Abstract
Purpose
The 90° rotation technique for inserting the ProSeal™ laryngeal mask airway (PLMA) in anesthetized paralyzed patients was compared with the index finger insertion technique.
Methods
One hundred twenty Asian adult patients were randomly allocated to either a standard technique group or a rotation technique group. A PLMA size 4 was used for women and size 5 was used for men. In the standard technique group (n = 60), the PLMA was inserted using the index finger. In the rotation technique group (n = 60), the entire cuff of the PLMA was placed in the patient’s mouth in a midline approach without finger insertion, rotated 90° counter clockwise around the patient’s tongue, advanced and then rotated back until resistance was felt. The primary outcome was success at first insertion. Secondary outcome measures were insertion time and complications.
Results
The success rate at first insertion was greater for the rotation technique group than for the standard technique group (100% vs 83%, respectively; P = 0.003), and less time was required (11 ± 3 sec vs 19 ± 16 sec, respectively; P = 0.03). The incidence of postoperative sore throat was lower for the rotation technique group than for the standard technique group (12% vs 33%, respectively; P = 0.009), and blood staining on the PLMA was less (8% vs 40%, respectively; P < 0.001).
Conclusion
The 90° rotation technique for inserting the PLMA is more successful than the standard index finger insertion technique. It is associated with fewer side effects, such as blood on the PLMA and sore throat, which suggests it causes less pharyngeal trauma. (Clinical trial registration number: NCT00966186).
Résumé
Objectif
La technique de rotation à 90° pour insérer le masque laryngé ProSeal™ (PLMA) chez des patients anesthésiés curarisés a été comparée à la technique d’insertion avec l’index.
Méthode
Cent vingt patients adultes asiatiques ont été aléatoirement répartis en deux groupes, soit un groupe avec technique d’insertion standard et l’autre avec technique de rotation. Un masque PLMA de taille 4 a été utilisé chez les femmes et un masque de taille 5 chez les hommes. Dans le groupe avec technique d’insertion standard (n = 60), le PLMA a été inséré à l’aide de l’index. Dans le groupe avec technique de rotation (n = 60), la manchette du PLMA a été placée en entier dans la bouche du patient à l’aide d’une approche par ligne médiane sans insertion de doigt, tournée de 90° dans le sens inverse des aiguilles d’une montre autour de la langue du patient, avancée puis retournée jusqu’à ressentir une résistance. Le critère d’évaluation principal était la réussite à la première insertion. Les critères d’évaluation secondaires comprenaient le temps d’insertion et les complications.
Résultats
Le taux de réussite à la première insertion était plus élevé dans le groupe avec technique de rotation que dans le groupe avec technique d’insertion standard (100 % vs 83 %, respectivement; P = 0,003), et a requis moins de temps (11 ± 3 sec vs 19 ± 16 sec, respectivement; P = 0,03). L’incidence de mal de gorge postopératoire était plus basse dans le groupe avec technique de rotation que dans le groupe avec technique d’insertion standard (12 % vs 33 %, respectivement; P = 0,009), et il y avait moins de taches de sang sur le PLMA (8 % vs 40 %, respectivement; P < 0,001).
Conclusion
La technique de rotation à 90° pour insérer le PLMA donne de meilleurs résultats que la technique d’insertion standard avec l’index. Elle est associée à moins d’effets secondaires tels que des traces de sang sur le PLMA et les maux de gorge, ce qui suggère qu’elle provoque moins de traumatisme pharyngé. (Numéro d’enregistrement de l’étude clinique : NCT00966186).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The ProSeal™ laryngeal mask airway (PLMA) (Laryngeal Mask Co. Ltd, Mahe, Seychelles) has a drainage tube and achieves a good seal.1,2 However, the PLMA has a larger cuff than the Classic™ laryngeal mask airway (LMA), which makes it more difficult to insert. The success rate for first-time insertion is lower for the PLMA than for the LMA, and more time is required to achieve an effective airway, even when it is inserted by a well-trained physician.1–3 Strategies, such as partial inflation of the cuff4 and the use of an introducer5 and a laryngoscope6 guide, have been investigated to improve the ease of insertion of PLMAs. The 90° rotation technique was introduced to improve success with inserting the PLMA. In a recent study, the rotation technique was associated with a higher success rate and less postoperative sore throat than the standard technique.7 However, the study was limited to small-sized (size 3) PLMAs and women patients breathing spontaneously undergoing brief surgery. Larger sizes (size 4 or 5 for women and size 5 for men) are recommended to ensure a good seal and to allow positive pressure ventilation.8–10 Although large PLMAs result in a better seal, they are associated with greater pharyngolaryngeal morbidity.8,9 Rotation of the large cuff of the PLMA in the patient’s mouth can be difficult or traumatic.
In this prospective study, we investigated the usefulness of the 90° rotation technique for inserting a large-sized PLMA in anesthetized paralyzed patients and compared it with the index finger insertion technique. We used insertion success rate and insertion time to indicate ease of insertion, and we used blood on the surface of the cuff and the incidence of postoperative sore throat as indices of complications.
Methods
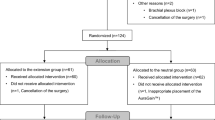
This study was approved by the Institutional Review Board of Seoul National University Bundang Hospital, and written informed consent was obtained from all patients. The randomized controlled trial was registered August 20, 2009 at clinicalTrials.gov (NCT00966186). We screened 122 Asian adult patients over a six-month period (age range 27–75 yr, American Society of Anesthesiologists physical status I–II) who required general anesthesia with a PLMA for elective surgery. The exclusion criteria included a predicted difficult airway, mouth opening < 2.5 cm, sore throat, and high risk of aspiration (non-fasted subjects or gastroesophageal reflux disease). Two patients were excluded due to a sore throat prior to surgery; consequently, 120 patients were finally enrolled. The patients were randomly allocated to the two insertion techniques by block randomization (block size 6), and the assignments were concealed under opaque cover until immediately before induction.
Midazolam 0.04 mg·kg−1 was administered intravenously as premedication 15 min before induction of anesthesia. The patients were monitored using an electrocardiogram, a pulse oximeter, a noninvasive blood pressure monitor, and a gas analyzer. Anesthesia was induced using a plasma propofol target concentration of 7 μg·mL−1 and an intravenous injection of alfentanil 5 μg·kg−1 and was maintained using a propofol concentration of 2–4 μg·mL−1 in 50% O2 and air. Propofol was infused through a target-controlled infusion device (Orchestra™, Frenius-Vial, Brezins, France), and the Marsh pharmacokinetic model was applied. Neuromuscular blockade was achieved using rocuronium 0.6 mg·kg−1. The patient was placed in the supine position with the head resting on a 3-cm high pillow. A water-based lubricant gel without local anesthetic was applied to the posterior surface of the PLMA. Regardless of body weight, we used a size 4 PLMA for women and a size 5 PLMA for men. The cuff was fully deflated before insertion. Heart rate and mean blood pressure were recorded one minute before and one minute after insertion.
Insertion of the PLMA was performed by one of two anesthesiologists who had both completed the 90° rotation insertion technique > 50 times and the conventional finger insertion technique > 100 times. The 90° rotation technique involved the following steps. Holding the midportion of the airway tube of the PLMA, the entire cuff was placed into the patient’s mouth via the midline approach without finger insertion. The airway tube was rotated 70°–90° counter-clockwise from outside the mouth so that the cuff was turned around the tongue to come to rest to the right side of the tongue. The PLMA was then advanced into the hypopharynx until resistance was felt. During advancement, the PLMA was rotated back to the midline. The standard technique was conducted using the index finger insertion technique according to the manufacturer’s instruction manual.5 The index finger was placed in the retaining strap. The PLMA was pressed against the hard palate and advanced into the hypopharynx. The introducer tool was not used.
The PLMA was connected to a breathing circuit after insertion. The cuff was inflated with air (size 4, 15 mL; size 5, 20 mL) to 50% of the recommended maximum volume.11 Airway pressure and end-tidal CO2 concentration were monitored. Insertion time was defined as the interval between picking up the PLMA and achieving an effective airway as determined by the physician blinded to the study. An effective airway was defined as normal thoracoabdominal movement and a square wave capnograph tracing during gentle manual ventilation. The number of insertion attempts was recorded. If insertion failed after three attempts using the same technique, one additional attempt was permitted using the other technique. The ease of insertion was assessed according to insertion success rate and insertion time.
Airway seal pressure was defined as equilibrium airway pressure (maximum allowed = 40 cm H2O) when the expiratory valve of the breathing circuit was closed and a gas flow rate of 3 L·min−1 was maintained.12 The locations of airway gas leaks at airway seal pressure were classified as the mouth (audible),12 the stomach (epigatric auscultation),13 or the PLMA drainage tube (bubbling of lubricant placed on the proximal end of the drainage tube).1
The PLMA was removed after surgery when the patients were able to breathe spontaneously and obey commands. Blood staining on the PLMA was noted upon its removal and sore throat (throat pain at rest or when swallowing) was assessed before discharge to the ward by a nurse blinded to the method of insertion.
Statistical analysis
The primary outcome measurement was first-attempt insertion success rate. A previous study3 reported that the success rate for first-attempt insertion of the PLMA using the standard technique was 82%. Expecting a 20% improvement in success rate to 99% with the rotation technique, 57 patients per group were required assuming a type 1 error of 0.05 (two-tailed) and a power of 0.8.14 The Student’s t test was used to compare the demographic data between groups, and insertion time was compared by the rank sum test because it failed the normality test. A repeated measures analysis of variance was used to evaluate the effect of insertion on blood pressure and heart rate. Sex ratio, success rates, the presence of the blood on the PLMA, and the occurrence of complications were compared using Chi square analysis or Fisher’s exact test. A value of P < 0.05 was considered as indicating a statistically significant difference.
Results
Demographic characteristics and duration of surgery were similar in both groups (Table 1). The success rate for first-attempt insertion was better for the rotation technique than for the standard technique (100% vs 83%, respectively; P = 0.003). The overall success rate for the standard technique was 95%, and there was no statistically significant difference between techniques. In three patients, there were three consecutive unsuccessful attempts to insert the PLMA using the standard technique. The PLMA was subsequently inserted using the rotation technique. Less time was required to achieve an effective airway with the rotation technique than with the standard technique (11 sec vs 19 sec, respectively; P = 0.03) (Table 2). Airway seal pressure was similar in both groups. There was no significant change in heart rate, but blood pressure change showed group-insertion interaction effect (P < 0.001) (Table 3). The incidence of blood staining was less for the rotation technique than for the standard technique (8% vs 40%, respectively; P < 0.001), as was the incidence of sore throat (12% vs 33%, respectively; P = 0.009) (Table 3).
Discussion
This study demonstrates that the 90° rotation technique has advantages over the standard technique for insertion of PLMAs in anesthetized paralyzed patients. In the current study, PLMA size 4 was used for women and PLMA size 5 was used for men. Selection of an appropriately sized device is important for safety and for securing an effective airway. Many studies have been conducted to determine the optimal sizes for the Classic™ LMA15,16 and the PLMA.8–10 Grady et al.15 suggested that a small LMA (size 4) decreases the incidence of sore throat in spontaneously breathing male patients. They reported that a large LMA increased the risk of sore throat fourfold.15 However, many investigators recommend routine use of a large size for general anesthesia.8,10,16 Kihara et al.10 showed that selection of PLMA size according to sex was more appropriate than selection according to the manufacturer’s weight-based guidelines5 (size 3, 30–70 kg; size 4, > 70–90 kg; and size 5, > 90 kg). The main reason for this recommendation was that the large size had a higher oropharyngeal leak pressure. The adequacy of the seal is very important during positive pressure ventilation, especially in patients undergoing laparoscopic surgery. Even in the Asian population, a size 5 PLMA for men and a size 4 PLMA for women resulted in better seals than smaller sizes.9
The ProSeal™ LMA was reportedly more difficult to insert than the Classic™ LMA.1,3 Its larger cuff makes it difficult to place in the oral cavity and leaves little room for insertion of an index finger or thumb. During our study, we experienced difficulty inserting size 5 PLMAs into small-sized male patients using the index finger. The 90° rotation technique does not require the insertion of a finger, which avoids finger trauma and glove contamination with blood or saliva.
Many techniques have been proposed to improve the success rate of PLMA insertion.2 The introducer tool was no more successful than the standard digital technique.17 The Eschmann® Tracheal Introducer (commonly known as gum elastic bougie)-guided railroading technique has an excellent first-attempt success rate (100%). Therefore, the railroading technique is suggested as a useful backup technique when other techniques fail.17 The 90° rotation insertion technique is convenient because it does not require additional devices. Insertion simply consists of insertion of the PLMA into the oral cavity, rotation around the tongue, and advancement. We were initially concerned that it would be difficult to rotate the large cuff in the mouth. However, this proved not to be problematic, and we never failed to insert PLMAs using the rotation insertion technique. Moreover, the first attempt with the rotation technique was successful in the three patients in whom three previous attempts with the standard technique had been unsuccessful.
The subjects in this study were all Asians with relatively small body statures, which may be responsible for the higher incidence of blood staining on the PLMAs and sore throats in the standard technique group than in the rotation technique group. Tan et al.9 compared success rate, seal pressure, and mucosal trauma between two sizes of PLMA in an Asian population. They reported that a size 5 PLMA resulted in a better seal but was more traumatic compared with size 4. A size 5 caused mucosal injury in 36% of Asian men compared with 20% of Caucasian patients.8 In this study, the rotation technique reduced the incidence of mucosal bleeding (8%) and sore throat (12%) compared with the index finger insertion technique, suggesting that the rotation technique causes less pharyngeal trauma. The decreased incidence of complications may be associated with reduced resistance between the tip of the PLMA head and the pharyngeal wall.
This study has some limitations. First, as the PLMAs were inserted by two anesthesiologists who were experts in PLMA insertion, these results may not apply to novices. Further evaluation of the rotation insertion technique in the hands of inexperienced personnel is required. Second, it was impossible to blind the anesthesiologists to the insertion technique, which may have been a source of bias even though assessment of insertion time, blood pressure change, and postoperative complications was conducted by another person blinded to the insertion method. Third, we did not assess the position of the PLMA directly using a bronchoscope, and correct positioning was confirmed by clinical assessment only.
In conclusion, the 90° rotation insertion technique improves the ease of inserting a large PLMA and results in less pharyngeal trauma. We suggest this technique as the first choice for insertion of PLMAs in anesthetized paralyzed patients.
References
Brimacombe J, Keller C. The ProSeal laryngeal mask airway: a randomized, crossover study with the standard laryngeal mask airway in paralyzed, anesthetized patients. Anesthesiology 2000; 93: 104–9.
Cook TM, Lee G, Nolan JP. The ProSeal laryngeal mask airway: a review of the literature. Can J Anesth 2005; 52: 739–60.
Brimacombe J, Keller C, Fullekrug B, et al. A multicenter study comparing the ProSeal and Classic laryngeal mask airway in anesthetized, nonparalyzed patients. Anesthesiology 2002; 96: 289–95.
Matta BF, Marsh DS, Nevin M. Laryngeal mask airway: a more successful method of insertion. J Clin Anesth 1995; 7: 132–5.
LMA™ Airway Instruction Manual. San Diego: LMA North America; 2005. Available from URL: http://s7672.gridserver.com/docs/LMA_Airways_Manual.pdf (accessed November 2009)
Koay CK, Yoong CS, Kok P. A randomized trial comparing two laryngeal mask airway insertion techniques. Anaesth Intensive Care 2001; 29: 613–5.
Hwang JW, Park HP, Lim YJ, Do SH, Lee SC, Jeon YT. Comparison of two insertion techniques of ProSeal laryngeal mask airway: standard versus 90-degree rotation. Anesthesiology 2009; 110: 905–7.
Kihara S, Brimacombe J. Sex-based ProSeal laryngeal mask airway size selection: a randomized crossover study of anesthetized, paralyzed male and female adult patients. Anesth Analg 2003; 97: 280–4.
Tan SM, Sim YY, Koay CK. The ProSeal laryngeal mask airway size selection in male and female patients in an Asian population. Anaesth Intensive Care 2005; 33: 239–42.
Kihara S, Brimacombe JR, Yaguchi Y, Taguchi N, Watanabe S. A comparison of sex- and weight-based ProSeal laryngeal mask size selection criteria: a randomized study of healthy anesthetized, paralyzed adult patients. Anesthesiology 2004; 101: 340–3.
Brimacombe J, Holyoake L, Keller C, et al. Pharyngolaryngeal, neck, and jaw discomfort after anesthesia with the face mask and laryngeal mask airway at high and low cuff volumes in males and females. Anesthesiology 2000; 93: 26–31.
Keller C, Brimacombe JR, Keller K, Morris R. Comparison of four methods for assessing airway sealing pressure with the laryngeal mask airway in adult patients. Br J Anaesth 1999; 82: 286–7.
Brimacombe J, Keller C, Kurian S, Myles J. Reliability of epigastric auscultation to detect gastric insufflation. Br J Anaesth 2002; 88: 127–9.
Brasher PM, Brant RF. Sample size calculations in randomized trials: common pitfalls. Can J Anesth 2007; 54: 103–6.
Grady DM, McHardy F, Wong J, Jin F, Tong D, Chung F. Pharyngolaryngeal morbidity with the laryngeal mask airway in spontaneously breathing patients: does size matter? Anesthesiology 2001; 94: 760–6.
Voyagis GS, Batzioulis PG, Secha-Doussaitou PN. Selection of the proper size of laryngeal mask airway in adults. Anesth Analg 1996; 83: 663–4.
Brimacombe J, Keller C, Judd DV. Gum elastic bougie-guided insertion of the ProSeal laryngeal mask airway is superior to the digital and introducer tool techniques. Anesthesiology 2004; 100: 25–9.
Funding
Support was received from institutional and departmental sources.
Conflicts of interest
None declared.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jeon, YT., Na, H.S., Park, SH. et al. Insertion of the ProSeal™ laryngeal mask airway is more successful with the 90° rotation technique. Can J Anesth/J Can Anesth 57, 211–215 (2010). https://doi.org/10.1007/s12630-009-9241-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-009-9241-4