Abstract
Objectives
This study aims to assess the effectiveness of a multidomain intervention program on the change in functional status of hospitalized older adults.
Design
This single-arm, prospective, non-randomized interventional study investigates the efficacy of a multidomain interventional program including cognitive stimulation activity, simple exercises, frailty education, and nutrition counseling.
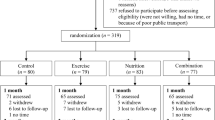
Setting and Participants
At a tertiary hospital in southern Taiwan, 352 eligible patients were sequentially enrolled. Included patients were aged ≥65 years (mean age, 79.6 ± 9.0 years; 62% male), scored 3–7 on the Clinical Frailty Scale (CFS), and were hospitalized in the geriatric acute ward.
Intervention
Those receiving standard care (physical rehabilitation and nutrition counseling) during January–July 2019 composed the historical control group. Those receiving the multidomain intervention during August–December 2019 composed the intervention group.
Measurements
The primary outcome was the change in activities of daily life (ADL) and frailty status, as assessed by Katz Index and Clinical Frailty Scale, with using the generalized estimating equation model. The length of hospital stay, medical costs, and re-admission rates were secondary outcomes.
Results
Participants undergoing intervention (n = 101; 27.9%) showed greater improvements in the ADL and CFS during hospitalization (ADL adjusted estimate, 0.61; 95% CI, 0.11–1.11; p = 0.02; CFS adjusted estimate, −1.11; 95% CI, −1.42–−0.80; p < 0.01), shorter length of hospital stay (adjusted estimate, -5.00; 95% CI, −7.99–−2.47; p < 0.01), lower medical costs (adjusted estimate, 0.58; 95% CI, 0.49–0.69; p < 0.01), and lower 30- and 90-day readmission rates (30-day adjusted OR [aOR], 0.12; 95% CI, 0.27–0.50; p < 0.01; 60-day aOR, 0.04; 95% CI, 0.01–0.33; p < 0.01) than did controls.
Conclusions
Participation in the multidomain intervention program during hospitalization improved the functional status and decreased the hospital stay length, medical costs, and readmission rates of frail older people.


Similar content being viewed by others
References
Loyd C, Markland AD, Zhang Y, Fowler M, Harper S, Wright NC, et al. Prevalence of Hospital-Associated Disability in Older Adults: A Meta-analysis. Journal of the American Medical Directors Association. 2020;21(4):455–61.e5. doi:https://doi.org/10.1016/j.jamda.2019.09.015
Gill TM, Gahbauer EA, Han L, Allore HG. The role of intervening hospital admissions on trajectories of disability in the last year of life: prospective cohort study of older people. BMJ (Clinical research ed). 2015;350:h2361. doi:https://doi.org/10.1136/bmj.h2361
Covinsky KE, Pierluissi E, Johnston CB. Hospitalization-associated disability: “She was probably able to ambulate, but I’m not sure”. Jama. 2011;306(16):1782–93. doi:https://doi.org/10.1001/jama.2011.1556
Gill TM, Allore HG, Gahbauer EA, Murphy TE. Change in disability after hospitalization or restricted activity in older persons. Jama. 2010;304(17):1919–28. doi:https://doi.org/10.1001/jama.2010.1568
Boyd CM, Landefeld CS, Counsell SR, Palmer RM, Fortinsky RH, Kresevic D, Burant C, Covinsky KE. Recovery of activities of daily living in older adults after hospitalization for acute medical illness. J Am Geriatr Soc. 2008;56(12):2171–9. doi:https://doi.org/10.1111/j.1532-5415.2008.02023.x
Dharmarajan K, Han L, Gahbauer EA, Leo-Summers LS, Gill TM. Disability and Recovery After Hospitalization for Medical Illness Among Community-Living Older Persons: A Prospective Cohort Study. J Am Geriatr Soc. 2020;68(3):486–95. doi:https://doi.org/10.1111/jgs.16350
Gilbert T, Neuburger J, Kraindler J, Keeble E, Smith P, Ariti C, et al. Development and validation of a Hospital Frailty Risk Score focusing on older people in acute care settings using electronic hospital records: an observational study. Lancet. 2018;391(10132):1775–82. doi:https://doi.org/10.1016/s0140-6736(18)30668-8
Martinez-Velilla N, Herrero AC, Cadore EL, Saez de Asteasu ML, Izquierdo M. Iatrogenic Nosocomial Disability Diagnosis and Prevention. J Am Med Dir Assoc. 2016;17(8):762–4. doi:https://doi.org/10.1016/j.jamda.2016.05.019
Gill TM, Allore HG, Holford TR, Guo Z. Hospitalization, restricted activity, and the development of disability among older persons. Jama. 2004;292(17):2115–24. doi:https://doi.org/10.1001/jama.292.17.2115
Cunha AIL, Veronese N, de Melo Borges S, Ricci NA. Frailty as a predictor of adverse outcomes in hospitalized older adults: A systematic review and meta-analysis. Ageing research reviews. 2019;56:100960. doi:https://doi.org/10.1016/j.arr.2019.100960
Davenport C, Stetzer RJ. Prevention of Hazards of Hospitalization. In: Chun A, editor. Geriatric Practice: A Competency Based Approach to Caring for Older Adults. Cham: Springer International Publishing; 2020. p. 425–40.
Ng TP, Feng L, Nyunt MS, Feng L, Niti M, Tan BY, et al. Nutritional, Physical, Cognitive, and Combination Interventions and Frailty Reversal Among Older Adults: A Randomized Controlled Trial. The American journal of medicine. 2015;128(11):1225–36.e1. doi:https://doi.org/10.1016/j.amjmed.2015.06.017
Hsu C-C, Yu P-C, Lin M-H, Peng L-N, Chen L-K. Early Geriatric Evaluation and Management Services Reduced In-Hospital Mortality Risk among Frail Oldest-Old Patients. Aging Medicine and Healthcare. 2021;12(2):62–7. doi:https://doi.org/10.33879/AMH.122.2020.12046
Kosse NM, Dutmer AL, Dasenbrock L, Bauer JM, Lamoth CJ. Effectiveness and feasibility of early physical rehabilitation programs for geriatric hospitalized patients: a systematic review. BMC geriatrics. 2013;13:107. doi:https://doi.org/10.1186/1471-2318-13-107
Martinez-Velilla N, Cadore EL, Casas-Herrero A, Idoate-Saralegui F, Izquierdo M. Physical Activity and Early Rehabilitation in Hospitalized Elderly Medical Patients: Systematic Review of Randomized Clinical Trials. J Nutr Health Aging. 2016;20(7):738–51. doi:https://doi.org/10.1007/s12603-016-0683-4
Fossat G, Baudin F, Courtes L, Bobet S, Dupont A, Bretagnol A, et al. Effect of In-Bed Leg Cycling and Electrical Stimulation of the Quadriceps on Global Muscle Strength in Critically Ill Adults: A Randomized Clinical Trial. Jama. 2018;320(4):368–78. doi:https://doi.org/10.1001/jama.2018.9592
Martinez-Velilla N, Casas-Herrero A, Zambom-Ferraresi F, Saez de Asteasu ML, Lucia A, Galbete A, et al. Effect of Exercise Intervention on Functional Decline in Very Elderly Patients During Acute Hospitalization: A Randomized Clinical Trial. JAMA internal medicine. 2019;179(1):28–36. doi:https://doi.org/10.1001/jamainternmed.2018.4869
Ortiz-Alonso J, Bustamante-Ara N, Valenzuela PL, Vidán-Astiz M, Rodríguez-Romo G, Mayordomo-Cava J, et al. Effect of a Simple Exercise Program on Hospitalization-Associated Disability in Older Patients: A Randomized Controlled Trial. Journal of the American Medical Directors Association. 2020;21(4):531–7.e1. doi:https://doi.org/10.1016/j.jamda.2019.11.027
Guerville F, de Souto Barreto P, Giudici KV, Rolland Y, Vellas B. Association of 3-Year Multidomain Intervention and Omega-3 Supplementation with Frailty Incidence. J Am Geriatr Soc. 2019;67(8):1700–6. doi:https://doi.org/10.1111/jgs.15994
Puts MTE, Toubasi S, Andrew MK, Ashe MC, Ploeg J, Atkinson E, et al. Interventions to prevent or reduce the level of frailty in community-dwelling older adults: a scoping review of the literature and international policies. Age and ageing. 2017;46(3):383–92. doi:https://doi.org/10.1093/ageing/afw247
Chen LK, Hwang AC, Lee WJ, Peng LN, Lin MH, Neil DL, Shih SF, Loh CH, Chiou ST, Taiwan Health Promotion Intervention Study for Elders research g. Efficacy of multidomain interventions to improve physical frailty, depression and cognition: data from cluster-randomized controlled trials. Journal of cachexia, sarcopenia and muscle. 2020. doi:https://doi.org/10.1002/jcsm.12534
Harris D, Haboubi N. Malnutrition screening in the elderly population. J R Soc Med. 2005;98(9):411–4. doi:https://doi.org/10.1258/jrsm.98.9.411
Kisner C, and Lynn Allen Colby. Therapeutic Exercise: Foundations and Techniques. 7 ed. Philadelphia: F.A. Davis; 1996. 960 p.
Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of Illness in the Aged. The Index of Adl: A Standardized Measure of Biological and Psychosocial Function. Jama. 1963;185:914–9.
Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I, Mitnitski A. A global clinical measure of fitness and frailty in elderly people. Cmaj. 2005;173(5):489–95. doi:https://doi.org/10.1503/cmaj.050051
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. Journal of chronic diseases. 1987;40(5):373–83.
Functional outcomes for clinical trials in frail older persons: time to be moving. J Gerontol A Biol Sci Med Sci. 2008;63(2):160–4. doi:https://doi.org/10.1093/gerona/63.2.160
Heldmann P, Werner C, Belala N, Bauer JM, Hauer K. Early inpatient rehabilitation for acutely hospitalized older patients: a systematic review of outcome measures. BMC geriatrics. 2019;19(1):189. doi:https://doi.org/10.1186/s12877-019-1201-4
Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet. 2013;381(9868):752–62. doi:https://doi.org/10.1016/s0140-6736(12)62167-9
Cesari M, Prince M, Thiyagarajan JA, De Carvalho IA, Bernabei R, Chan P, et al. Frailty: An Emerging Public Health Priority. J Am Med Dir Assoc. 2016;17(3):188–92. doi:https://doi.org/10.1016/j.jamda.2015.12.016
Oh G, Lee H, Park CM, Jung HW, Lee E, Jang IY, Guralnik JM, Kim DH. Long-term effect of a 24-week multicomponent intervention on physical performance and frailty in community-dwelling older adults. Age Ageing. 2021;50(6):2157–66. doi:https://doi.org/10.1093/ageing/afab149
Theou O, Squires E, Mallery K, Lee JS, Fay S, Goldstein J, Armstrong JJ, Rockwood K. What do we know about frailty in the acute care setting? A scoping review. BMC geriatrics. 2018;18(1):139. doi:https://doi.org/10.1186/s12877-018-0823-2
Valenzuela PL, Morales JS, Pareja-Galeano H, Izquierdo M, Emanuele E, de la Villa P, Lucia A. Physical strategies to prevent disuse-induced functional decline in the elderly. Ageing research reviews. 2018;47:80–8. doi:https://doi.org/10.1016/j.arr.2018.07.003
Rezaei-Shahsavarloo Z, Atashzadeh-Shoorideh F, Gobbens RJJ, Ebadi A, Ghaedamini Harouni G. The impact of interventions on management of frailty in hospitalized frail older adults: a systematic review and meta-analysis. BMC geriatrics. 2020;20(1):526. doi:https://doi.org/10.1186/s12877-020-01935-8
Chen CC, Chen CN, Lai IR, Huang GH, Saczynski JS, Inouye SK. Effects of a modified Hospital Elder Life Program on frailty in individuals undergoing major elective abdominal surgery. J Am Geriatr Soc. 2014;62(2):261–8. doi:https://doi.org/10.1111/jgs.12651
Ekerstad N, Dahlin Ivanoff S, Landahl S, Östberg G, Johansson M, Andersson D, Husberg M, Alwin J, Karlson BW. Acute care of severely frail elderly patients in a CGA-unit is associated with less functional decline than conventional acute care. Clin Interv Aging. 2017;12:1239–49. doi:https://doi.org/10.2147/cia.S139230
Braun T, Grüneberg C, Süßmilch K, Wiessmeier M, Schwenk I, Eggert S, Machleit-Ebner A, Harras I, Thiel C. An augmented prescribed exercise program (APEP) to improve mobility of older acute medical patients - a randomized, controlled pilot and feasibility trial. BMC geriatrics. 2019;19(1):240. doi:https://doi.org/10.1186/s12877-019-1246-4
Church S, Rogers E, Rockwood K, Theou O. A scoping review of the Clinical Frailty Scale. BMC geriatrics. 2020;20(1):393. doi:https://doi.org/10.1186/s12877-020-01801-7
Xu W, Li YX, Hu Y, Wu C. Association of Frailty with recovery from disability among community-dwelling Chinese older adults: China health and retirement longitudinal study. BMC geriatrics. 2020;20(1):119. doi:https://doi.org/10.1186/s12877-020-01519-6
Chang HC, Lu YY, Kao SL. Association of frailty and functional recovery in an Acute Care for Elders unit: a prospective observational study. BMC geriatrics. 2022;22(1):608. doi:https://doi.org/10.1186/s12877-022-03290-2
Kidd T, Mold F, Jones C, Ream E, Grosvenor W, Sund-Levander M, Tingström P, Carey N. What are the most effective interventions to improve physical performance in pre-frail and frail adults? A systematic review of randomised control trials. BMC geriatrics. 2019;19(1):184. doi:https://doi.org/10.1186/s12877-019-1196-x
Scheerman K, Raaijmakers K, Otten RHJ, Meskers CGM, Maier AB. Effect of physical interventions on physical performance and physical activity in older patients during hospitalization: a systematic review. BMC geriatrics. 2018;18(1):288. doi:https://doi.org/10.1186/s12877-018-0965-2
Carneiro MAS, Franco CMC, Silva AL, Castro ESP, Kunevaliki G, Izquierdo M, Cyrino ES, Padilha CS. Resistance exercise intervention on muscular strength and power, and functional capacity in acute hospitalized older adults: a systematic review and meta-analysis of 2498 patients in 7 randomized clinical trials. Geroscience. 2021;43(6):2693–705. doi:https://doi.org/10.1007/s11357-021-00446-7
Lee W-J, Peng L-N, Lin C-H, Chen R-C, Lin S-Z, Loh C-H, et al. Effects of incorporating multidomain interventions into integrated primary care on quality of life: a randomised controlled trial. The Lancet Healthy Longevity. 2021;2(11):e712–e23. doi:https://doi.org/10.1016/S2666-7568(21)00248-8
Ng TP, Feng L, Nyunt MS, Feng L, Niti M, Tan BY, et al. Nutritional, Physical, Cognitive, and Combination Interventions and Frailty Reversal Among Older Adults: A Randomized Controlled Trial. The American journal of medicine. 2015;128(11):1225–36e1. doi:https://doi.org/10.1016/j.amjmed.2015.06.017
Pahor M, Blair SN, Espeland M, Fielding R, Gill TM, Guralnik JM, et al. Effects of a physical activity intervention on measures of physical performance: Results of the lifestyle interventions and independence for Elders Pilot (LIFE-P) study. J Gerontol A Biol Sci Med Sci. 2006;61(11):1157–65. doi:https://doi.org/10.1093/gerona/61.11.1157
Serra-Prat M, Sist X, Domenich R, Jurado L, Saiz A, Roces A, Palomera E, Tarradelles M, Papiol M. Effectiveness of an intervention to prevent frailty in pre-frail community-dwelling older people consulting in primary care: a randomised controlled trial. Age Ageing. 2017;46(3):401–7. doi:https://doi.org/10.1093/ageing/afw242
Chia-Hui Chen C, Yang YT, Lai IR, Lin BR, Yang CY, Huang J, et al. Three Nurse-administered Protocols Reduce Nutritional Decline and Frailty in Older Gastrointestinal Surgery Patients: A Cluster Randomized Trial. J Am Med Dir Assoc. 2019;20(5):524–9.e3. doi:https://doi.org/10.1016/j.jamda.2018.09.016
Wang YY, Yue JR, Xie DM, Carter P, Li QL, Gartaganis SL, Chen J, Inouye SK. Effect of the Tailored, Family-Involved Hospital Elder Life Program on Postoperative Delirium and Function in Older Adults: A Randomized Clinical Trial. JAMA internal medicine. 2020;180(1):17–25. doi:https://doi.org/10.1001/jamainternmed.2019.4446
Brown CJ, Foley KT, Lowman JD, Jr., MacLennan PA, Razjouyan J, Najafi B, Locher J, Allman RM. Comparison of Posthospitalization Function and Community Mobility in Hospital Mobility Program and Usual Care Patients: A Randomized Clinical Trial. JAMA internal medicine. 2016;176(7):921–7. doi:https://doi.org/10.1001/jamainternmed.2016.1870
Braet A, Weltens C, Sermeus W. Effectiveness of discharge interventions from hospital to home on hospital readmissions: a systematic review. JBI database of systematic reviews and implementation reports. 2016;14(2):106–73. doi:https://doi.org/10.11124/jbisrir-2016-2381
Tzeng HM, Yin CY. Family involvement in inpatient care in Taiwan. Clinical nursing research. 2008;17(4):297–311. doi:https://doi.org/10.1177/1054773808324655
Siebens H, Aronow H, Edwards D, Ghasemi Z. A randomized controlled trial of exercise to improve outcomes of acute hospitalization in older adults. J Am Geriatr Soc. 2000;48(12):1545–52. doi:https://doi.org/10.1111/j.1532-5415.2000.tb03862.x
Acknowledgements
The authors would like to thank all colleagues who contributed to this study and the personnel at the Cancer Center, Department of Medical Education and Research, and Research Center of Medical Informatics of Kaohsiung Veterans General Hospital for providing information in response to inquiries and assistance in data processing; Shih-Tsung Huang from Graduate Institute of Clinical Pharmacy, College of Medicine, National Taiwan University, and Department of Medical Education and Research, Kaohsiung Veterans General Hospital, Kaohsiung, Taiwan for full assistance in statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Additional information
Conflict of interest: To the best of our knowledge, the named authors have no potential conflict of interest including financial, intellectual property and personal conflicts.
Ethical standards: The authors declare that the study procedures comply with current ethical standards for research involving human participants in Taiwan and follows the principles outlined in the Declaration of Helsinki. The study was approved by the Clinical Research Ethics Committee of the Kaohsiung Veterans General Hospital(KSVGH20-CT9-07). Because this protocol met the waivers of informed consent guidelines, the Institutional Review Board agreed the request to waive the documentation of informed consent.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Wang, YC., Liang, CK., Chou, MH. et al. The Effectiveness of Frailty Intervention for Older Patients with Frailty during Hospitalization. J Nutr Health Aging 27, 413–420 (2023). https://doi.org/10.1007/s12603-023-1924-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-023-1924-y