Abstract
Purpose
The air-Q® intubating laryngeal airway (ILA) is a supraglottic device (SGD) designed specifically to function as both a primary airway and a bridging device and conduit for fibreoptic intubation in difficult airway scenarios. This observational study evaluated the usability and performance characteristics of pediatric air-Q ILA sizes 1.0, 1.5, 2.0, and 2.5 when used as a primary airway.
Methods
One hundred ten children, American Society of Anesthesiologists physical status I-III and undergoing elective surgery, received a weight-appropriate air-Q ILA following induction of anesthesia. The evaluation criteria included ease of insertion, quality of ventilation, presence of gastric insufflation, oropharyngeal leak pressures (OLPs) and maximum tidal volumes (VT max) in five different head positions, and fibreoptic view of the glottis.
Results
For sizes 1.0, 1.5, 2.0, and 2.5, the median [P25,P75] neutral OLPs (cm H2O) were 23.0 [20.0,30.0], 16.5 [15.0,20.8], 14.0 [10.0,17.8], and 14.0 [11.3,16.8], respectively. The median [P25,P75] neutral VT max values (mL·kg−1) were 17.4 [14.3,19.7], 20.3 [16.8,25.5], 17.8 [14.5,22.1], and 14.0 [11.6,16.0], respectively. Median [P25,P75] ease of insertion scores (0-10; 0 = easiest ever, 10 = most difficult ever) were 1 [1,2], 2 [2,3], 2 [1,2.8], and 2 [2,3] respectively. Ventilation was adequate in 108/110 cases, and a fibreoptic view of the vocal cords was obtained in 102/110 cases.
Conclusions
The air-Q ILA functions acceptably as a primary SGD in infants and children. The OLPs are lower than published values for the ProSeal laryngeal mask airway (LMA ProSeal™), the current pediatric SGD of choice, but adequate tidal volumes are readily achievable. The fibreoptic views of the glottis portend well for fibreoptic intubation through the device. (This trial was registered at clinicaltrials.gov number, NCT00885911).
Résumé
Objectif
Le masque laryngé d’intubation air-Q® est un dispositif supraglottique (DSG) conçu spécialement pour fonctionner aussi bien seul comme instrument de gestion des voies aériennes que comme pont et guide d’intubation fibroscopique en cas de voies aériennes difficiles. Cette étude observationnelle a évalué les caractéristiques de convivialité et de performance du masque laryngé air-Q de tailles 1,0, 1,5, 2,0 et 2,5 utilisé seul.
Méthode
Après l’induction de l’anesthésie, on a inséré un masque laryngé d’intubation air-Q adapté au poids chez 110 enfants de statut physique I-III selon la classification de l’American Society of Anesthesiologists devant subir une chirurgie non urgente. Les critères d’évaluation comprenaient la facilité d’insertion, la qualité de la ventilation, la présence d’insufflation gastrique, les pressions de fuite oropharyngée (OLP) et les volumes courants maximaux (VT max) dans cinq positions différentes de la tête, ainsi que la vue fibroscopique de la glotte.
Résultats
Pour les tailles 1,0, 1,5, 2,0, et 2,5, les OLP neutres médianes [P25,P75] (cm H2O) étaient de 23,0 [20,0,30,0], 16,5 [15,0,20,8], 14,0 [10,0,17,8], et 14,0 [11,3,16,8], respectivement. Les valeurs VT maximales neutres médianes [P25,P75] (mL·kg−1) étaient de 17,4 [14,3,19,7], 20,3 [16,8,25,7], 17,8 [14,5,22,1], et 14,0 [11,6,16,0], respectivement. Les scores médians [P25,P75] de facilité d’insertion (0-10; 0 = le plus facile, 10 = le plus difficile) étaient de 1 [1,2], 2 [2,3], 2 [1,2.8], et 2 [2,3] respectivement. La ventilation était adéquate dans 108/110 cas, et une vue fibroscopique des cordes vocales a été obtenue dans 102/110 cas.
Conclusion
Le fonctionnement du masque laryngé d’intubation air-Q est acceptable utilisé seul chez les nourrissons et les enfants. Les OLP sont plus basses que les valeurs publiées pour le masque laryngé ProSeal (LMA ProSeal™), le DSG actuellement privilégié en pédiatrie, mais on peut facilement atteindre des volumes courants adéquats. Les vues fibroscopiques de la glotte laissent présager une bonne intubation fibroscopique via le dispositif. (Cette étude a été enregistrée au numéro ClinicalTrials.gov NCT00885911).
Similar content being viewed by others
The laryngeal mask airway (LMA™) is a supraglottic device (SGD) that was introduced in 1986 and has revolutionized routine and difficult airway management in anesthesia and other critical care specialties. The LMA is now routinely employed as a device for maintaining airway patency during anesthesia. In addition, it has an established role as a rescue device in management of the difficult airway.1
As the advantages and versatility of the original LMA Classic™ became apparent, various modifications of its design evolved. The LMA ProSeal™ (PLMA) has improved pharyngeal seal, while the intubating LMA Fastrach™ offers one solution to securing the airway with an endotracheal tube via the LMA.
Supraglottic device options for pediatric patients undergoing anesthesia have been restricted by differences in size and three-dimensional pharyngeal anatomy. The LMA Classic is available in pediatric sizes, but the smaller sizes do not perform as well or as reliably as they do in adults. Pediatric-sized PLMAs are also available and provide superior performance with respect to sealing pressures when compared with the LMA Classic.2-4 The LMA Fastrach is a much bulkier device and is not available in pediatric sizes. Consequently, the SGD options for airway rescue in the difficult pediatric airway are limited. The evaluation of SGDs for this purpose in this population is a neglected research area, and the role of these devices in difficult pediatric airway management is based on published case reports or small case series.5,6
The air-Q® intubating laryngeal airway (ILA) (Cookgas LLC, St. Louis, MO, USA.) is a SGD specifically engineered for use as both a primary airway and a rescue or “Plan B” device in the event of a difficult airway.7,8 Its design allows insertion of a tracheal tube through its lumen, either blindly or mounted on a fibreoptic bronchoscope (FOB), to achieve tracheal intubation.
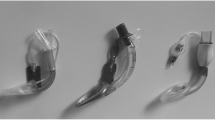
The air-Q ILA has a number of novel features that facilitate tracheal intubation (Fig. 1). The proximal 15-mm connector can be removed to reveal a larger opening for tracheal tube insertion. Also, the effective length of the shaft is shorter than the LMA, which is pertinent for ease of removal once the tracheal tube has been introduced. The air-Q ILA also has an elliptical cross-sectional profile to allow easier passage of the tracheal tube pilot balloon, and the shape and orientation of the distal outlet help to direct a FOB or an endotracheal tube reliably towards the glottis. The optional stylet facilitates retaining control of the tracheal tube during removal of the air-Q ILA, thus reducing the risk of dislodging the tracheal tube and losing the airway. The device also has a number of anatomical features that combine to improve the fit and seal of the mask once in situ. Reinforced bars across the dorsum of the mask prevent the tip from either downfolding or backfolding, and a tab is inserted into the pilot balloon valve so that the cuff of the mask can mould to the pharynx on insertion. Once the cuff is satisfactorily positioned, the tab is removed, sealing the cuff in its moulded shape. The cuff can then be inflated or deflated in a conventional manner according to the clinician’s preferences.
Air-Q® intubating laryngeal airway (ILA): (a) removable proximal 15-mm connector, (b) larger opening to allow passage of the endotracheal tube, (c) shorter effective length of the shaft for ease of air-Q ILA removal, (d) shape and orientation of the distal outlet directs a FOB or an endotracheal tube towards the glottis, (e) reinforced bars prevent the tip from downfolding or backfolding, (f) the tab inserted in the pilot balloon valve allows the mask cuff to mould to the pharynx; once the tab is removed, the cuff is sealed in its moulded shape
The objective of this study was to test the performance characteristics of the air-Q ILA as a primary airway in clinical pediatric anesthetic practice.
Methods
Recruitment for this observational study began after receiving approval from the University of British Columbia/Children’s and Women’s Health Centre of British Columbia Research Ethics Board (CW08-0170/H08-01196; approved November 2008). Written informed consent, and assent where appropriate, were obtained for children with American Society of Anesthesiologists physical status I-III, weighing up to 50 kg, and undergoing elective surgery appropriate for airway management with a SGD. Exclusion criteria included emergency surgery; weight less than the third percentile or greater than the 97th percentile for age; abnormal or contraindicated cervical spine flexion, extension, or rotation; or a contraindication to SGD placement. The subjects were stratified into four air-Q ILA groups based on the child’s weight: size 1.0, < 7 kg; size 1.5, 7-17 kg; size 2.0, 17-30 kg; and size 2.5, 30-50 kg, per manufacturer’s recommendation.
Enrolled subjects received anesthetic management from one of three consultant anesthesiologists. Anesthesia was induced with intravenous propofol 5 mg·kg−1 and remifentanil 2.5 μg·kg−1 or with 5-8% sevoflurane in O2/air, as determined by the anesthesiologist. Routine monitoring was applied. After induction, the anesthesiologist inserted the appropriate-sized air-Q ILA using the manufacturer’s described technique of midline non-rotational insertion. The cuff was inflated to an intracuff pressure of 60 cm H2O, as measured with a digital pressure cuff monitor. The abovementioned anesthesiologist, who was unblinded by definition, systematically evaluated the air-Q ILA as follows:
-
1.
The number of attempts at air-Q ILA placement was recorded. Failed insertion was defined as requiring more than two attempts.
-
2.
The anesthesiologist recorded ease of insertion as a subjective evaluation based on career experience using a numerical rating scale score from 0-10, with 0 being “the easiest possible insertion” and 10 being “the most difficult insertion ever”.
-
3.
The patient’s lungs were manually ventilated with the breathing circuit’s adjustable pressure limiting valve set at 20 cm H2O. Quality of ventilation was assessed and classified as excellent (chest rise with no audible leak), adequate (chest rise despite an audible leak), or poor (absent or inadequate chest rise with audible leak).
-
4.
With the adjustable pressure limiting valve still set at 20 cm H2O, the presence or absence of gastric insufflation was determined by epigastric auscultation during manual ventilation.
-
5.
Maximum tidal volume (VT max) was assessed using in-line spirometry from a Datex Ohmeda AS/3 patient monitoring system (GE Canada, Mississauga, ON, Canada) with the adjustable pressure limiting valve at 20 cm H2O and the patient’s lungs manually ventilated to an inspiratory pressure of 20 cm H2O. Maximum tidal volume is the largest of three consecutive exhaled measurements recorded and adjusted for subject weight (mL·kg−1).
-
6.
Oropharyngeal leak pressure was determined by setting the adjustable pressure-limiting valve set at 40 cm H2O and recording the pressure reading from the gauge in the anesthetic machine circuit where an oropharyngeal leak developed.
-
7.
The assessments of VT max and OLP were repeated with the patient’s head in five positions: neutral, maximum flexion, maximum extension, 90° left rotation, and 90° right rotation.
-
8.
With the patient’s head in the neutral position, flexible fibreoptic laryngoscopy was performed through the lumen of the air-Q ILA. The tip of the FOB was positioned at the distal outlet of the air-Q ILA, and the view of the larynx was scored as follows9: no vocal cords, vocal cords and anterior (downfolded, lingual surface) epiglottis, vocal cords and posterior (laryngeal surface) epiglottis, only vocal cords.
-
9.
Any necessary adjustments to the air-Q ILA, problems with ventilation, or adverse airway events were documented during the surgical procedure.
-
10.
After the end of anesthesia, the air-Q ILA was removed and scored dichotomously to examine for blood staining as an indicator of traumatic insertion.
Data were recorded in real time by an unblinded research assistant (E.C.).
No sample size calculation was performed. We planned to recruit 120 subjects, 30 in each air-Q ILA size category. Previously published studies of performance of new iterations of LMAs in adults and children have used similar group sizes.2-4
Data are described with median [P25,P75] for continuous data and frequency (percent) for discrete and categorical data. Due to its observational design, this study was not powered for comparisons, and as such, no inferential methods of statistical analysis were employed.
Results
One hundred ten patients were recruited (May 29, 2009 to February 24, 2012); none were excluded from data analysis. Demographic data are presented in Table 1. Three staff anesthesiologists independently performed 44 (40%), 36 (33%), and 30 (27%) air-Q ILA evaluations. There were no failed insertions. One hundred eight (98%) of the 110 air-Q ILAs were placed on the first attempt, and two (2%) were placed on the second attempt. The median [P25,P75] ease of insertion rating was 1 [1,2] for size 1.0; 2 [2,3] for sizes 1.5 and 2.5; and 2 [1,2.8] for size 2.0. One hundred eight (98%) subjects had acceptable (adequate or better) airway patency with the air-Q ILA (Table 2). Eleven (10%) subjects were determined to have gastric insufflation.
Oropharyngeal leak pressure and VT max data are shown in Table 3 and also in Figs 2 and 3. The median OLP appears to increase in flexion for all air-Q ILA sizes and decrease in extension for sizes 2.0 and 2.5 when compared with the neutral head position. Median VT max values do not appear to change with different head positions.
Median oropharyngeal leak pressure (OLP) values for the air-Q® intubating laryngeal airway (ILA) sizes 1.0 - 2.5 in five different head positions; Neutral (N), Flexion (F), Extension (E), Left rotation (L), and Right rotation (R). Individual data points are displayed, and each box plot represents the median and interquartile range
Median maximum tidal volume (VT max) values for the air-Q® intubating laryngeal airway (ILA) sizes 1.0 - 2.5 in five different head positions; Neutral (N), Flexion (F), Extension (E), Left rotation (L), and Right rotation (R). Individual data points are displayed, and each box plot represents the median and interquartile range
Data on FOB view are reported in Table 4. One hundred two (93%) subjects had visible vocal cords. A very low proportion of subjects with air-Q ILA sizes 2.0 and 2.5 had no visible vocal cords, whereas a higher proportion of subjects with sizes 1.0 and 1.5 had no vocal cords visible. A higher proportion of subjects with air-Q ILA sizes 1.5, 2.0, and 2.5 had only their vocal cords visible compared with subjects with size 1.0.
Six air-Q ILAs were removed before the end of the procedure. One was removed due to gastric insufflation, and three were removed due to low seal pressures (including both of those categorized as having poor quality of ventilation); these four air-Q ILAs were replaced with PLMAs. One air-Q ILA was replaced with an endotracheal tube for an undocumented reason; neutral OLP and VT max for this device were 15.0 cm H2O and 16.6 mL·kg−1, respectively. No vocal cords were visible via FOB in this patient. One patient desaturated shortly after study completion, and the air-Q ILA was replaced with an endotracheal tube. This patient was undergoing a magnetic resonance imaging for investigation of an axillary vascular malformation and was subsequently found to have a right to left shunt which accounted for the low saturation.
Blood was present on five (5%) air-Q ILAs after removal.
Discussion
The current SGD of choice in pediatric anesthetic practice is arguably the PLMA by virtue of its superior oropharyngeal seal compared with the LMA Classic. Therefore, when evaluating any new device that might contend for use as a primary airway, it must perform comparably or better than the PLMA.
The air-Q ILA devices were all successfully placed, and almost all were positioned on the first attempt, with a 97% (29/30) first attempt success rate for sizes 1.5 and 2.0 and a 100% (20/20 and 30/30) first attempt success rate for sizes 1.0 and 2.5. This is consistent with a previous report of the air-Q ILA in children10,11 and higher than the 88% reported with the air-Q ILA in adults.12 The first attempt success rate is also similar to the 92-100% reported for PLMA sizes 1.5-2.5.2-4,13,14 The air-Q ILA appears to be at least as easy to insert on the first attempt as the PLMA. As high first attempt success rate is predictive of easy insertion, it is unsurprising that we found the air-Q ILA subjectively easy to insert, with median ease of insertion scores of 1 and 2.
Quality of ventilation immediately after device insertion is an important variable, not only when considering its use as a primary airway but also if it is to be a viable choice as a bridging device in difficult airway scenarios. In this respect, the air-Q ILA performed satisfactorily, being excellent or adequate in 98% of subjects. The air-Q ILA sizes 1.5 through 2.5 perform similarly to the PLMA with comparatively equal proportions of subjects with excellent, adequate, and poor ventilation.2-4 A higher proportion of subjects had excellent ventilation with the size 1 PLMA than with the size 1.0 air-Q ILA.14
We elected to use manual ventilation to produce a more realistic simulation of clinical practice. Most anesthesiologists would check adequacy of SGD position and satisfactory tidal volume with manual intermittent positive-pressure ventilation before switching to the ventilator. Using manual bag compression in a circle system with the adjustable pressure limiting valve at 20 cm H2O, we delivered a VT max that comfortably exceeded clinical goals of 7-8 mL·kg−1, indicating that an adequate seal would be achieved in the majority of healthy children with normal lung compliance. Our data on neutral OLP values and, commensurately, our VT max values for the air-Q ILA are lower than existing published data for the PLMA.2-4,14 Our findings for air-Q ILA sizes 1.5 and 2.0 are similar to those previously published,10,11 where the mean (standard deviation [SD]) OLP was 17.5 (6.4) cm H2O and 18.5 (1.6) cm H2O for size 1.5 and 15.7 (4.3) cm H2O for size 2.0. Our OLP findings for size 1 were higher than those by Sinha et al. 11 who reported a mean (SD) OLP of 18.5 (2.1) cm H2O. Oropharyngeal leak pressures increase when the patient’s neck is in the flexed position, a phenomenon also described with the PLMA. Oropharyngeal leak pressures decrease in extension for air-Q ILA sizes 2.0 and 2.5; however, VT max is well above an acceptable level.
The FOB view through the air-Q ILA was excellent in the majority of patients; 102 (93%) subjects had visible vocal cords, with 45 (41%) having only their vocal cords visible from the distal outlet of the air-Q ILA. This is a higher percentage than that reported by Sinha et al. 11 and Jagannathan et al., 10 where only 70% and 73%, respectively, had any vocal cords visible. The percentage of subjects with only their vocal cords visible was similar to that of Sinha et al. 11 (45%) but higher than that of Jagannathan et al., 10 with 31% having only their vocal cords visible. Furthermore, at 7%, we report a much lower incidence of no fibreoptic view of the vocal cords than Jagannathan et al. 10 (27%) and Sinha et al. 11 (30%), the difference being most striking in the smallest air-Q ILA sizes.
Explanations for the more optimized views we obtained are speculative. Although our patients were not paralyzed, our high incidence of intravenous induction ensured that the majority were apneic during device insertion. Perhaps differences in airway muscle tone that result from propofol-remifentanil induction and no muscle relaxant allow for more optimal positioning of the air-Q ILA compared with an inhalational induction followed by non-depolarizing muscle blockade. Whatever the reasons, these findings offer evidence to support the potential ability of the air-Q ILA to fulfill a role as a bridging airway that facilitates fibreoptic endotracheal intubation.
Our study has certain limitations. First, we studied individuals with normal airways. This approach was appropriate for an observational study of a newly marketed device intended for use as a first-choice SGD in pediatric patients. Whether the air-Q ILA will perform equally well in patients with a difficult airway and abnormal anatomy remains to be investigated. We5 and others6,10,15 have reported on the successful use of the air-Q ILA in pediatric difficult airway management. Second, some of our evaluation criteria are subjective and semi-quantitative. This is a common feature of “usability” studies, as is a third issue, i.e., operator experience. We tried to strike a balance between the extremes of a single very experienced operator, where the benefits of consistency of technique, application of methodology, and no interobserver variability may be offset by a lack of generalizability of findings, and “everyday” practitioners and a large number of investigators, where these relative advantages and disadvantages are reversed.
In conclusion, the air-Q ILA has performed satisfactorily as a primary airway in clinical pediatric anesthetic practice. It is easy to insert and produces an OLP and maximum VT that meet clinical goals. The excellent FOB view augurs well for FOB-guided endotracheal intubation through the air-Q ILA, which is currently being evaluated in a separate study.
References
American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology 2003; 98: 1269-77.
Goldmann K, Jakob C. Size 2 ProSeal laryngeal mask airway: a randomized, crossover investigation with the standard laryngeal mask airway in paediatric patients. Br J Anaesth 2005; 94: 385-9.
Goldmann K, Jakob C. A randomized crossover comparison of the size 2 1/2 laryngeal mask airway ProSeal versus laryngeal mask airway-Classic in pediatric patients. Anesth Analg 2005; 100: 1605-10.
Goldmann K, Roettger C, Wulf H. The size 1(1/2) ProSeal laryngeal mask airway in infants: a randomized, crossover investigation with the Classic laryngeal mask airway. Anesth Analg 2006; 102: 405-10.
Peiris K, Traynor M, Whyte S. Intubation via the intubating laryngeal airway in two pediatric patients with predicted difficult airways. Paediatr Anaesth 2010; 20: 202-4.
Jagannathan N, Roth AG, Sohn LE, Pak TY, Amin S, Suresh S. The new air-Q intubating laryngeal airway for tracheal intubation in children with anticipated difficult airway: a case series. Paediatr Anaesth 2009; 19: 618-22.
Henderson JJ, Popat MT, Latto IP, Pearce AC, Difficult Airway Society. Difficult Airway Society guidelines for management of the unanticipated difficult intubation. Anaesthesia 2004; 59: 675-94.
Weiss M, Engelhardt T. Proposal for the management of the unexpected difficult pediatric airway. Paediatr Anaesth 2010; 20: 454-64.
Brimacombe J, Berry A. A proposed fiber-optic scoring system to standardize the assessment of laryngeal mask airway position. Anesth Analg 1993; 76: 457.
Jagannathan N, Kozlowski RJ, Sohn LE, et al. A clinical evaluation of the intubating laryngeal airway as a conduit for tracheal intubation in children. Anesth Analg 2011; 112: 176-82.
Sinha R, Chandralekha, Ray BR. Evaluation of air-Q™ intubating laryngeal airway as a conduit for tracheal intubation in infants--a pilot study. Paediatr Anaesth 2012; 22: 156-60
Bakker EJ, Valkenburg M, Galvin EM. Pilot study of the air-Q intubating laryngeal airway in clinical use. Anaesth Intensive Care 2010; 38: 346-8.
Wheeler M. ProSeal laryngeal mask airway in 120 pediatric surgical patients: a prospective evaluation of characteristics and performance. Paediatr Anaesth 2006; 16: 297-301.
Micaglio M, Bonato R, De Nardin M, et al. Prospective, randomized comparison of ProSeal and Classic laryngeal mask airways in anaesthetized neonates and infants. Br J Anaesth 2009; 103: 263-7.
Jagannathan N, Kho MF, Kozlowski RJ, Sohn LE, Siddiqui A, Wong DT. Retrospective audit of the air-Q intubating laryngeal airway as a conduit for tracheal intubation in pediatric patients with a difficult airway. Paediatr Anaesth 2011; 21: 422-7.
Acknowledgements
We thank Dr. A. Morrison for providing input into the study design and conducting air-Q ILA insertions on recruited subjects, and we are grateful to Ms Disha Mehta for drafting the initial study proposal and ethics applications.
Funding
This study was part-funded by the award to SDW of the Canadian Anesthesiologists’ Society Baxter Corporation Canadian Research Award in Anesthesia. This study was also supported by in-kind donations from Cookgas and Mercury Medical, manufacturer and distributor, respectively, of the air-Q® ILA, who provided the air-Q ILA devices. The study investigators have analyzed and published study data independently, and neither Cookgas nor Mercury Medical had any input into the study design or conduct, data analysis, or manuscript preparation. None of the study investigators or their families receive remuneration from, hold shares in, or have any sort of contract with these companies.
Author information
Authors and Affiliations
Corresponding author
Additional information
This report was previously presented, in part, at the Canadian Anesthesiologists’ Society (June 25-29, 2010 in Montreal, QC, Canada) and the Society for Airway Management (September 24-26, 2010 in Chicago, IL, USA) 2010 Annual Meetings.
Rights and permissions
About this article
Cite this article
Whyte, S.D., Cooke, E. & Malherbe, S. Usability and performance characteristics of the pediatric air-Q® intubating laryngeal airway. Can J Anesth/J Can Anesth 60, 557–563 (2013). https://doi.org/10.1007/s12630-013-9918-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-013-9918-6