Abstract
Purpose
While infraorbital nerve blocks have demonstrated analgesic benefits for pediatric nasal and facial plastic surgery, no studies to date have explored the effect of this regional anesthetic technique on adult postoperative recovery. We designed this study to test the hypothesis that infraorbital nerve blocks combined with a standardized general anesthetic decrease the duration of recovery following outpatient nasal surgery.
Methods
At a tertiary care university hospital, healthy adult subjects scheduled for outpatient nasal surgery were randomly assigned to receive bilateral infraorbital injections with either 0.5% bupivacaine (Group IOB) or normal saline (Group NS) using an intraoral technique immediately following induction of general anesthesia. All subjects underwent a standardized general anesthetic regimen and were transported to the recovery room following tracheal extubation. The primary outcome was the duration of recovery (minutes) from recovery room admission until actual discharge to home. Secondary outcomes included average and worst pain scores, nausea and vomiting, and supplemental opioid requirements.
Results
Forty patients were enrolled. A statistically significant difference in mean [SD] recovery room duration was not observed between Groups IOB and NS (131 [61] min vs 133 [58] min, respectively; P = 0.77). Subjects in Group IOB did experience a reduction in average pain on a 0–100 mm scale (mean [95% confidence interval]) compared to Group NS (−11 [−21 to 0], P = 0.047), but no other comparison of secondary outcomes was statistically significant.
Conclusions
When added to a standardized general anesthetic, bilateral IOB do not decrease actual time to discharge following outpatient nasal surgery despite a beneficial effect on postoperative pain.
Résumé
Objectif
Malgré que les bienfaits analgésiques des blocs du nerf sous-orbitaire aient été démontrés pour la chirurgie nasale pédiatrique et la chirurgie plastique faciale, à ce jour aucune étude n’a exploré l’effet de cette technique d’anesthésie régionale sur la récupération postopératoire chez l’adulte. Nous avons conçu cette étude de façon à tester l’hypothèse selon laquelle les blocs du nerf sous-orbitaire associés à un anesthésique général standard réduisent le temps de récupération après une chirurgie nasale ambulatoire.
Méthode
Dans un hôpital universitaire de soins tertiaires, des patients adultes sains devant subir une chirurgie nasale ambulatoire ont été répartis aléatoirement en deux groupes, l’un recevant des injections sous-orbitaires bilatérales avec de la bupivacaïne 0,5 % (groupe IOB), et l’autre une solution physiologique (groupe NS) à l’aide d’une technique intra-buccale immédiatement après l’induction de l’anesthésie générale. Tous les patients ont reçu une anesthésie standard et ont été transférés à la salle de réveil après l’extubation trachéale. Le critère d’évaluation primaire était la durée de la récupération (minutes) à partir de l’admission en salle de réveil jusqu’au congé effectif de l’hôpital. Les critères d’évaluation secondaires comprenaient les scores de douleur moyens et extrêmes, les nausées et vomissements, ainsi que les besoins additionnels en opiacés.
Résultats
Quarante patients ont participé à l’étude. Une différence statistiquement significative dans le temps moyen [ET] passé en salle de réveil n’a pas été observée entre les groupes IOB et NS (131 [61] min vs. 133 [58] min, respectivement; P = 0,77). Les patients du groupe IOB ont ressenti une douleur moyenne réduite sur une échelle de 0 à 100 mm (moyenne [intervalle de confiance 95 %]) par rapport au groupe NS (-11 [-21 – 0], P = 0,047), mais aucune autre comparaison parmi les critères d’évaluation secondaires n’a été statistiquement significative.
Conclusion
Lorsqu’il est ajouté à une anesthésie générale standard, le bloc sous-orbitaire bilatéral ne réduit pas le temps effectif jusqu’au congé après une chirurgie nasale ambulatoire, malgré son effet bénéfique sur la douleur postopératoire.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Infraorbital nerve blocks (IOB) have been shown to improve postoperative analgesia following pediatric cleft lip and intranasal surgery.1–5 Limited reports in adult patients suggest IOB to be an effective anesthetic for minor nasal procedures when used alone6 and may decrease consumption of anesthetic agents when used in combination with general anesthesia.7 However, the benefits of these nerve blocks, if any, on postoperative recovery outcomes in adult patients have not been previously studied.
Postoperative nausea and vomiting (PONV) and pain are factors predictive of prolonged postanesthetic recovery,8 and anesthetic techniques that minimize their incidence potentially lead to increased patient satisfaction.9 Peripheral nerve blocks used for other outpatient surgeries have been shown to provide superior pain relief without clinically significant side effects.10–12
We designed this study to test the primary hypothesis that the addition of IOB to a standardized general anesthetic decreases the duration of postanesthetic recovery following outpatient nasal surgery. The secondary aim of this study was to determine the effect of IOB on the quality of postanesthetic recovery in terms of analgesia and incidence of side effects.
Methods
After Institutional Review Board approval (University of California, San Diego School of Medicine, San Diego, CA, USA), we offered study enrolment to adult patients (18–75 years of age) with American Society of Anesthesiologists physical status I or II scheduled for outpatient nasal surgery (e.g., septoplasty, rhinoplasty, endoscopic sinus surgery, nasal reconstruction, or combination) to be performed by a single surgeon (DW). Exclusion criteria included pregnancy, incarceration, allergy to local anesthetic medication, bleeding disorder, chronic pain condition, or an inability to comprehend or adhere to the study protocol. Demographic, morphometric, and surgical procedure-related characteristics were recorded for each subject.
Following written informed consent, the subjects were randomly assigned to one of two groups using a computer-generated block randomization scheme. The subjects assigned to Group IOB would receive bilateral IOB with 0.5% bupivacaine after the induction of general anesthesia. The subjects in Group NS would receive bilateral infraorbital injections of preservative-free normal saline. The subjects, clinical health care providers, and study investigators, including the statistician, were unaware of treatment group assignments (triple-masked design).
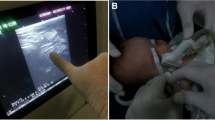
After anesthetic induction and tracheal intubation, infraorbital injections were performed by regional anesthesia attending staff or by regional anesthesia fellows under the direct supervision of attending staff. After retracting the upper lip, a 25-gauge, 2.54 cm needle attached to a 10 mL 3-ring control syringe was inserted anterior to the ipsilateral canine tooth along the maxilla. The needle was then directed superiorly toward the infraorbital foramen on the ipsilateral side, as previously described.13,14 Appropriate needle placement was confirmed by palpating the needle tip in proximity to the infraorbital foramen and by inability to aspirate blood. Three millilitres of study solution (0.5% plain bupivacaine for Group IOB or preservative-free normal saline for Group NS) were then injected while palpating the expanding wheal over the infraorbital foramen. An additional 3 mL of the same study solution were injected on the contralateral side using an identical technique. To preserve masking, study solutions were prepared independently by staff not involved in the care of the subjects enrolled in the study and not involved in the study itself.
Anesthetic maintenance consisted of sevoflurane in a 70% nitrous oxide/30% oxygen mixture titrated to a bispectral index (BIS) level of 40–60. Each subject received dexamethasone 10 mg iv for the prevention of postoperative swelling and local infiltration with 10 mL of 1% lidocaine with epinephrine 10 μg · mL−1 for hemostasis, according to the routine practice of the surgeon (DW). Since dexamethasone was administered per protocol, this was considered appropriate monotherapy for anti-emetic prophylaxis, and no additional anti-emetics were given.15 After anesthetic emergence and removal of the tracheal tube, the subjects were transported to the postanesthesia care unit (PACU).
Standard postoperative analgesic orders included hydromorphone 0.2–0.4 mg iv as needed for pain (the visual analog scale [VAS] ≥ 4). The subjects were discharged home directly from the PACU with a caretaker. All subjects were given a prescription for an oral analgesic medication, i.e., combined acetaminophen-hydrocodone tablets (500 mg and 5 mg, respectively), to take every 4–6 h as needed for pain.
The primary outcome of the study was the actual duration of postanesthesia recovery, which was defined as the time in minutes from t 0 (time of admission to the PACU) until PACU discharge to home. Each subject was assigned to a nurse who assessed eligibility for discharge every 15 min. Discharge eligibility was determined by our institution’s modification of a numerical scoring system (modified Aldrete)16,17 incorporating individual scores for vital signs, activity and mental status, pain, PONV, bleeding, and intake/output. Subjects were considered “home ready” when they achieved a score comparable to baseline (≥19 out of a possible 21 points).
Regarding secondary outcomes, the subjects’ postoperative pain, PONV, and intravenous opioid requirements were assessed and recorded every 30 min until discharge. The visual analog scale was used to assess pain18,19 and nausea.20 The subjects indicated their pain and nausea VAS scores at each time point using a 100 mm slide ruler (0 = None, 100 = Worst imaginable). On postoperative day one, the subjects were surveyed via telephone interview regarding their average and worst pain scores (using the verbal Numeric Rating Scale [NRS] 0–100; 0 = None, 100 = Worst imaginable for pain21) in the previous 24 h and regarding their oral analgesic consumption. The subjects were asked to rate their satisfaction with postanesthesia recovery on a Likert scale (1 = Not satisfied, 2 = Worse than expected, 3 = As expected, 4 = Better than expected, 5 = Extremely satisfied). The time to achieve discharge criteria in minutes was also recorded. All study-related data were collected by an independent research assistant who was masked to treatment group assignment.
Statistical analysis
In an unpublished retrospective pilot study (n = 16), PACU duration (min) for patients who received general anesthesia with IOB using the previously described technique was compared with age- and gender-matched controls who received general anesthesia alone. PACU duration (mean [SD]) was 132 [38] min for patients who received IOB vs 182 [34] min for their matched controls (P = 0.015). A sample size of 14 subjects per group for the present study was calculated using the following assumptions: the study control group would have a similar PACU recovery time (mean [SD]) to pilot controls; the standard deviations of the recovery time for both study groups would equal those of the pilot groups; 80% power, α = 0.05 (two-sided); and precision to detect a difference of 40 min between groups (NCSS and PASS Software, Kaysville, UT, USA). We enrolled 20 patients per group to allow for up to 30% dropout.
Statistical analysis was conducted with the software program SPSS version 12.0 (SPSS Inc., Chicago, IL, USA). Normality of distribution was determined using the Kolmogorov–Smirnov test. Student’s t test was used to compare normally distributed continuous variables. For distributions other than normal, a Mann–Whitney U test was applied. Comparisons of categorical variables, including differences in proportions, were analyzed by the Chi square test or the Fisher’s Exact test. For all comparisons, data were analyzed using the intention-to-treat principle with P < 0.05 considered statistically significant.
Results
Forty subjects were screened and enrolled, and all enrolled subjects completed the study protocol. The morphometric and surgical characteristics were similar between groups (Table 1).
With regard to the primary outcome, subjects in Group IOB were discharged after a total time (mean [SD]) of 131 [61] min compared with 133 [58] min for Group NS (P = 0.77). This difference (mean [95% confidence interval]) was −2.6 [−40.5 to 35.4] min and not statistically significant.
Analysis of secondary outcomes revealed a reduction in average VAS pain scores (mean [95% confidence interval]) reported in the PACU by subjects in Group IOB compared with subjects in Group NS (−11 [−21 to 0], P = 0.047) with a trend towards a decrease in intravenous opioid requirements, but differences in other PACU secondary outcomes were not statistically significant (Table 2). Average time to achieve discharge eligibility (mean [SD]) was 15 [31] min in Group IOB vs 22 [32] min in Group NS (P = 0.497).
In the first 24 h, there were trends for subjects in Group IOB to report lower NRS scores (mean [SD]) for worst pain (29 [27]) than subjects in Group NS (43 [23], P = 0.114) and to use fewer oral opioid tablets (Group IOB 2.1 [1.7] vs Group NS 3.3 [2.3], P = 0.057). Average NRS pain scores in the first 24 h were similar in both groups (Group IOB 20 [20] vs Group NS 26 [20], P = 0.403).
Subjects in Groups IOB and NS reported similar satisfaction scores on a Likert scale (median [25th–75th percentile]) of 5.0 [3.3–5.0] and 5.0 [4.0–5.0], respectively) (P = 0.694). There were no protocol deviations or adverse events related to study procedures.
Discussion
When added to a standardized general anesthetic regimen, bilateral infraorbital nerve blocks do not decrease time to PACU discharge following outpatient nasal and sinus surgery despite a beneficial effect on postoperative pain.
The subjects in our treatment group reported less pain, on average, than subjects who received placebo. In addition, there were trends toward decreased opioid requirements in PACU and at home and worst pain scores for the first 24 h that should be investigated in future studies. Yet, the subjects who received IOB did not return home sooner.
Although pain control is an important outcome in postoperative recovery,8,22 we consider total PACU duration to be the most clinically relevant outcome in outpatient surgery for reasons related to perioperative management. Actual duration of recovery influences perioperative costs, PACU staffing, and patient satisfaction. We had hypothesized that minimizing the incidence of general-anesthetic-induced side effects and pain by using peripheral nerve blocks would result in a quantifiable decrease in PACU length of stay compared with general anesthesia alone. Rather than investigating the time to achieve discharge criteria as in previous studies,23 we chose to measure actual discharge time as our primary outcome in this study.
Previous investigators have theorized that many of the causes of discharge delays are unrelated to medical or surgical issues and remain unaccounted for by established predictive models.23–26 Social and system issues can account for 34% of the delays in discharge, even after patients achieve home readiness.25 We can only speculate that non-medical issues at our institution, such as waiting for prescriptions to be filled by pharmacy or unavailability of transportation, may have contributed to delayed discharge.
A possible limitation in the present study is the fact that our surgical outpatients are discharged directly from Phase I PACU while published studies demonstrating the beneficial effects of regional anesthesia on discharge times have employed Phase II (step-down) recovery units.27,28 Process improvements at our institution may be necessary to take advantage of the analgesic benefits of nerve block techniques and to facilitate fast-tracking of ambulatory surgery patients.
Since the IOB was performed intraoperatively under general anesthesia, sensory testing was not possible prior to surgery. Accurate postoperative assessment of nerve block success is made difficult by facial swelling, bruising, and surgical dressing, in addition to the potential for unmasking the research team and patient care staff. We employ the intraoral IOB technique in our practice, which is based on the volunteer crossover study by Lynch et al. 13 that demonstrated 100% efficacy in producing anesthesia in the nasal branches of the infraorbital nerves (V2) with longer anesthetic duration than achieved by using the percutaneous route. It is still possible that not all injections resulted in successful nerve blocks, and study data were analyzed according to the intention-to-treat principle.
Compared with published studies on oral analgesic efficacy in the setting of outpatient nasal surgery,29,30 the control group in our study did not experience moderate to severe pain after surgery as anticipated. Unique aspects of the surgeon’s technique or perioperative management employed in our study may have contributed to lower pain scores, but these data may also be the result of placebo effect or perhaps an analgesic effect of normal saline injections around the infraorbital nerves not previously described.
Although the nasal branches of the infraorbital nerves (V2) innervate the external nasal walls and portions of the nasal septum, nasal regions innervated by the terminal branches of the ophthalmic nerve (V1) remain unanesthetized after IOB. Perhaps combining distal V1 nerve blocks and IOB for nasal surgery deserves future investigation. For minor nasal surgeries that do not produce significant postoperative pain, perhaps the surgeon injecting long-acting local anesthetics directly into the surgical site may provide sufficient analgesia,31 although this technique and IOB have not yet been compared in a randomized fashion.
In conclusion, IOB does not result in a statistically significant reduction in PACU time, but duration of recovery may be influenced by many factors not necessarily related to medical or surgical issues. Given the potential analgesic benefits of infraorbital nerve blocks and the minimal risk involved, further prospective studies are warranted to clearly determine their role in the postoperative management of ambulatory nasal surgery patients.
References
Prabhu KP, Wig J, Grewal S. Bilateral infraorbital nerve block is superior to peri-incisional infiltration for analgesia after repair of cleft lip. Scand J Plast Reconstr Surg Hand Surg 1999; 33: 83–7.
Nicodemus HF, Ferrer MJ, Cristobal VC, de Castro L. Bilateral infraorbital block with 0.5% bupivacaine as post-operative analgesia following cheiloplasty in children. Scand J Plast Reconstr Surg Hand Surg 1991; 25: 253–7.
Bosenberg AT, Kimble FW. Infraorbital nerve block in neonates for cleft lip repair: anatomical study and clinical application. Br J Anaesth 1995; 74: 506–8.
McAdam D, Muro K, Suresh S. The use of infraorbital nerve block for postoperative pain control after transsphenoidal hypophysectomy. Reg Anesth Pain Med 2005; 30: 572–3.
Rajamani A, Kamat V, Rajavel VP, Murthy J, Hussain SA. A comparison of bilateral infraorbital nerve block with intravenous fentanyl for analgesia following cleft lip repair in children. Paediatr Anaesth 2007; 17: 133–9.
Molliex S, Navez M, Baylot D, Prades JM, Elkhoury Z, Auboyer C. Regional anaesthesia for outpatient nasal surgery. Br J Anaesth 1996; 76: 151–3.
Higashizawa T, Koga Y. Effect of infraorbital nerve block under general anesthesia on consumption of isoflurane and postoperative pain in endoscopic endonasal maxillary sinus surgery. J Anesth 2001; 15: 136–8.
Chung F, Mezei G. Factors contributing to a prolonged stay after ambulatory surgery. Anesth Analg 1999; 89: 1352–9.
Macario A, Weinger M, Carney S, Kim A. Which clinical anesthesia outcomes are important to avoid? The perspective of patients. Anesth Analg 1999; 89: 652–8.
Hadzic A, Arliss J, Kerimoglu B, et al. A comparison of infraclavicular nerve block versus general anesthesia for hand and wrist day-case surgeries. Anesthesiology 2004; 101: 127–32.
Hadzic A, Karaca PE, Hobeika P, et al. Peripheral nerve blocks result in superior recovery profile compared with general anesthesia in outpatient knee arthroscopy. Anesth Analg 2005; 100: 976–81.
Singelyn FJ, Lhotel L, Fabre B. Pain relief after arthroscopic shoulder surgery: a comparison of intraarticular analgesia, suprascapular nerve block, and interscalene brachial plexus block. Anesth Analg 2004; 99: 589–92.
Lynch MT, Syverud SA, Schwab RA, Jenkins JM, Edlich R. Comparison of intraoral and percutaneous approaches for infraorbital nerve block. Acad Emerg Med 1994; 1: 514–9.
Suresh S, Wheeler M. Practical pediatric regional anesthesia. Anesthesiol Clin North America 2002; 20: 83–113.
Gan TJ, Meyer T, Apfel CC, et al. Consensus guidelines for managing postoperative nausea and vomiting. Anesth Analg 2003; 97: 62–71.
Aldrete JA. Modifications to the postanesthesia score for use in ambulatory surgery. J Perianesth Nurs 1998; 13: 148–55.
Viitanen H, Annila P, Viitanen M, Tarkkila P. Premedication with midazolam delays recovery after ambulatory sevoflurane anesthesia in children. Anesth Analg 1999; 89: 75–9.
Bodian CA, Freedman G, Hossain S, Eisenkraft JB, Beilin Y. The visual analog scale for pain: clinical significance in postoperative patients. Anesthesiology 2001; 95: 1356–61.
Jensen MP, Chen C, Brugger AM. Interpretation of visual analog scale ratings and change scores: a reanalysis of two clinical trials of postoperative pain. J Pain 2003; 4: 407–14.
Korttila KT, Jokinen JD. Timing of administration of dolasetron affects dose necessary to prevent postoperative nausea and vomiting. J Clin Anesth 2004; 16: 364–70.
Farrar JT, Young JP Jr, LaMoreaux L, Werth JL, Poole RM. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain 2001; 94: 149–58.
Pavlin DJ, Chen C, Penaloza DA, Polissar NL, Buckley FP. Pain as a factor complicating recovery and discharge after ambulatory surgery. Anesth Analg 2002; 95: 627–34.
Edler AA, Mariano ER, Golianu B, Kuan C, Pentcheva K. An analysis of factors influencing postanesthesia recovery after pediatric ambulatory tonsillectomy and adenoidectomy. Anesth Analg 2007; 104: 784–9.
Liu SS, Strodtbeck WM, Richman JM, Wu CL. A comparison of regional versus general anesthesia for ambulatory anesthesia: a meta-analysis of randomized controlled trials. Anesth Analg 2005; 101: 1634–42.
Shirakami G, Teratani Y, Namba T, Hirakata H, Tazuke-Nishimura M. Delayed discharge and acceptability of ambulatory surgery in adult outpatients receiving general anesthesia. J Anesth 2005; 19: 93–101.
Seago JA, Weitz S, Walczak S. Factors influencing stay in the postanesthesia care unit: a prospective analysis. J Clin Anesth 1998; 10: 579–87.
Williams BA, Kentor ML, Vogt MT, et al. Economics of nerve block pain management after anterior cruciate ligament reconstruction: potential hospital cost savings via associated postanesthesia care unit bypass and same-day discharge. Anesthesiology 2004; 100: 697–706.
Williams BA, Kentor ML, Williams JP, et al. PACU bypass after outpatient knee surgery is associated with fewer unplanned hospital admissions but more phase II nursing interventions. Anesthesiology 2002; 97: 981–8.
Recart A, Issioui T, White PF, et al. The efficacy of celecoxib premedication on postoperative pain and recovery times after ambulatory surgery: a dose-ranging study. Anesth Analg 2003; 96: 1631–5.
Issioui T, Klein KW, White PF, et al. The efficacy of premedication with celecoxib and acetaminophen in preventing pain after otolaryngologic surgery. Anesth Analg 2002; 94: 1188–93.
Demiraran Y, Ozturk O, Guclu E, Iskender A, Ergin MH, Tokmak A. Vasoconstriction and analgesic efficacy of locally infiltrated levobupivacaine for nasal surgery. Anesth Analg 2008; 106: 1008–11.
Acknowledgments
The authors gratefully acknowledge the invaluable assistance of the entire Outpatient Surgery Center operating and recovery room staff at the University of California, San Diego Medical Center (San Diego, CA, USA).
Financial support
This work was supported by the National Institutes of Health, Bethesda, Maryland, USA [GM077026 to B.I., GM071400 to L.C.], and the Department of Anesthesiology, University of California, San Diego Medical Center. The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of this entity.
Conflicts of interest
None declared.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Additional information
A portion of the results of this investigation were presented at the Annual Meeting of the American Society of Anesthesiologists, Orlando, Florida, USA (October 18–22, 2008).
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Mariano, E.R., Watson, D., Loland, V.J. et al. Bilateral infraorbital nerve blocks decrease postoperative pain but do not reduce time to discharge following outpatient nasal surgery. Can J Anesth/J Can Anesth 56, 584–589 (2009). https://doi.org/10.1007/s12630-009-9119-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-009-9119-5