Abstract
Objectives
This study aimed to determine the changing prevalence of five chronic non-communicable diseases (NCDs)- hypertension, coronary heart disease (CHD), stroke, chronic obstructive pulmonary disease (COPD), and asthma— and its multimorbidity (refers to the co-existence of two or more chronic diseases in an individual) across socioeconomic spectra in rural southwest China.
Measurements
Two cross-sectional health interviews and examination surveys were conducted among individuals aged ≥35 years in rural China. An individual socioeconomic position (SEP) index was constructed using principal component analysis. Anthropometric measurements, blood pressure, and post-bronchodilator spirometry tests were recorded for each participant.
Results
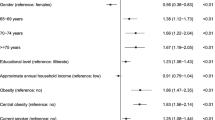
The mean age and proportion of men was 56.1 years and 48.4% in 2011, while was 56.6 years and 49.4% in 2021. From 2011 to 2021, the overall prevalence of hypertension, stroke and COPD increased from 26.1%, 1.1%, and 8.7% to 40.4%, 2.4%, and 12.8%, respectively (P < 0.01), while prevalence of CHD (2.1% vs. 2.2%) and asthma (1.4% vs. 1.5%) did not differ between the two study years (P > 0.05). The prevalence of NCDs multimorbidity increased from 2.3% to 9.7%, and was also observed among subgroups categorized by sex, age, ethnicity, level of education, income, and SEP (P < 0.01). In addition, the relative increases in the prevalence of multimorbidity were greater among men, old individuals, ethnic minorities, and those with low level of education and low SEP. Both in 2011 and 2021, ethnic minorities and individuals with lower level of education and low SEP had a higher prevalence of multimorbidity of the five studied chronic NCDs than their counterparts (P <0.01).
Conclusions
The prevalence of NCDs multimorbidity increased substantially across all socioeconomic gradients in rural southwest China. Future interventions to further manage NCDs and their multimorbidity must be tailored to address socioeconomic factors.
Similar content being viewed by others
References
Global Burden of Disease Collaborative Network, Global Burden of Disease Study 2019 (GBD 2019) Results (2020, Institute for Health Metrics and Evaluation–IHME) https://vizhub.healthdata.org/gbd-results/.
Wagner KH, Brath H. A global view on the development of non-communicable diseases. Prev Med. 2012; 54 Suppl:S38–41. https://doi.org/10.1016/j.ypmed.2011.11.012.
Muka T, Imo D, Jaspers L, et al. The global impact of non-communicable diseases on healthcare spending and national income: a systematic review. Eur J Epidemiol. 2015;30(4):251–77. https://doi.org/10.1007/s10654-014-9984-2.
Zhang X, Pan T, McPake B. Re-examining the reversal hypothesis: A nationwide population-based study of the association between socioeconomic status, and NCDs and risk factors in China. SSM Popul Health. 2023; 21:101335. https://doi.org/10.1016/j.ssmph.2022.101335.
Ma S, Yang L, Zhao M, et al. Trends in hypertension prevalence, awareness, treatment and control rates among Chinese adults, 1991–2015. J Hypertens. 2021;39(4):740–748. https://doi.org/10.1097/hjh.0000000000002698.
Chan KY, Li X, Chen W, et al. Prevalence of chronic obstructive pulmonary disease (COPD) in China in 1990 and 2010. J Glob Health. 2017;7(2):020704. https://doi.org/10.7189/jogh.07.020704.
Tu WJ, Hua Y, Yan F, et al. Prevalence of stroke in China, 2013–2019: A population-based study. Lancet Reg Health West Pac. 2022; 28:100550. https://doi.org/10.1016/j.lanwpc.2022.100550.
Asogwa OA, Boateng D, Marza-Florensa A, et al. Multimorbidity of non-communicable diseases in low-income and middle-income countries: a systematic review and meta-analysis. BMJ Open. 2022;12(1):e049133. https://doi.org/10.1136/bmjopen-2021-049133.
Sun ZJ, Fan JN, Yu CQ, et al. [Prevalence, patterns and long-term changes of multimorbidity in adults from 10 regions of China]. Zhonghua Liu Xing Bing Xue Za Zhi. 2021;42(5):755–762. https://doi.org/10.3760/cma.j.cn112338-20200305-00259.
Linetzky B, De Maio F, Ferrante D, et al. Sex-stratified socio-economic gradients in physical inactivity, obesity, and diabetes: evidence of short-term changes in Argentina. International journal of public health. 2013; 58:277–84. https://doi.org/10.1007/s00038-012-0371-z.
Violan C, Foguet-Boreu Q, Flores-Mateo G, et al. Prevalence, determinants and patterns of multimorbidity in primary care: a systematic review of observational studies. PLoS One. 2014;9(7):e102149. https://doi.org/10.1371/journal.pone.0102149.
Pickering TG, Hall JE, Appel LJ, et al. Recommendations for blood pressure measurement in humans and experimental animals: part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Circulation. 2005;47(299–310):1524–4539. (Electronic).
Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. The European respiratory journal. 2005; 26:319–38. https://doi.org/10.1183/09031936.05.00034805.
WHO/LASA/IOTF. The Asia Pacific perspective: redefining obesity and its treatment. Melbourne, Australia: Health Communications Australia Pty Ltd;2000.
Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease (2017 report). https://goldcopd.org/%20gold-2017-global-strategy-diagnosis-management-prevention-copd/.
Wang C, Xu J, Yang L, et al. Prevalence and risk factors of chronic obstructive pulmonary disease in China (the China Pulmonary Health [CPH] study): a national cross-sectional study. Lancet. 2018;391(10131):1706–1717. https://doi.org/10.1016/s0140-6736(18)30841-9.
Roy A, Praveen PA, Amarchand R, et al. Changes in hypertension prevalence, awareness, treatment and control rates over 20 years in National Capital Region of India: results from a repeat cross-sectional study. BMJ Open. 2017;7(7):e015639. https://doi.org/10.1136/bmjopen-2016-015639.
India State-Level Disease Burden Initiative CRDC. The burden of chronic respiratory diseases and their heterogeneity across the states of India: the Global Burden of Disease Study 1990–2016. Lancet Glob Health. 2018;6(12):e1363–e1374. https://doi.org/10.1016/s2214-109x(18)30409-1.
Wang Y, Li Y, Liu X, et al. Prevalence and Influencing Factors of Coronary Heart Disease and Stroke in Chinese Rural Adults: The Henan Rural Cohort Study. Front Public Health. 2019; 7:411. https://doi.org/10.3389/fpubh.2019.00411.
Wan J, Zhang Q, Li C, et al. Prevalence of and risk factors for asthma among people aged 45 and older in China: a cross-sectional study. BMC Pulm Med. 2021;21(1):311. https://doi.org/10.1186/s12890-021-01664-7.
Teh JK, Tey NP, Ng ST. Ethnic and gender differentials in non-communicable diseases and self-rated health in Malaysia. PLoS One. 2014;9(3):e91328. https://doi.org/10.1371/journal.pone.0091328.
Ezejimofor MC, Chen YF, Kandala NB, et al. Stroke survivors in low- and middle-income countries: A meta-analysis of prevalence and secular trends. J Neurol Sci. 2016; 364:68–76. https://doi.org/10.1016/j.jns.2016.03.016.
Ta Y, Zhu Y, Fu H. Trends in access to health services, financial protection and satisfaction between 2010 and 2016: Has China achieved the goals of its health system reform? Soc Sci Med. 2020;245:112715. https://doi.org/10.1016/j.socscimed.2019.112715.
Abebe F, Schneider M, Asrat B, et al. Multimorbidity of chronic non-communicable diseases in low- and middle-income countries: A scoping review. J Comorb. 2020; 10:2235042X20961919. https://doi.org/10.1177/2235042x20961919.
Geng Y, Jie W, He Y, et al. Prevalence and Patterns of Multimorbidity Among Adults Aged 18 Years and Older - China, 2018. China CDC weekly. 2023; 5(2):35–39. https://doi.org/10.46234/ccdcw2023.007.
Tetzlaff J, Epping J, Sperlich S, et al. Widening inequalities in multimorbidity? Time trends among the working population between 2005 and 2015 based on German health insurance data. Int J Equity Health. 2018;17(1):103. https://doi.org/10.1186/s12939-018-0815-z.
Caraballo C, Herrin J, Mahajan S, et al. Temporal Trends in Racial and Ethnic Disparities in Multimorbidity Prevalence in the United States, 1999–2018. Am J Med. 2022; 135(9):1083–1092.e14. https://doi.org/10.1016/j.amjmed.2022.04.010.
Singer L, Green M, Rowe F, et al. Trends in multimorbidity, complex multimorbidity and multiple functional limitations in the ageing population of England, 2002–2015. Journal of Comorbidity. 2019; 9:2235042X19872030. https://doi.org/10.1177/2235042x19872030.
Zhang Q, Ruan Y, Hu W, et al. Perceived social support and diet quality among ethnic minority groups in Yunnan Province, Southwestern China: a cross-sectional study. BMC Public Health. 2021;21(1):1726. https://doi.org/10.1186/s12889-021-11787-5.
Hui-Fang L, Cai L, Wang XM, et al. Ethnic disparities in prevalence and clustering of cardiovascular disease risk factors in rural Southwest China. BMC Cardiovasc Disord. 2019;19(1):200. https://doi.org/10.1186/s12872-019-1185-1.
Pathirana TI, Jackson CA. Socioeconomic status and multimorbidity: a systematic review and meta-analysis. Aust N Z J Public Health. 2018;42(2):186–194. https://doi.org/10.1111/1753-6405.12762.
Allen L, Williams J, Townsend N, et al. Socioeconomic status and non-communicable disease behavioural risk factors in low-income and lower-middle-income countries: a systematic review. Lancet Glob Health. 2017;5(3):e277–e289. https://doi.org/10.1016/S2214-109X(17)30058-X.
Acknowledgement
This study was supported by grants from the National Natural Science Foundation of China (72064026 and 82160165), Yunnan Provincial Philosophy and Social Science Innovative Research Team (2023CX11), Program for Innovative Research Team of Yunnan Province (202005AE160002), the Young and Middle-aged Academic and Technical Leaders Reserve Talented Person Project in Yunnan (202105AC160093), and the Training Plan for Medical Discipline Leaders of Yunnan Provincial Health and Family Planning Commission (d-2017039).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The Kunming Medical University Ethics Committee approved this study prior to beginning research. Written informed consent was obtained from all participants in the study, and the Ethics Committee of Kunming Medical University approved the consent procedure. This study was performed in accordance with the Declaration of Helsinki.
Additional information
Conflict of Interest statement
The authors declare that there are no conflicts of interest.
Electronic Supplementary Material
Rights and permissions
About this article
Cite this article
Liu, L., Wu, X., Li, HF. et al. Trends in the Prevalence of Chronic Non-Communicable Diseases and Multimorbidity across Socioeconomic Gradients in Rural Southwest China. J Nutr Health Aging 27, 457–462 (2023). https://doi.org/10.1007/s12603-023-1932-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-023-1932-y