Abstract
Background
Late-night overeating (LNOE) is closely associated with many health risk factors, but whether LNOE can increase the risk of death remains unknown. Thus, the prospective cohort study aimed to investigate the relationship between LNOE and mortality using data from the National Health and Nutrition Examination Survey.
Methods
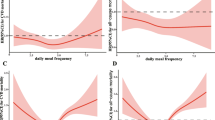
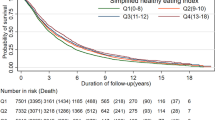
11,893 participants aged 50 years and older were included in the study. Dietary information was obtained through 24-h dietary recall interviews. Cox regression, subgroup, sensitivity, and restricted cubic spline analyses were used to assess the association between LNOE and mortality.
Results
During a median follow-up of 8.3 years, 2,498 deaths occurred. After adjusting for major confounders, compared to the non-late-night eating (NLNE) group, the LNOE group was associated with higher risks of all-cause (HR = 1.47, 95% CI = 1.06–2.04) and cardiovascular disease (CVD) mortality (HR = 2.02, 95% CI = 1.13–3.60). No significant association was found between late-night eating (LNE) and mortality. Subgroup analyses showed that the LNOE group had a greater risk of all-cause and CVD mortality in participants older than 70 years, with alcohol consumption and hypertension and demonstrated an increased risk of all-cause mortality in males and higher CVD mortality in females.
Conclusion
The habit of LNOE was an independent risk factor for all-cause and CVD mortality in US adults aged 50 years and older, which was also influenced by age, sex, alcohol consumption, and hypertension.



Similar content being viewed by others
Abbreviations
- LNOE:
-
late-night overeating
- dTEI:
-
daily total energy intake
- CVD:
-
cardiovascular disease
- NHANES:
-
National Health and Nutrition Examination Survey
- NCHS:
-
National Center for Health Statistics
- ICD-10:
-
10th Revision of the International Classification of Diseases
- LNEI:
-
late-night energy intake
- NLNE:
-
non-late-night eating
- LNE:
-
late-night eating
- HEI-2105:
-
Healthy Eating Index 2015
- BMI:
-
body mass index
- PA:
-
physical activity
- VIF:
-
variance inflation factor
- CI:
-
confidence interval
- HR:
-
hazard ratio
- PSM:
-
propensity score matching
- IQR:
-
interquartile range
References
Basdeki, E.D., K. Koumi, C. Tsirimiagkou, et al. Late-Night Overeating or Low-Quality Food Choices Late at Night Are Associated with Subclinical Vascular Damage in Patients at Increased Cardiovascular Risk[J]. Nutrients, 2022, 14(3) DOI: https://doi.org/10.3390/nu14030470.
van der Merwe, C., M. Münch, R. Kruger. Chronotype Differences in Body Composition, Dietary Intake and Eating Behavior Outcomes: A Scoping Systematic Review[J]. Adv Nutr, 2022, 13(6):2357–2405. DOI: https://doi.org/10.1093/advances/nmac093.
Ni, Y., L. Wu, J. Jiang, et al. Late-Night Eating-Induced Physiological Dysregulation and Circadian Misalignment Are Accompanied by Microbial Dysbiosis[J]. Mol Nutr Food Res, 2019, 63(24): e1900867. DOI: https://doi.org/10.1002/mnfr.201900867.
St-Onge, M.P., J. Ard, M.L. Baskin, et al. Meal Timing and Frequency: Implications for Cardiovascular Disease Prevention: A Scientific Statement From the American Heart Association[J]. Circulation, 2017, 135(9): e96–e121. DOI: https://doi.org/10.1161/cir.0000000000000476.
McHill, A.W., E.L. Melanson, J. Higgins, et al. Impact of circadian misalignment on energy metabolism during simulated nightshift work[J]. Proc Natl Acad Sci U S A, 2014, 111(48):17302–7. DOI: https://doi.org/10.1073/pnas.1412021111.
Reutrakul, S., E. Van Cauter. Sleep influences on obesity, insulin resistance, and risk of type 2 diabetes[J]. Metabolism, 2018, 84 56–66. DOI: https://doi.org/10.1016/j.metabol.2018.02.010.
Rynders, C.A., A. Bergouignan, E. Kealey, et al. Ability to adjust nocturnal fat oxidation in response to overfeeding predicts 5-year weight gain in adults[J]. Obesity (Silver Spring), 2017, 25(5):873–880. DOI: https://doi.org/10.1002/oby.21807.
Vujović, N., M.J. Piron, J. Qian, et al. Late isocaloric eating increases hunger, decreases energy expenditure, and modifies metabolic pathways in adults with overweight and obesity[J]. Cell Metab, 2022, 34(10):1486–1498.e7. DOI: https://doi.org/10.1016/j.cmet.2022.09.007.
Garaulet, M., J. Lopez-Minguez, H.S. Dashti, et al. Interplay of Dinner Timing and MTNR1B Type 2 Diabetes Risk Variant on Glucose Tolerance and Insulin Secretion: A Randomized Crossover Trial[J]. Diabetes Care, 2022, 45(3):512–519. DOI: https://doi.org/10.2337/dc21-1314.
Challet, E. The circadian regulation of food intake[J]. Nat Rev Endocrinol, 2019, 15(7):393–405. DOI: https://doi.org/10.1038/s41574-019-0210-x.
Ferreira, I., M.S. Huijberts. Eating at the right time of day: an underappreciated lifestyle therapy for hypertension?[J]. J Hypertens, 2013, 31(5):866–9. DOI: https://doi.org/10.1097/HJH.0b013e328360d602.
Tsirimiagkou, C., K. Karatzi, A. Argyris, et al. Levels of dietary sodium intake: diverging associations with arterial stiffness and atheromatosis[J]. Hellenic J Cardiol, 2021, 62(6):439–446. DOI: https://doi.org/10.1016/j.hjc.2021.02.005.
Pontzer, H., Y. Yamada, H. Sagayama, et al. Daily energy expenditure through the human life course[J]. Science, 2021, 373(6556):808–812. DOI: https://doi.org/10.1126/science.abe5017.
Cox, N.J., L. Morrison, S.M. Robinson, et al. Older individual’s perceptions of appetite, its loss, influencing factors and adaptions to poor appetite. A qualitative study[J]. Appetite, 2021, 167(105609. DOI: https://doi.org/10.1016/j.appet.2021.105609.
Treacy, D., L. Hassett, K. Schurr, et al. Mobility training for increasing mobility and functioning in older people with frailty[J]. Cochrane Database Syst Rev, 2022, 6(6): Cd010494. DOI: https://doi.org/10.1002/14651858.CD010494.pub2.
Pooler, J.A., H. Hartline-Grafton, M. DeBor, et al. Food Insecurity: A Key Social Determinant of Health for Older Adults[J]. J Am Geriatr Soc, 2019, 67(3):421–424. DOI: https://doi.org/10.1111/jgs.15736.
Pieroth, R., D. Rigassio Radler, P.M. Guenther, et al. The Relationship between Social Support and Diet Quality in Middle-Aged and Older Adults in the United States[J]. J Acad Nutr Diet, 2017, 117(8):1272–1278. DOI: https://doi.org/10.1016/j.jand.2017.03.018.
Delerue Matos, A., F. Barbosa, C. Cunha, et al. Social isolation, physical inactivity and inadequate diet among European middle-aged and older adults[J]. BMC Public Health, 2021, 21(1):924. DOI: https://doi.org/10.1186/s12889-021-10956-w.
Census Bureau. (Accessed April 26, 2023, at https://www.census.gov/newsroom/press-releases/2018/cb18-41-population-projections.html.).
Murray, C.J., C. Atkinson, K. Bhalla, et al. The state of US health, 1990–2010: burden of diseases, injuries, and risk factors[J]. Jama, 2013, 310(6):591–608. DOI: https://doi.org/10.1001/jama.2013.13805.
NCHS Data Linkage - Mortality Data - Public-Use Files. (Accessed April 26, 2023, at https://www.cdc.gov/nchs/data-linkage/mortality-public.htm.).
NHANES Questionnaires, Datasets, and Related Documentation. (Accessed April 26, 2023, at https://wwwn.cdc.gov/nchs/nhanes/Default.aspx.).
About the National Health and Nutrition Examination Survey. (Accessed April 26, 2023, at https://www.cdc.gov/nchs/nhanes/about_nhanes.htm.).
Chen, T.C., J. Clark, M.K. Riddles, et al. National Health and Nutrition Examination Survey, 2015–2018: Sample Design and Estimation Procedures[J]. Vital Health Stat 2, 2020, 184): 1–35.
Charidimou, A., S. Martinez-Ramirez, Y.D. Reijmer, et al. Total Magnetic Resonance Imaging Burden of Small Vessel Disease in Cerebral Amyloid Angiopathy: An Imaging-Pathologic Study of Concept Validation[J]. JAMA Neurol, 2016, 73(8):994–1001. DOI: https://doi.org/10.1001/jamaneurol.2016.0832.
Banna, J.C., M.A. McCrory, M.K. Fialkowski, et al. Examining Plausibility of Self-Reported Energy Intake Data: Considerations for Method Selection[J]. Front Nutr, 2017, 4(45. DOI: https://doi.org/10.3389/fnut.2017.00045.
Dashti, H.S., P. Gómez-Abellán, J. Qian, et al. Late eating is associated with cardiometabolic risk traits, obesogenic behaviors, and impaired weight loss[J]. Am J Clin Nutr, 2021, 113(1):154–161. DOI: https://doi.org/10.1093/ajcn/nqaa264.
Mogavero, M.P., L.M. DelRosso, F. Fanfulla, et al. Sleep disorders and cancer: State of the art and future perspectives[J]. Sleep Med Rev, 2021, 56(101409. DOI: https://doi.org/10.1016/j.smrv.2020.101409.
Almoosawi, S., S. Vingeliene, L.G. Karagounis, et al. Chrono-nutrition: a review of current evidence from observational studies on global trends in time-of-day of energy intake and its association with obesity[J]. Proc Nutr Soc, 2016, 75(4):487–500. DOI: https://doi.org/10.1017/s0029665116000306.
Yoshida, J., E. Eguchi, K. Nagaoka, et al. Association of night eating habits with metabolic syndrome and its components: a longitudinal study[J]. BMC Public Health, 2018, 18(1):1366. DOI: https://doi.org/10.1186/s12889-018-6262-3.
Li, M., L.A. Tse, W.C. Chan, et al. Nighttime eating and breast cancer among Chinese women in Hong Kong[J]. Breast Cancer Res, 2017, 19(1):31. DOI: https://doi.org/10.1186/s13058-017-0821-x.
Kaneko, H., H. Itoh, H. Kiriyama, et al. Possible association between eating behaviors and cardiovascular disease in the general population: Analysis of a nationwide epidemiological database[J]. Atherosclerosis, 2021, 320(79–85. DOI: https://doi.org/10.1016/j.atherosclerosis.2021.01.022.
Beale, A.L., P. Meyer, T.H. Marwick, et al. Sex Differences in Cardiovascular Pathophysiology: Why Women Are Overrepresented in Heart Failure With Preserved Ejection Fraction[J]. Circulation, 2018, 138(2):198–205. DOI: https://doi.org/10.1161/circulationaha.118.034271.
Go, A.S., E.M. Hylek, K.A. Phillips, et al. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study[J]. Jama, 2001, 285(18):2370–5. DOI: https://doi.org/10.1001/jama.285.18.2370.
Wu, A.Z., M. Chen, D. Yin, et al. Sex-specific I(KAS) activation in rabbit ventricles with drug-induced QT prolongation[J]. Heart Rhythm, 2021, 18(1):88–97. DOI: https://doi.org/10.1016/j.hrthm.2020.07.020.
Fogli Iseppe, A., H. Ni, S. Zhu, et al. Sex-Specific Classification of Drug-Induced Torsade de Pointes Susceptibility Using Cardiac Simulations and Machine Learning[J]. Clin Pharmacol Ther, 2021, 110(2):380–391. DOI: https://doi.org/10.1002/cpt.2240.
Frommeyer, G., L. Eckardt. Drug-induced proarrhythmia: risk factors and electrophysiological mechanisms[J]. Nat Rev Cardiol, 2016, 13(1):36–47. DOI: https://doi.org/10.1038/nrcardio.2015.110.
Dworatzek, E., I. Baczko, G. Kararigas. Effects of aging on cardiac extracellular matrix in men and women[J]. Proteomics Clin Appl, 2016, 10(1):84–91. DOI: https://doi.org/10.1002/prca.201500031.
Chen, F., M. Du, J.B. Blumberg, et al. Association Among Dietary Supplement Use, Nutrient Intake, and Mortality Among U.S. Adults: A Cohort Study[J]. Ann Intern Med, 2019, 170(9):604–613. DOI: https://doi.org/10.7326/m18-2478.
Acknowledgements: We thank Yuren 930 for allowing the authors to collaborate on this study.
Funding
Funding statement: Not applicable.
Author information
Authors and Affiliations
Contributions
Author contribution: All authors read and approved the final manuscript. Zhen-kang Qiu: Conceptualization, Writing-Review, Editing and Supervision; Jia Wang and Yu-jing Li: Methodology, and Writing of Draft; Xiao-xuan Li, Yu-xin Sun, and Shuai Xiang: Study Design, and Data Curation; Meng-qi Zhang and Xiang-jun Li: Statistical analysis, Supervision, and Validation. All authors contributed to the interpretation of the results and critical revision of the manuscript for important intellectual content and approved the final version of the manuscript. Zhen-kang Qiu is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Conflicts of interest: There are no conflicts of interests of any of the authors.
Ethics approval: The survey protocol was approved by NCHS Ethics Review Board (https://www.cdc.gov/nchs/nhanes/irba98.htm), and all participants have written informed consent.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Wang, J., Li, Yj., Li, XX. et al. Late-Night Overeating and All-Cause and Cardiovascular Disease Mortality in Adults Aged ≥ 50: A Cohort Study. J Nutr Health Aging 27, 701–708 (2023). https://doi.org/10.1007/s12603-023-1966-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-023-1966-1