Abstract
Objectives
The relationship of dietary iron intake with the risk of hypertension remains uncertain. We aimed to investigate the prospective association between dietary iron intake and new-onset hypertension among Chinese adults.
Design
A nationwide cohort study.
Setting
Using data from seven rounds of the China Health and Nutrition Survey (CHNS) from 1997 to 2015.
Participants
A total of 12,245 participants without hypertension at baseline were included in this study.
Exposures
Dietary intake was measured by three consecutive 24-h dietary recalls combined with a household weighing inventory.
Measurements
The study outcome was new-onset hypertension, defined as systolic blood pressure ≥140 mmHg and/or diastolic blood pressure ≥90 mmHg or diagnosed by physician or currently under antihypertensive treatment during the follow-up.
Results
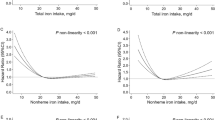
During a median follow-up of 6.1 years, 4,304 (35.1%) participants developed hypertension. Overall, there was a U-shaped association between dietary total iron intake and new-onset hypertension (P for nonlinearity <0.001), with the lowest risk observed at 18.2–<22.1 mg/day (quintile 2–3). Similarly, a U-shaped association between dietary nonheme iron intake and new-onset hypertension was found (P for nonlinearity <0.001), with the lowest risk at 17.4–<21.3 mg/day (quintile 2–3). However, the association between dietary heme iron intake and new-onset hypertension followed a L-shape (P for nonlinearity <0.001), and a significantly lower risk of new-onset hypertension was found in participants with quintile 2–5 of dietary heme iron intake (adjusted HR, 0.75; 95% CI: 0.68, 0.82), compared with those in quintile 1 (<0.25 mg/day).
Conclusions
The association between dietary iron and new-onset hypertension was nonlinear in Chinese adults, following a U-shape for total or nonheme iron intake, and a L-shape for heme iron intake.


Similar content being viewed by others
References
Mills KT, Stefanescu A, He J. The global epidemiology of hypertension. Nat Rev Nephrol. 2020; 16:223–237. doi:https://doi.org/10.1038/s41581-019-0244-2
Li Y, Yang L, Wang L, et al. Burden of hypertension in China: a nationally representative survey of 174,621 adults. Int J Cardiol. 2017; 227:516–523. doi:https://doi.org/10.1016/j.ijcard.2016.10.110
Zhang Y, Nie J, Zhang Y, et al. Degree of Blood Pressure Control and Incident Diabetes Mellitus in Chinese Adults With Hypertension. J Am Heart Assoc. 2020; 9: e017015. doi: https://doi.org/10.1161/JAHA.120.017015
Lewington S, Lacey B, Clarke R, et al. The burden of hypertension and associated risk for cardiovascular mortality in China. JAMA Intern Med. 2016; 176:524. doi:https://doi.org/10.1001/jamainternmed.2016.0190.
Mohammadifard N, Humphries KH, Gotay C, et al. Trace minerals intake: risks and benefits for cardiovascular health. Crit Rev Food Sci Nutr. 2019; 59:1334–1346. doi:https://doi.org/10.1080/10408398.2017.1406332.
Papanikolaou G, Pantopoulos K. Iron metabolism and toxicity. Toxicol Appl Pharm. 2005; 202:199–211. doi:https://doi.org/10.1016/j.taap.2004.06.021.
von Drygalski A, Adamson JW. Iron metabolism in man. JPEN J Parenter Enteral Nutr. 2013; 37:599–606. doi: https://doi.org/10.1177/0148607112459648.
Zhang H, Zhabyeyev P, Wang S, Oudit GY. Role of iron metabolism in heart failure: from iron deficiency to iron overload. Biochim Biophys Acta Mol Basis Dis. 2019; 1865:1925–1937. doi:https://doi.org/10.1016/j.bbadis.2018.08.030.
Geissler C, Singh M. Iron, meat and health. Nutrients. 2011; 3:283–316. doi:https://doi.org/10.3390/nu3030283.
Anderson GJ, Frazer DM. Current understanding of iron homeostasis. Am J Clin Nutr. 2017; 106: 1559S–1566S. doi: https://doi.org/10.3945/ajcn.117.155804.
Tzoulaki I, Brown IJ, Chan Q, et al. Relation of iron and red meat intake to blood pressure: cross sectional epidemiological study. BMJ. 2008; 337:a258. doi:https://doi.org/10.1136/bmj.a258.
Esfandiar Z, Hosseini-Esfahani F, Mirmiran P, Habibi-Moeini AS, Azizi F. Red meat and dietary iron intakes are associated with some components of metabolic syndrome: Tehran Lipid and Glucose Study. J Transl Med. 2019; 17:313. doi:https://doi.org/10.1136/bmj.a258.
Galan P, Vergnaud AC, Tzoulaki I, et al. Low total and nonheme iron intakes are associated with a greater risk of hypertension. J Nutr. 2010; 140:75–80. doi:https://doi.org/10.3945/jn.109.114082.
Zhang B, Zhai FY, Du SF, Popkin BM. The China Health and Nutrition Survey, 1989–2011. Obes Rev. 2014; 15:2–7. doi:https://doi.org/10.1111/obr.12119.
Popkin BM, Du S, Zhai F, Zhang B. Cohort profile: the China Health and Nutrition Survey-monitoring and understanding socio-economic and health change in China, 1989–2011. Int J Epidemiol. 2010; 39:1435–1440. doi:https://doi.org/10.1093/ije/dyp322.
Li Q, Liu C, Zhang S, Li R, et al. Dietary carbohydrate intake and new-onset hypertension: a nationwide cohort study in china. Hypertension. 2021; 78:422–430. doi: https://doi.org/10.1161/HYPERTENSIONAHA.120.16751.
Zhang Z, Liu M, Zhou C, et al. Evaluation of dietary niacin and new-onset hypertension among chinese adults. JAMA Netw Open. 2021; 4:e2031669. doi: https://doi.org/10.1001/jamanetworkopen.2020.31669.
Liu M, Zhou C, Zhang Z, et al. Inverse association between riboflavin intake and new-onset hypertension: a nationwide cohort study in china. Hypertension. 2020; 76:1709–1716. doi: https://doi.org/10.1161/HYPERTENSIONAHA.120.16211.
Zhai F, Guo X, Popkin B, et al. Evaluation of the 24-hour individual recall method in China. Food Nutr Bull. 1996; 17:1–7.
Monsen ER, Hallberg L, Layrisse M, et al. Estimation of available dietary iron. Am J Clin Nutr. 1978; 31:134–141. doi:https://doi.org/10.1093/ajcn/31.1.134.
Willett W, Stampfer MJ. Total energy intake: implications for epidemiologic analyses. Am J Epidemiol. 1986; 124:17–27. doi:https://doi.org/10.1093/oxfordjournals.aje.a114366.
Andriolo V, Dietrich S, Knuppel S, et al. Traditional risk factors for essential hypertension: analysis of their specific combinations in the EPIC-Potsdam cohort. Sci Rep. 2019; 9(1): 1501. doi: https://doi.org/10.1038/s41598-019-38783-5.
Pantell MS, Prather AA, Downing JM, et al. Association of Social and Behavioral Risk Factors with Earlier Onset of Adult Hypertension and Diabetes. JAMA Netw Open. 2019; 2(5): e193933. doi: https://doi.org/10.1001/jamanetworkopen.2019.3933.
Waldvogel-Abramowski S, Waeber G, Gassner C, et al. Physiology of iron metabolism. Transfus Med Hemother. 2014; 41:213–221. doi:https://doi.org/10.1159/000362888.
Oliveira F, Rocha S, Fernandes R. Iron metabolism: from health to disease. J Clin Lab Anal. 2014; 28:210–218. doi:https://doi.org/10.1002/jcla.21668.
von Haehling S, Ebner N, Evertz R, Ponikowski P, Anker SD. Iron deficiency in heart failure: an overview. JACC Heart Fail. 2019; 7:36–46. doi:https://doi.org/10.1016/j.jchf.2018.07.015.
Ames BN, Atamna H, Killilea DW. Mineral and vitamin deficiencies can accelerate the mitochondrial decay of aging. Mol Aspects Med. 2005; 26:363–378. doi:https://doi.org/10.1016/j.mam.2005.07.007.
Chen B, Lu Y, Chen Y, Cheng J. The role of NRF2 in oxidative stress-induced endothelial injuries. J Endocrinol. 2015; 225:R83–99. doi:https://doi.org/10.1530/JOE-14-0662.
Rajapurkar MM, Shah SV, Lele SS, et al. Association of catalytic iron with cardiovascular disease. The American Journal of Cardiology. 2012; 109:438–442. doi:https://doi.org/10.1016/j.amjcard.2011.09.032.
Spasojevic-Kalimanovska V, Bogavac-Stanojevic N, Kalimanovska-Ostric D, et al. Factor analysis of risk variables associated with iron status in patients with coronary artery disease. Clin Biochem. 2014; 47:564–569. doi:https://doi.org/10.1016/j.clinbiochem.2014.03.014.
Sullivan JL. Iron in arterial plaque: modifiable risk factor for atherosclerosis. Biochim Biophys Acta. 2009; 1790:718–723. doi:https://doi.org/10.1016/j.bbagen.2008.06.005.
Hurrell R, Egli I. Iron bioavailability and dietary reference values. Am J Clin Nutr. 2010; 91(5):1461S–1467S. doi: https://doi.org/10.3945/ajcn.2010.28674F.
Adrogue HJ, Madias NE. Sodium and potassium in the pathogenesis of hypertension. N Engl J Med. 2007; 356(19):1966–78. doi: https://doi.org/10.1056/NEJMra064486.
Adrogué HJ, Madias NE. Sodium surfeit and potassium deficit: Keys to the pathogenesis of hypertension. J Am Soc Hypertens. 2014; 8(3):203–13. doi: https://doi.org/10.1016/j.jash.2013.09.003.
Gong W, Liu A, Yao Y, et al. Nutrient supplement use among the Chinese population: a cross-sectional study of the 2010–2012 China Nutrition and Health Surveillance. Nutrients. 2018; 10:1733. doi:https://doi.org/10.3390/nu10111733.
Hu FB, Stampfer MJ, Rimm E, et al. Dietary fat and coronary heart disease: a comparison of approaches for adjusting for total energy intake and modeling repeated dietary measurements. Am J Epidemiol. 1999; 149(6):531–40. doi: https://doi.org/10.1093/oxfordjournals.aje.a009849.
Dehghan M, Mente A, Zhang, X, et al. Associations of fats and carbohydrate intake with cardiovascular disease and mortality in 18 countries from five continents (PURE): a prospective cohort study. Lancet. 2017; 390(10107):2050–2062. doi: https://doi.org/10.1016/S0140-6736(17)32252-3.
Acknowledgements
This research uses data from China Health and Nutrition Survey (CHNS). We thank the National Institute for Nutrition and Health, China Center for Disease Control and Prevention, Carolina Population Center (P2C HD050924, T32 HD007168), the University of North Carolina at Chapel Hill, the NIH (R01-HD30880, DK056350, R24 HD050924, and R01-HD38700) and the NIH Fogarty International Center (D43 TW009077, D43 TW007709) for financial support for the CHNS data collection and analysis files from 1989 to 2015 and future surveys, and the China-Japan Friendship Hospital, Ministry of Health for support for CHNS 2009, Chinese National Human Genome Center at Shanghai since 2009, and Beijing Municipal Center for Disease Prevention and Control since 2011.
Funding
Sources of Funding: The study was supported by the National Key Research and Development Program [2022YFC2009600]; National Key R&D program of China [2020YFC2005000]; the National Natural Science Foundation of China [81973133, 81730019]; and the Project of the First People’s Hospital of Qujing City [2022YJKTY15].
Author information
Authors and Affiliations
Contributions
Authors’ contributions: Zhuxian Zhang and Xianhui Qin designed and conducted the study; Zhuxian Zhang, Xianhui Qin, Chengzhang Liu and Mengyi Liu performed the data management and statistical analyses; Zhuxian Zhang and Xianhui Qin drafted the manuscript; all authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest: No disclosure was reported.
Ethical standards: The institutional review boards of the University of North Carolina at Chapel Hill and the National Institute of Nutrition and Food Safety, and Chinese Center for Disease Control and Prevention, approved the study.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Zhang, Z., Liu, C., Liu, M. et al. Dietary Iron Intake and New-Onset Hypertension: A Nationwide Cohort Study from China. J Nutr Health Aging 26, 1016–1024 (2022). https://doi.org/10.1007/s12603-022-1861-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-022-1861-1