Abstract
Objectives
There is little evidence in the literature about the relationship between frailty and falls in older adults. Our objective was to explore the relationship between frailty and falls, and to analyze the effect factors (e.g., gender, different frailty assessment tools, areas, level of national economic development, and year of publication) of the association between frailty and falls among older adults.
Design
Systematic review and meta-analysis.
Setting and Participants
Cohort studies that evaluated the association between frailty and falls in the older adults were included. We excluded any literature outside of cohort studies.
Methods
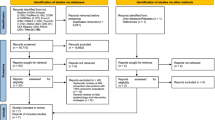
We did a systematic literature search of English databases PubMed, Scopus, Web of Science, EBSCOhost, and SciElO, as well as the Chinese databases CNKI, WANFANG, and VIP from 2001 until October 2022. The eligible studies were evaluated for potential bias using the Newcastle-Ottawa Scale (NOS). Study selection, data extraction and assessment of study quality were each conducted by two investigators. In Stata/MP 17.0 software, we calculated pooled estimates of the prevalence of falls by using a random-effects model, Subgroup analysis was conducted based on gender, different frailty assessment tools, areas, level of economic development, and year of publication. The results are presented using a forest plot.
Results
Twenty-nine studies were included in this meta-analysis and a total of 1,093,270 participants aged 65 years and above were enrolled. Among the older adults, frailty was significantly associated with a higher risk for falls, compared with those without frailty (combined RR-relative risk = 1.48, 95% CI-confidence interval: 1.27–1.73, I2=98.9%). In addition, the results of subgroup analysis indicated that men had a higher risk for falls than women among the older adults with frailty (RR 1.94, 95% CI: 1.18–3.2 versus RR 1.44, 95% CI: 1.24–1.67). Subgroup analysis by different frailty assessment tools revealed an increased risk of falls in older adults with frailty when assessed using the Frailty Phenotype (combined RR 1.32, 95%CI: 1.17–1.48), FRAIL score (combined RR 1.82, 95%CI: 1.36–2.43), and Study of Osteoporotic Fractures index (combined RR 1.54, 95%CI: 1.10–2.16). Furthermore, subgroup analysis by areas and level of national economic development found the highest fall risk in Oceania (combined RR 2.35, 95%CI: 2.28–2.43) and the lowest in Europe (combined RR 1.20, 95%CI: 1.05–1.38). Developed countries exhibited a lower fall risk compared to developing countries (combined RR 1.44, 95%CI: 1.21–1.71). Analysis by year of publication showed the highest fall risk between 2013–2019 (combined RR 1.79, 95%CI: 1.45–2.20) and the lowest between 2001–2013 (combined RR 1.21, 95%CI: 1.13–1.29).
Conclusion
Frailty represents a significant risk factor for falls in older adults, with the degree of risk varying according to the different frailty assessment tools employed, and notably highest when using the FRAIL scale. Additionally, factors such as gender, areas, level of national economic development, and healthcare managers’ understanding of frailty may all impact the correlation between frailty and falls. Thus, it’s imperative to select suitable frailty diagnostic tools tailored to the specific characteristics of the population in question. This, in turn, facilitates the accurate identification of frailty in older adults and informs the development of appropriate preventive and therapeutic strategies to mitigate fall risk.





Similar content being viewed by others
References
Mittelbrunn M, Kroemer G. Hallmarks of T cell aging. Nat Immunol Jun 2021;22(6):687–698. doi: https://doi.org/10.1038/s41590-021-00927-z
Kennedy BK, Berger SL, Brunet A, et al. Geroscience: linking aging to chronic disease. Cell Nov 6 2014;159(4):709–13. doi: https://doi.org/10.1016/j.cell.2014.10.039
Siracuse JJ, Odell DD, Gondek SP, et al. Health care and socioeconomic impact of falls in the elderly. Am J Surg Mar 2012;203(3):335–8; discussion 338. doi: https://doi.org/10.1016/j.amjsurg.2011.09.018
Parry SW, Deary V, Finch T, et al. The STRIDE (Strategies to Increase confidence, InDependence and Energy) study: cognitive behavioural therapy-based intervention to reduce fear of falling in older fallers living in the community - study protocol for a randomised controlled trial. Trials Jun 6 2014;15:210. doi: https://doi.org/10.1186/1745-6215-15-210
Gill TM, Murphy TE, Gahbauer EA, Allore HG. Association of injurious falls with disability outcomes and nursing home admissions in community-living older persons. Am J Epidemiol Aug 1 2013;178(3):418–25. doi: https://doi.org/10.1093/aje/kws554
Kumar A, Carpenter H, Morris R, Iliffe S, Kendrick D. Which factors are associated with fear of falling in community-dwelling older people? Age Ageing Jan 2014;43(1):76–84. doi: https://doi.org/10.1093/ageing/aft154
Kamo T, Takayama K, Ishii H, Suzuki K, Eguchi K, Nishida Y. Coexisting severe frailty and malnutrition predict mortality among the oldest old in nursing homes: A 1-year prospective study. Arch Gerontol Geriatr May–Jun 2017;70:99–104. doi: https://doi.org/10.1016/j.archger.2017.01.009
Chang SF, Lin PL. Frail phenotype and mortality prediction: a systematic review and meta-analysis of prospective cohort studies. Int J Nurs Stud Aug 2015;52(8):1362–74. doi: https://doi.org/10.1016/j.ijnurstu.2015.04.005
Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci Mar 2001;56(3):M146–56. doi: https://doi.org/10.1093/gerona/56.3.m146
Allore HG, Tinetti ME, Gill TM, Peduzzi PN. Experimental designs for multicomponent interventions among persons with multifactorial geriatric syndromes. Clin Trials 2005;2(1):13–21. doi: https://doi.org/10.1191/1740774505cn067oa
Fhon JRS, Rodrigues RAP, Neira WF, Huayta VMR, Robazzi MLdCC. Fall and its association with the frailty syndrome in the elderly: systematic review with meta-analysis. Rev Esc Enferm USP 2016;50(6):1005–1013. doi: https://doi.org/10.1590/s0080-623420160000700018
Cheng MH, Chang SF. Frailty as a Risk Factor for Falls Among Community Dwelling People: Evidence From a Meta-Analysis. J Nurs Scholarsh Sep 2017;49(5):529–536. doi: https://doi.org/10.1111/jnu.12322
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol Sep 2010;25(9):603–5. doi: https://doi.org/10.1007/s10654-010-9491-z
Li Y, Zhang D, Ma Q, Diao Z, Liu S, Shi X. The impact of frailty on prognosis in elderly hemodialysis patients: A prospective cohort study. Clinical Interventions in Aging 2021;16:1659–1667. doi: https://doi.org/10.2147/CIA.S329665
Middleton R, Poveda JL, Orfila Pernas F, et al. Mortality, Falls, and Fracture Risk Are Positively Associated With Frailty: A SIDIAP Cohort Study of 890 000 Patients. J Gerontol A Biol Sci Med Sci Jan 7 2022;77(1):148–154. doi: https://doi.org/10.1093/gerona/glab102
Athuraliya N, Etherton-Beer C. Health in Men Study: Is frailty a predictor of medication-related hospitalization? QJM 2022;115(2):84–90. doi: https://doi.org/10.1093/qjmed/hcaa324
Papachristou E, Wannamethee SG, Lennon LT, et al. Ability of Self-Reported Frailty Components to Predict Incident Disability, Falls, and All-Cause Mortality: Results From a Population-Based Study of Older British Men. Journal of the American Medical Directors Association 2017;18(2):152–157. doi: https://doi.org/10.1016/j.jamda.2016.08.020
Bartosch PS, Kristensson J, McGuigan FE, Akesson KE. Frailty and prediction of recurrent falls over 10 years in a community cohort of 75-year-old women. Aging Clin Exp Res Nov 2020;32(11):2241–2250. doi: https://doi.org/10.1007/s40520-019-01467-1
Ensrud KE, Ewing SK, Cawthon PM, et al. A Comparison of Frailty Indexes for the Prediction of Falls, Disability, Fractures, and Mortality in Older Men. Journal of the American Geriatrics Society Mar 2009;57(3):492–498. doi: https://doi.org/10.1111/j.1532-5415.2009.02137.x
Ensrud KE, Ewing SK, Taylor BC, et al. Comparison of 2 frailty indexes for prediction of falls, disability, fractures, and death in older women. Archives of Internal Medicine Jan 25 2008;168(4):382–389. doi: https://doi.org/10.1001/archinternmed.2007.113
Woods NF, LaCroix AZ, Gray SL, et al. Frailty: emergence and consequences in women aged 65 and older in the Women’s Health Initiative Observational Study. J Am Geriatr Soc Aug 2005;53(8):1321–30. doi: https://doi.org/10.1111/j.1532-5415.2005.53405.x
Jiao J, Guo N, Xie L, et al. Association between Frailty and 90-Day Outcomes amongst the Chinese Population: A Hospital-Based Multicentre Cohort Study. Gerontology 2022;68(1):8–16. doi: https://doi.org/10.1159/000514948
Jung HW, Baek JY, Kwon YH, et al. At-Point Clinical Frailty Scale as a Universal Risk Tool for Older Inpatients in Acute Hospital: A Cohort Study. Frontiers in Medicine 2022;9929555. doi: https://doi.org/10.3389/fmed.2022.929555
Bennett A, Gnjidic D, Gillett M, et al. Prevalence and Impact of Fall-Risk-Increasing Drugs, Polypharmacy, and Drug-Drug Interactions in Robust Versus Frail Hospitalised Falls Patients: A Prospective Cohort Study. Drugs & Aging Mar 2014;31(3):225–232. doi: https://doi.org/10.1007/s40266-013-0151-3
Jarman H, Crouch R, Baxter M, et al. Feasibility and accuracy of ED frailty identification in older trauma patients: a prospective multi-centre study. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine 2021;29(1) 54. doi: https://doi.org/10.1186/s13049-021-00868-4
McEvoy L, Richter M, Chen T, et al. Frailty among older surgical patients and risk of hospital acquired adverse events: The South-Western Sydney frailty and nurse sensitive indicators study. Journal of Clinical Nursing 2022;doi: https://doi.org/10.1111/jocn.16259
Abraham DS, Pham Nguyen TP, Willis AW. Claims-Based Frailty and Outcomes: Applying an Aging Measure to Older Adults with Parkinson’s Disease. Movement Disorders 2021;36(8):1871–1878. doi: https://doi.org/10.1002/mds.28561
Beauchet O, Matskiv J, Launay CP, et al. CARE frailty e-health scale: Association with incident adverse health outcomes and comparison with the Cardiovascular Health Study frailty scale in the NuAge cohort. Maturitas 2022;162:37–43. doi: https://doi.org/10.1016/j.maturitas.2022.04.006
Li JJ, Jiang S, Zhu ML, Liu X, Sun X, Zhao SQ. Comparison of Three Frailty Scales for Prediction of Adverse Outcomes among Older Adults: A Prospective Cohort Study. Journal of Nutrition, Health and Aging 2021;25(4):419–424. doi: https://doi.org/10.1007/s12603-020-1534-x
Doi T, Makizako H, Tsutsumimoto K, et al. Transitional status and modifiable risk of frailty in Japanese older adults: A prospective cohort study. Geriatrics and Gerontology International 2018;18(11):1562–1566. doi: https://doi.org/10.1111/ggi.13525
Samper-Ternent R, Karmarkar A, Graham J, Reistetter T, Ottenbacher K. Frailty as a Predictor of Falls in Older Mexican Americans. Journal of Aging and Health Jun 2012;24(4):641–653. doi: https://doi.org/10.1177/0898264311428490
Sheehan KJ, O’Connell MDL, Cunningham C, Crosby L, Kenny RA. The relationship between increased body mass index and frailty on falls in community dwelling older adults. Bmc Geriatrics Dec 6 2013;13 doi: Artn 132 https://doi.org/10.1186/1471-2318-13-132
Forti P, Rietti E, Pisacane N, Olivelli V, Maltoni B, Ravaglia G. A comparison of frailty indexes for prediction of adverse health outcomes in an elderly cohort. Arch Gerontol Geriatr Jan–Feb 2012;54(1):16–20. doi: https://doi.org/10.1016/j.archger.2011.01.007
Kojima G, Kendrick D, Skelton DA, Morris RW, Gawler S, Iliffe S. Frailty predicts short-term incidence of future falls among British community-dwelling older people: a prospective cohort study nested within a randomised controlled trial. BMC Geriatr Dec 2 2015;15:155. doi: https://doi.org/10.1186/s12877-015-0152-7
Yang F, Wang S, Tan H, et al. A cohort study of the effect of debilitating syndrome on falls in elderly diabetic patients in the community. Chinese Journal of Epidemiology 2018;39(6):776–780. doi: https://doi.org/10.3760/cma.j.issn.0254-6450.2018.06.016
Cai Y, Xu W, Xiao H, Liu H, Chen T. Correlation between Frailty and Adverse Outcomes Among Older Community-Dwelling Chinese Adults: The China Health and Retirement Longitudinal Study. J Nutr Health Aging 2020;24(7):752–757. doi: https://doi.org/10.1007/s12603-020-1368-6
Bilotta C, Nicolini P, Case A, Pina G, Rossi S, Vergani C. Frailty syndrome diagnosed according to the Study of Osteoporotic Fractures (SOF) criteria and adverse health outcomes among community-dwelling older outpatients in Italy. A one-year prospective cohort study. Archives of Gerontology and Geriatrics Mar–Apr 2012;54(2):E23–E28. doi: https://doi.org/10.1016/j.archger.2011.06.037
Grosshauser FJ, Schoene D, Kiesswetter E, Sieber CC, Volkert D. Frailty in Nursing Homes-A Prospective Study Comparing the FRAIL-NH and the Clinical Frailty Scale. J Am Med Dir Assoc Oct 2022;23(10):1717.e1–1717.e8. doi: https://doi.org/10.1016/j.jamda.2022.07.028
Leblanc C, Godaert L, Dramé M, et al. Predictive capacity of the modified SEGA frailty scale upon discharge from geriatric hospitalisation: a six-month prospective study. Geriatr Psychol Neuropsychiatr Vieil Mar 1 2020;18(1):34–41. doi: https://doi.org/10.1684/pnv.2020.0856
Ma L, Tang Z, Chan P, Walston JD. Novel Frailty Screening Questionnaire (FSQ) Predicts 8-Year Mortality in Older Adults in China. Journal of Frailty and Aging 2019;8(1):33–38. doi: https://doi.org/10.14283/jfa.2018.38
Marzetti E, Calvani R, Tosato M, et al. Sarcopenia: an overview. Aging Clin Exp Res Feb 2017;29(1):11–17. doi: https://doi.org/10.1007/s40520-016-0704-5
Marzetti E, Lees HA, Wohlgemuth SE, Leeuwenburgh C. Sarcopenia of aging: underlying cellular mechanisms and protection by calorie restriction. Biofactors Jan–Feb 2009;35(1):28–35. doi: https://doi.org/10.1002/biof.5
Janssen I, Heymsfield SB, Wang ZM, Ross R. Skeletal muscle mass and distribution in 468 men and women aged 18–88 yr. J Appl Physiol (1985) Jul 2000;89(1):81–8. doi: https://doi.org/10.1152/jappl.2000.89.1.81
Morley JE, Malmstrom TK, Miller DK. A simple frailty questionnaire (FRAIL) predicts outcomes in middle aged African Americans. J Nutr Health Aging Jul 2012;16(7):601–8. doi: https://doi.org/10.1007/s12603-012-0084-2
Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci Mar 2001;56(3):M146–56. doi: https://doi.org/10.1093/gerona/56.3.m146
Duong MH, Gnjidic D, McLachlan AJ, Sakiris MA, Goyal P, Hilmer SN. The Prevalence of Adverse Drug Reactions and Adverse Drug Events from Heart Failure Medications in Frail Older Adults: A Systematic Review. Drugs & aging 2022;39(8):631–643. doi: https://doi.org/10.1007/s40266-022-00957-8
Steinman MA, Lee SJ, John Boscardin W, et al. Patterns of multimorbidity in elderly veterans. J Am Geriatr Soc Oct 2012;60(10):1872–80. doi: https://doi.org/10.1111/j.1532-5415.2012.04158.x
Rockwood K, Song X, MacKnight C, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ 2005;173(5):489–495.
Ensrud KE, Palermo L, Black DM, et al. Hip and calcaneal bone loss increase with advancing age: longitudinal results from the study of osteoporotic fractures. J Bone Miner Res Nov 1995;10(11):1778–87. doi: https://doi.org/10.1002/jbmr.5650101122
Feng Z, Lugtenberg M, Franse C, et al. Risk factors and protective factors associated with incident or increase of frailty among community-dwelling older adults: A systematic review of longitudinal studies. PLoS One 2017;12(6):e0178383. doi: https://doi.org/10.1371/journal.pone.0178383
Kwak D, Thompson LV. Frailty: Past, present, and future? Sports Med Health Sci Mar 2021;3(1):1–10. doi: https://doi.org/10.1016/j.smhs.2020.11.005
Whitson HE, Duan-Porter W, Schmader KE, Morey MC, Cohen HJ, Colón-Emeric CS. Physical Resilience in Older Adults: Systematic Review and Development of an Emerging Construct. J Gerontol A Biol Sci Med Sci Apr 2016;71(4):489–95. doi: https://doi.org/10.1093/gerona/glv202
Reid KF, Fielding RA. Skeletal muscle power: a critical determinant of physical functioning in older adults. Exerc Sport Sci Rev Jan 2012;40(1):4–12. doi: https://doi.org/10.1097/JES.0b013e31823b5f13
Stulp G, Barrett L. Evolutionary perspectives on human height variation. Biol Rev Camb Philos Soc Feb 2016;91(1):206–34. doi: https://doi.org/10.1111/brv.12165
Mackenbach JP. Politics is nothing but medicine at a larger scale: reflections on public health’s biggest idea. J Epidemiol Community Health Mar 2009;63(3):181–4. doi: https://doi.org/10.1136/jech.2008.077032
Bambra C, Pope D, Swami V, et al. Gender, health inequalities and welfare state regimes: a cross-national study of 13 European countries. J Epidemiol Community Health Jan 2009;63(1):38–44. doi: https://doi.org/10.1136/jech.2007.070292
McKay J. Economic development and its influences and risks for nutrition, cuisine and health. Asia Pac J Clin Nutr 2004;13(2):171–7.
Zijlstra GA, van Haastregt JC, van Rossum E, van Eijk JT, Yardley L, Kempen GI. Interventions to reduce fear of falling in community-living older people: a systematic review. J Am Geriatr Soc Apr 2007;55(4):603–15. doi: https://doi.org/10.1111/j.1532-5415.2007.01148.x
Morley JE, Vellas B, van Kan GA, et al. Frailty consensus: a call to action. J Am Med Dir Assoc Jun 2013;14(6):392–7. doi: https://doi.org/10.1016/j.jamda.2013.03.022
Hoogendijk EO, Afilalo J, Ensrud KE, Kowal P, Onder G, Fried LP. Frailty: implications for clinical practice and public health. Lancet Oct 12 2019;394(10206):1365–1375. doi: https://doi.org/10.1016/s0140-6736(19)31786-6
Author information
Authors and Affiliations
Contributions
Author Contributions: Zhi-cheng Yang contributed to the performance of the study, analyzed and interpreted the data, and wrote the manuscript. Gui-hua Jiang contributed to the study’s performance and data interpretation; Ying-hong Chu and Ji-hong Gao contributed to the data analysis; He Lin and Zhou-jie Tong contributed to manuscript revision.
Corresponding author
Additional information
Conflicts of Interest: The authors declare no conflict of interest.
Ethical standards: This meta-analysis followed PRISMA guidelines and used data from previously published articles. No primary data collection involving humans or animals was conducted. Research methods and data analysis were performed transparently and rigorously.
Financial support: This work was funded by the research grants from Clinical Research Center of Shandong University (No.2020SDUCRCC027), Taishan Scholars (No. tsqn202103146), the National Natural Science Foundation of China (82070392, 81702194, 81801953), Key research and development program of Shandong Province (2019GSF108041).
Rights and permissions
About this article
Cite this article
Yang, ZC., Lin, H., Jiang, GH. et al. Frailty Is a Risk Factor for Falls in the Older Adults: A Systematic Review and Meta-Analysis. J Nutr Health Aging 27, 487–495 (2023). https://doi.org/10.1007/s12603-023-1935-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-023-1935-8