Abstract
Purpose
To investigate the association between sarcopenia and overactive bladder (OAB) in a United States adult population from 2011 to 2018, and whether sarcopenia can predict the risk of OAB.
Materials and Methods
We analyzed data from the 2011–2018 National Health and Nutrition Examination Survey in a crosssectional study(NHANES) of 8746 participants, of whom 1213 were diagnosed with OAB, we analyzed correlations by sex, age, race, education level, marital status, household income-to-poverty ratio, hypertension, diabetes, strenuous work activity, moderate work activity, strenuous recreational activity, moderate recreational activity, blood urea nitrogen, creatinine, and uric acid levels using restricted cubic spline plots of dose-response curves, univariate and multivariate Logistic regression. Models based on sex, age, education, household income to poverty ratio, hypertension, diabetes, sarcopenia index, and cotinine were developed and evaluated using Nomogram, calibration curves, receiver operating characteristic curves, and clinical decision curves.
Results
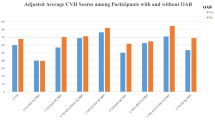
Of the 1213 OAB patients, 388 (32.0%) were male and 825 (68.0%) were female. Univariate and multivariate Logistic regression analysis showed that sarcopenia index was negatively correlated with the prevalence of OAB (OR=0.084, 95% CI, 0.056–0.130, P <0.001;OR=0.456, 95%CI, 0.215–0.968, P= 0.0041). Dose curve analysis of the sarcopenia index and prevalence of OAB showed that the prevalence of OAB decreased significantly with increasing sarcopenia index. Sarcopenia was positively correlated with OAB (OR=2.400, 95%CI, 2.000–2.800, P <0.001;OR=1.46, 95%CI, 1.096 −1.953, P = 0.010). In addition, our model shows that sarcopenia can predict the prevalence of OAB (AUC = 0.750) and has some clinical decision-making implications.
Conclusion
Sarcopenia is positively associated with the risk of OAB in United States adults and can be used as a predictor of OAB prevalence.





Similar content being viewed by others
Availability of data and material: The data and material that support the findings of this study are available from the corresponding author, Bo Peng, upon reasonable request.
References
Abrams P, Cardozo L, Fall M, et al The standardisation of terminology of lower urinary tract function: report from the standardisation sub-committee of the international continence society. Am J Obstet Gynecol 2002;187(1):116–126. doi: https://doi.org/10.1067/mob.2002.125704
Bo K, Frawley HC, Haylen BT, et al An international urogynecological association (iuga)/international continence society (ics) joint report on the terminology for the conservative and nonpharmacological management of female pelvic floor dysfunction. Int Urogynecol J 2017;28(2):191–213. doi: https://doi.org/10.1007/s00192-016-3123-4
Ikeda M, Nozawa K Prevalence of overactive bladder and its related factors in Japanese patients with diabetes mellitus. Endocr J 2015;62(9):847–854. doi: https://doi.org/10.1507/endocrj.EJ15-0237
Zecca C, Riccitelli GC, Disanto G, et al Urinary incontinence in multiple sclerosis: prevalence, severity and impact on patients’ quality of life. Eur J Neurol 2016;23(7):1228–1234. doi: https://doi.org/10.1111/ene.13010
Milsom I, Abrams P, Cardozo L, Roberts RG, Thuroff J, Wein AJ How widespread are the symptoms of an overactive bladder and how are they managed? A population-based prevalence study. BJU Int 2001;87(9):760–766. doi: https://doi.org/10.1046/j.1464-410x.2001.02228.x
Stewart W, Van Rooyen J, Cundiff G, et al Prevalence and burden of overactive bladder in the united states. World J Urol 2003;20(6):327–336. doi: https://doi.org/10.1007/s00345-002-0301-4
Mckellar K, Bellin E, Schoenbaum E, Abraham N Prevalence, risk factors, and treatment for overactive bladder in a racially diverse population. Urology 2019;126:70–75. doi: https://doi.org/10.1016/j.urology.2018.12.021
Cruz-Jentoft AJ, Sayer AA Sarcopenia. Lancet 2019;393(10191):2636–2646. doi: https://doi.org/10.1016/S0140-6736(19)31138-9
Anker SD, Morley JE, Haehling S Welcome to the icd-10 code for sarcopenia. Journal of Cachexia, Sarcopenia and Muscle 2016;7(5):512–514. doi: https://doi.org/10.1002/jcsm.12147
Cao L, Morley JE Sarcopenia is recognized as an independent condition by an international classification of disease, tenth revision, clinical modification (icd-10-cm) code. J Am Med Dir Assoc 2016;17(8):675–677. doi: https://doi.org/10.1016/j.jamda.2016.06.001
Mao W, Ma B, Wang K, et al Sarcopenia predicts prognosis of bladder cancer patients after radical cystectomy: a study based on the chinese population. Clin Transl Med 2020;10(2). doi: https://doi.org/10.1002/ctm2.105
Mao W, Wang K, Zhang H, et al Sarcopenia as a poor prognostic indicator for renal cell carcinoma patients undergoing nephrectomy in china: a multicenter study. Clin Transl Med 2021;11(1). doi: https://doi.org/10.1002/ctm2.270
Mao W, Zhang N, Wang K, et al Combination of albumin-globulin score and sarcopenia to predict prognosis in patients with renal cell carcinoma undergoing laparoscopic nephrectomy. Front Nutr 2021;8. doi: https://doi.org/10.3389/fnut.2021.731466
Shachar SS, Williams GR, Muss HB, Nishijima TF Prognostic value of sarcopenia in adults with solid tumours: a meta-analysis and systematic review. Eur J Cancer 2016;57:58–67. doi: https://doi.org/10.1016/j.ejca.2015.12.030
Sanchez-Rodriguez D, Marco E, Cruz-Jentoft AJ Defining sarcopenia: some caveats and challeng. Curr Opin Clin Nutr Metab Care 2020;23(2):127–132. doi: https://doi.org/10.1097/MCO.0000000000000621
Johnson Stoklossa CA, Sharma AM, Forhan M, Siervo M, Padwal RS, Prado CM Prevalence of sarcopenic obesity in adults with class ii/iii obesity using different diagnostic criteria. J Nutr Metab 2017;2017:1–11. doi: https://doi.org/10.1155/2017/7307618
Barbat-Artigas S, Pion CH, Leduc-Gaudet J, Rolland Y, Aubertin-Leheudre M Exploring the role of muscle mass, obesity, and age in the relationship between muscle quality and physical function. J Am Med Dir Assoc 2014;15(4):303–313. doi: https://doi.org/10.1016/j.jamda.2013.12.008
Blaivas JG, Panagopoulos G, Weiss JP, Somaroo C Validation of the overactive bladder symptom score. J Urol 2007;178(2):543–547. doi: https://doi.org/10.1016/j.juro.2007.03.133
Zhu S, Wang Z, Tao Z, Wang S, Wang Z Relationship between marijuana use and overactive bladder (oab): a cross-sectional research of nhanes 2005 to 2018. Am J Med 2023;136(1):72–78. doi: https://doi.org/10.1016/j.amjmed.2022.08.031
Li K, Chen C, Zeng J, et al Interplay between bladder microbiota and overactive bladder symptom severity: a cross-sectional study. BMC Urol 2022;22(1):39. doi: https://doi.org/10.1186/s12894-022-00990-0
Homma Y, Yoshida M, Seki N, et al Symptom assessment tool for overactive bladder syndrome—overactive bladder symptom score. Urology 2006;68(2):318–323. doi: https://doi.org/10.1016/j.urology.2006.02.042
Casals-Casas C, Desvergne B Endocrine disruptors: from endocrine to metabolic disruption. Annu Rev Physiol 2011;73:135–162. doi: https://doi.org/10.1146/annurevphysiol-012110-142200
Arab AM, Chehrehrazi M The response of the abdominal muscles to pelvic floor muscle contraction in women with and without stress urinary incontinence using ultrasound imaging. Neurourol Urodyn 2011;30(1):117–120. doi: https://doi.org/10.1002/nau.20959
Al-Shaiji TF, Radomski SB Relationship between body mass index and overactive bladder in women and correlations with urodynamic evaluation. Int Neurourol J 2012;16(3):126. doi: https://doi.org/10.5213/inj.2012.16.3.126
Zacche MM, Giarenis I, Thiagamoorthy G, Robinson D, Cardozo L Is there an association between aspects of the metabolic syndrome and overactive bladder? A prospective cohort study in women with lower urinary tract symptoms. Eur J Obstet Gynecol Reprod Biol 2017;217:1–5. doi: https://doi.org/10.1016/j.ejogrb.2017.08.002
Neumann P, Gill V Pelvic floor and abdominal muscle interaction: emg activity and intra-abdominal pressure. Int Urogynecol J Pelvic Floor Dysfunct 2002;13(2):125–132. doi: https://doi.org/10.1007/s001920200027
Sapsford RR, Hodges PW, Richardson CA, Cooper DH, Markwell SJ, Jull GA Co-activation of the abdominal and pelvic floor muscles during voluntary exercises. Neurourol Urodyn 2001;20(1):31–42. doi: https://doi.org/10.1002/1520-6777(2001)20:1<31::aidnau5>3.0.co;2-p
Acknowledgements: We are very grateful to all the participants in this research project.
Funding
Funding: The Shanghai Association for Science and Technology Commission (Grant No. 21142203400). This work was supported by National Natural Science Foundation of China (Grant No. 81870517;32070646). This research was supported by The National Key Research and Development Program of China (2021YFC2009300, 2021YFC200930X).
Author information
Authors and Affiliations
Contributions
Authors’ contributions: (I) Conception and design: Wei Song, Hui Zhang and Bo Peng. (II) Administrative support: Houliang Zhang and Haipeng Zhang. (III) Provision of study materials or patients: Yifan Zhang and Keyi Wang. (IV) Collection and assembly of data: Jinliang Ni and Keyi Wang. (V) Data analysis and interpretation: Wei Song and Huiqing Hu. (VI) Manuscript writing: All authors. (VII) Final approval of manuscript: All authors.
Corresponding authors
Ethics declarations
Ethical standrads: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study used previously collected deidentified data, which was deemed exempt from review by the Ethics Committee of the Tenth People’s Hospital of Shanghai.
Competing interests: The authors declare no competing interests.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Song, W., Hu, H., Ni, J. et al. The Role of Sarcopenia in Overactive Bladder in Adults in the United States: Retrospective Analysis of NHANES 2011–2018. J Nutr Health Aging 27, 734–740 (2023). https://doi.org/10.1007/s12603-023-1972-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-023-1972-3