measurements of the thyroid notch angle and the vision angle. The edge of the upper incisors was used as the centre of rotation to describe angular changes of the three lines.
Statistical analyses
The primary outcome was angle difference at a laryngoscopic force of 50 N. In a pilot study involving 12 subjects, the mean angle difference at a laryngoscopic force of 50 N was 11.3° with a standard deviation of 2.3°. A 20% change in the angle difference was considered clinically significant. Assuming α = 0.05 and β = 0.1, nine patients in each group were required to detect this difference. Considering a 10% drop-out rate, we calculated that at least ten patients were required for the study. Patients’ characteristics (age, height, weight, body mass index) and perioperative airway assessment (thyromental distance, Mallampati classification, and angle of head extension) were analyzed using the Mann-Whitney U test. The differences between the two groups regarding thyroid notch angle, vision angle, and angle difference were also analyzed using the Mann-Whitney U test. To investigate changes in the angles (thyroid notch angle, vision angle, and angle difference) with varying laryngoscope forces, the differences in the angles at each laryngoscopic force were assessed respectively by the Wilcoxon signed-rank test. The angle differences corresponding to Cormack-Lehane grades 1, 2, and 3 were investigated by the Kruskal-Wallis test. P values < 0.05 indicated statistical significance. Characteristics of preoperative airway assessment and angular variables are expressed as median and range. Statistical analyses were performed using SPSS® 18.0 (IBM SPSS, Somers, NY, USA).
Results
Among the 1,000 patients screened, 13 were expected to have a difficult laryngoscopy. Eleven of these patients turned out to have a Cormack-Lehane grade 3 or 4 view and were classified in the DLG, while the other two patients were classified in the ELG. Another nine patients completed the ELG. Demographic data and preoperative airway assessments of all patients are described in the Table. Age and body mass index were comparable between the two groups. Among the preoperative airway parameters, the thyromental distance was shorter in the DLG than in the ELG. In the ELG, five patients had a Cormack-Lehane grade 1 view and six patients had a grade 2 view. All patients in the DLG had a Cormack-Lehane grade 3 view at a laryngoscopic force of 50 N. In every patient, all measurements were completed within 90 sec. All patients underwent a safe tracheal intubation without any complications.
Angle difference
As the laryngoscopic force increased, the angle difference decreased gradually in both groups (Fig. 4). The angle difference was significantly greater in the DLG than in the ELG at 50 N (primary outcome measurement) [18.0° (16.5-21.0°) vs 12.0° (12.0-13.5°), respectively; P < 0.001] but also at all angles in the 10-50 N range (P < 0.001). At maximum laryngoscopic force, the laryngoscopic views were Cormack-Lehane grade 1 and 2 views in the ELG group and grade 3 views in the DLG group. The angle differences corresponding with the Cormack-Lehane grades 1, 2, and 3 views were 10.5-12.0°, 12.0-16.0°, and 16.0-22.0°, respectively (P < 0.001).
Thyroid notch angle, vision angle, and angle difference with defined laryngoscopic forces in the easy laryngoscopy group (ELG) and in the difficult laryngoscopy group (DLG). Angles are illustrated in Fig 2. Thyroid notch angle: the angle between the facial line and the line to the thyroid notch; Vision angle: the angle between the facial line and the line of vision; Angle difference = thyroid notch angle − vision angle, Hor = horizontal sniffing position; Ext = extended sniffing position. *P < 0.05 vs ELG; † P < 0.05 vs 10 N of laryngoscopic force; § P < 0.05 vs the change of vision angle from 10-50 N (ELG group only); ¥ P < 0.05 vs the change in the thyroid notch angle from extended sniffing to 50 N in easy laryngoscopy. Dots represent median, and error bars represent range
Thyroid notch angle
After neck extension, the thyroid notch angle was greater in the DLG than in the ELG. From neck extension to 50 N, the thyroid notch angle increased in the ELG, but not in the DLG (Fig. 4).
Vision angle
No significant difference in the vision angle was observed between the ELG and DLG (Fig. 4). Nevertheless, as laryngoscopic force increased from 10-50 N, the increase in the vision angle was significantly greater in the ELG than in the DLG [ELG: 10.0° (6.0-20.0°) vs DLG: 6.0° (4.5-8.5°); P = 0.02], indicating that the line of vision moved toward the larynx much more in the ELG than in the DLG at the same laryngoscopic force.
Discussion
This study shows that the thyroid notch angle in the extended sniffing position was greater and movement of the line of vision to the larynx was significantly smaller in the DLG than in the ELG during laryngoscopy. Consequently, the DLG angle difference, defined as the angle between the line of vision and a line from the upper incisors to the thyroid notch, was greater at all laryngoscopic forces (10-50 N). Consequently, the angle difference indirectly reflects how close the operator’s vision is to the larynx and determines the laryngoscopic view during direct laryngoscopy using a curved blade.
There are several possible reasons for the greater angle difference at 50 N in the DLG compared with the ELG. First, angle difference can be affected by laryngeal position, which is determined by the head and neck position, before laryngoscopy. In the present study, the DLG had a greater thyroid notch angle in the extended sniffing position when compared with the ELG before laryngoscopy, which means that the target is further away from the operator’s vision, and a greater laryngoscopic force may be required to reach the larynx and avoid failure. Second, a significantly smaller change in the vision angle at 10-50 N occurred in the DLG, suggesting limited movement of the laryngoscope blade compared with the ELG. Given that the movement of the laryngoscope blade is directly associated with the change in the line of vision, the limited movement of the blade would contribute considerably to the angle difference at the maximum laryngoscopic force in the DLG. Taken together, the present results show that both a line of vision at a distance from the larynx and limited movement of the laryngoscopic blade in the DLG patients could lead to more difficulty in pushing intraoral structures that obstruct the laryngeal view, and thus more force may be required during laryngoscopy in these patients.
Of significance, we showed that the angular change in the line of vision and its relationship with the larynx were closely associated with the laryngoscopic view. This novel study attempts to explain the mechanism of laryngoscopy in facilitating laryngeal exposure by investigating the angular change around the upper incisors under defined laryngoscopic forces. With increasing laryngoscopic force, angle difference decreases gradually in all patients (Figs. 1 and 4). Nevertheless, while this angle becomes small enough to visualize the laryngeal inlet (arytenoid cartilages) at less than 50 N in patients without a difficult laryngoscopy, the angle is still too wide to see any of the laryngeal structures in patients with a difficult laryngoscopy, even at 50 N. This means that the operator’s line of vision cannot reach the larynx in difficult laryngoscopy. Applying this principle, we can understand more easily how limited neck extension, a receding mandible, and a short thyromental distance can cause difficult laryngoscopy. In some situations, facilitated laryngoscopy can be explained by the modifications of the angle. One example is the BURP (backward, upward, and rightward pressure) maneuver,10 which moves the larynx backward, decreasing the angle difference and producing a better laryngoscopic view. Similarly, the McCoy laryngoscope moves the anterior larynx upward and decreases the angle difference, improving the laryngoscopic view in patients with difficult laryngoscopy.11,12 Another example is the “absence of upper incisors”,13 which facilitates a more downward movement of the proximal part of the blade, thereby bringing the line of vision closer to the larynx as the angle difference becomes smaller.
In the present study, the angle difference was significantly different between patients with easy laryngoscopy and those with difficult laryngoscopy, even at small laryngoscopic forces (10 N). Given that the known predictive factors of difficult laryngoscopy, such as a receding mandible, neck stiffness, or a high Mallampati classification, are perceptible without any force applied, we suggest that the angle difference at 10 N can be predictive of a difficult laryngoscopy at 50 N. In other words, measurement of angle difference may predict difficult laryngoscopy. The line of vision can be simulated by inserting a straight plate, e.g., a tongue depressor, into the oral cavity. Lifting the tongue to one side of the plate and pressing the opposite side with a small force on a pivot of the uppers incisor, we can measure angle difference – the angle between the plate and the line to the thyroid notch in the lateral view. The angle difference with the small force might help us predict difficult laryngoscopy. More investigation is needed to characterize and apply angle difference in clinical practice in order to predict difficult laryngoscopy and manage difficult intubation.
As is standard practice for direct laryngoscopy, the laryngoscopic force should be applied upward and forward along the axis of the laryngoscope handle after the tip of the laryngoscope blade is advanced into the vallecula and while the angle between the laryngoscope handle and facial line remains unchanged.5,8 Nevertheless, in practice, we observed that the angle tended to change while the blade turned toward the larynx, gradually revealing a better laryngoscopic view. This peculiar movement of the curved blade, followed by a vision change, is consistent with a previous result showing an increased laryngoscope angle between the axial line of the laryngoscope handle and the facial line in both easy and difficult laryngoscopies.1 Moreover, some patients undergoing a difficult laryngoscopy require significant force on the upper incisors, which are used as a fulcrum;14 this maneuver is not allowed during a standard laryngoscopy. Our results suggest an important change of view in clinical practice, namely, that rotation around the upper incisors is an effective movement of the curved blade for laryngeal exposure. In addition, the farther the blade is situated from the upper incisors, the worse the laryngoscopic view will be at the same laryngoscopic force.
Some limitations of the present study should be mentioned. First, the patient’s head was fully extended throughout the procedure in this study, which is contrary to conventional laryngoscopy allowing gradual head extension with increasing laryngoscopic force. Laryngoscopic view is influenced by head and neck position;2,3,5,15 therefore, positional changes in the head and neck due to the laryngoscopic force can affect the angular variables during laryngoscopy. We attempted to evaluate the unique effect of laryngoscopy on changes in the line of vision, larynx, and angle difference by preventing positional changes in the head and neck. Second, the laryngoscopist was not completely blinded to the study design; however, to reduce a potential bias, an assistant blinded to the study design monitored the laryngoscopic forces through a laptop computer, and we used a straight pin to assist in grading the laryngoscopic view in an effort to preclude the operator’s subjective decision. Third, the maximum laryngoscopic force was limited to 50 N. Although laryngoscopic forces > 50 N can be generated, they would increase the risk for tissue trauma and likely would not influence our results. In previous reports, the maximum laryngoscopic force required for the best laryngoscopic view ranged from 27.1-57.0 N.7-9
In conclusion, patients undergoing difficult laryngoscopy showed a significantly greater angle difference than patients who underwent easy laryngoscopy; therefore, the concept of using the change in the operator’s vision around the upper incisors could be regarded as a tool to understand and predict a difficult laryngoscopy.
References
Kitamura Y, Isono S, Suzuki N, Sato Y, Nishino T. Dynamic interaction of craniofacial structures during head positioning and direct laryngoscopy in anesthetized patients with and without difficult laryngoscopy. Anesthesiology 2007; 107: 875-83.
Adnet F, Baillard C, Borron SW, et al. Randomized study comparing the “sniffing position” with simple head extension for laryngoscopic view in elective surgery patients. Anesthesiology 2001; 95: 836-41.
Adnet F, Borron SW, Dumas JL, Apostolle F, Cupa M, Lapandry C. Study of the “sniffing position” by magnetic resonance imaging. Anesthesiology 2001; 94: 83-6.
Isono S. Common practice and concepts in anesthesia: time for reassessment: is the sniffing position a “gold standard” for laryngoscopy? Anesthesiology 2001; 95: 825-7.
Miller RD. Miller’s Anesthesia. 6th ed. Philadelphia, PA: Elsevier Churchill Livingstone Inc.; 2005 .
Cormack RS, Lehane J. Difficult tracheal intubation in obstetrics. Anaesthesia 1984; 39: 1105-11.
Hastings RH, Hon ED, Nghiem C, Wahrenbrock EA. Force, torque, and stress relaxation with direct laryngoscopy. Anesth Analg 1996; 82: 456-61.
Bucx MJ, Scheck PA, Van Geel RT, Den Ouden AH, Niesing R. Measurement of forces during laryngoscopy. Anaesthesia 1992; 47: 348-51.
Sudhir G, Wilkes AR, Clyburn P, Aguilera I, Hall JE. User satisfaction and forces generated during laryngoscopy using disposable Miller blades: a manikin study. Anaesthesia 2007; 62: 1056-60.
Knill RL. Difficult laryngoscopy made easy with a “BURP”. Can J Anaesth 1993; 40: 279-82.
Chisholm DG, Calder I. Experience with the McCoy laryngoscope in difficult laryngoscopy. Anaesthesia 1997; 52: 906-8.
Gabbott DA. Laryngoscopy using the McCoy laryngoscope after application of a cervical collar. Anaesthesia 1996; 51: 812-4.
Rocke DA, Murray WB, Rout CC, Gouws E. Relative risk analysis of factors associated with difficult intubation in obstetric anesthesia. Anesthesiology 1992; 77: 67-73.
Lee RA, van Zundert AA, Maassen RL, et al. Forces applied to the upper incisors during video-assisted intubation. Anesth Analg 2009; 108: 187-91.
Takenaka I, Aoyama K, Iwagaki T, Ishimura H, Kadoya T. The sniffing position provides greater occipito-atlanto-axial angulation than simple head extension: a radiological study. Can J Anesth 2007; 54: 129-33.
Funding
This study was supported by the Interdisciplinary Research Initiatives Program by the Colleges of Engineering and Medicine, Seoul National University (2011).
Conflicts of interest
None declared.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author contributions
Seongjoo Park, Jongryeol Jeong, Sukwon Cha, Sunghee Han, and Jinhee Kim helped design and conduct the study and reviewed the analysis of the data. Seongjoo Park, Sunghee Han, and Jinhee Kim helped analyze the data and write the manuscript. Seongjoo Park is the first author of this paper. Seongjoo Park is the author responsible for archiving the study files.
Rights and permissions
About this article
Cite this article
Park, S., Jeong, J., Cha, S. et al. Angular change in the line of vision to the larynx: implications for determining the laryngoscopic view. Can J Anesth/J Can Anesth 61, 433–440 (2014). https://doi.org/10.1007/s12630-014-0129-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-014-0129-6