Abstract
Objectives
This study aimed to explore the association between number of teeth and cognitive frailty in American older adults.
Design
Cross-sectional study.
Setting
Community.
Participants
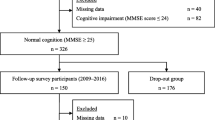
The participants were 1,531 community-dwelling older adults aged 60 or older from the NHANES database.
Methods
Frailty was assessed using a 49-item frailty index, with a cut-off value for frailty of more than 0.21. Cognitive dysfunction was evaluated by the Digit-Symbol Coding Test (DSCT), with the cut-off being below the lowest interquartile range (scores ≤37). Cognitive frailty was defined as participants who suffered from both frailty and cognitive dysfunction. Oral health indicators included number of teeth and other factors, such as the presence of gum disease, daily use of dental floss, daily use of mouthwash and self-rated oral health. Multivariable logistic regression models were used to explore the relationship between number of teeth and cognitive frailty.
Results
The mean age of the total sample was 69.67 (SD=6.60) years, and 52.71% (n=807) were female. Our study suggests there was a negative association between number of teeth and cognitive frailty (OR =0.98,95%CI:0.96–0.99, P=0.044) after controlling for potential confounding factors. In addition, older adults with 20 or more teeth had lower odds of being cognitively frail (OR=0.66,95%CI:0.44–0.99, P=0.046) than individuals who had less than 20 teeth.
Conclusion
This study suggests that older adults who have more teeth are associated with a lower risk of cognitive frailty. This finding highlights the importance of maintaining as many teeth as possible throughout life and into old age. Cohort studies will be required in the future to determine this relationship.


Similar content being viewed by others
References
Cunha AIL, Veronese N, de Melo Borges S, Ricci NA. Frailty as a predictor of adverse outcomes in hospitalized older adults: A systematic review and meta-analysis. Ageing Research Reviews 2019; 56: 100960. doi: https://doi.org/10.1016/j.arr.2019.100960
Bae JB, Han JW, Kwak KP, et al. Impact of Mild Cognitive Impairment on Mortality and Cause of Death in the Elderly. Journal of Alzheimer’s disease: JAD 2018; 64: 607–16. doi: https://doi.org/10.3233/jad-171182
Kelaiditi E, Cesari M, Canevelli M, et al. Cognitive frailty: rational and definition from an (I.A.N.A./I.A.G.G.) international consensus group. The journal of nutrition, health & aging 2013; 17: 726–34. doi: https://doi.org/10.1007/sl2603-013-0367-2
Zhang XM, Jiao J, Zhu C, et al. Cognitive Frailty and 30-Day Mortality in a National Cohort of Older Chinese Inpatients. Clinical interventions in aging 2021; 16: 389–401. doi: 10.2147/cia.S294106
Bu Z, Huang A, Xue M, Li Q, Bai Y, Xu G. Cognitive frailty as a predictor of adverse outcomes among older adults: A systematic review and meta-analysis. Brain and behavior 2021; 11: e01926. doi: https://doi.org/10.1002/brb3.1926
Vatanabe TP, Pedroso RV, Teles RHG, et al. A systematic review and meta-analysis on cognitive frailty in community-dwelling older adults: risk and associated factors. Aging & mental health 2021: 1–13. doi: https://doi.org/10.1080/13607863.2021.1884844
Patel J, Wallace J, Doshi M, et al. Oral health for healthy ageing. The Lancet Healthy Longevity 2021; 2: e521–e27. doi: https://doi.org/10.1016/S2666-7568(21)00142-2
Ortega O, Parra C, Zarcero S, Nart J, Sakwinska O, Clavé P. Oral health in older patients with oropharyngeal dysphagia. Age and ageing 2014; 43: 132–7. doi: 10.1093/ageing/aft164
Glick M, Williams DM, Kleinman DV, Vujicic M, Watt RG, Weyant RJ. A new definition for oral health developed by the FDI World Dental Federation opens the door to a universal definition of oral health. The Journal of the American Dental Association 2016; 147: 915–17. doi: https://doi.org/10.1016/j.adaj.2016.10.001
Saito S, Ohi T, Murakami T, et al. Association between tooth loss and cognitive impairment in community-dwelling older Japanese adults: a 4-year prospective cohort study from the Ohasama study. BMC oral health 2018; 18: 142. doi: https://doi.org/10.1186/s12903-018-0602-7
Zhang S, Yang F, Wang Z, et al. Poor oral health conditions and cognitive decline: Studies in humans and rats. PloS one 2020; 15: e0234659. doi: https://doi.org/10.1371/journal.pone.0234659
Takehara S, Wright FAC, Waite LM, et al. Oral health and cognitive status in the Concord Health and Ageing in Men Project: A cross-sectional study in community-dwelling older Australian men. Gerodontology 2020; 37: 353–60. doi: https://doi.org/10.1111/ger.12469
Qi X, Zhu Z, Plassman BL, Wu B. Dose-Response Meta-Analysis on Tooth Loss With the Risk of Cognitive Impairment and Dementia. Journal of the American Medical Directors Association 2021; 22: 2039–45. doi: https://doi.org/10.1016/j.jamda.2021.05.009
Dibello V, Zupo R, Sardone R, et al. Oral frailty and its determinants in older age: a systematic review. The Lancet Healthy Longevity 2021; 2: e507–e20. doi: https://doi.org/10.1016/S2666-7568(21)00143-4
Kuo YW, Chen MY, Chang LC, Lee JD. Oral Health as a Predictor of Physical Frailty among Rural Community-Dwelling Elderly in an Agricultural County of Taiwan: A Cross-Sectional Study. International journal of environmental research and public health 2021; 18. doi: https://doi.org/10.3390/ijerph18189805
Castrejón-Pérez RC, Jiménez-Corona A, Bernabé E, et al. Oral Disease and 3-Year Incidence of Frailty in Mexican Older Adults. The journals of gerontology Series A, Biological sciences and medical sciences 2017; 72: 951–57. doi: https://doi.org/10.1093/gerona/glw201
Mitnitski AB, Mogilner AJ, Rockwood K. Accumulation of deficits as a proxy measure of aging. The Scientific World Journal 2001; 1: 323–36. doi: https://doi.org/10.1100/tsw.2001.58
Hakeem FF, Bernabé E, Sabbah W. Self-rated oral health and frailty index among older Americans. Gerodontology 2021; 38: 185–90. doi: https://doi.org/10.1111/ger.12513
Blodgett J, Theou O, Kirkland S, Andreou P, Rockwood KJAog, geriatrics. Frailty in NHANES: comparing the frailty index and phenotype. 2015; 60: 464–70. doi:https://doi.org/10.1016/j.archger.2015.01.016. Epub 2015 Feb 3
Li A, Chen Y, Visser A, Marks LAM, Tjakkes GE. Combined association of cognitive impairment and poor oral health on mortality risk in older adults: Results from the NHANES with 15 years of follow-up. Journal of periodontology 2021.doi: https://doi.org/10.1002/jper.21-0292
Hakeem FF, Bernabé E, Sabbah W. Association Between Oral Health and Frailty Among American Older Adults. Journal of the American Medical Directors Association 2021; 22: 559–63.e2. doi: https://doi.org/10.1016/j.jamda.2020.07.023
Yang L, Koyanagi A, Smith L, et al. Hand grip strength and cognitive function among elderly cancer survivors. PloS one 2018; 13: e0197909. doi: https://doi.org/10.1371/journal.pone.0197909
de Souto Barreto P, Delrieu J, Andrieu S, Vellas B, Rolland Y. Physical Activity and Cognitive Function in Middle-Aged and Older Adults: An Analysis of 104,909 People From 20 Countries. Mayo Clinic proceedings 2016; 91: 1515–24. doi: https://doi.org/10.1016/j.mayocp.2016.06.032
Fan Y, Zhang Y, Li J, Liu Y, Zhou L, Yu Y. Association between Healthy Eating Index-2015 and physical frailty among the United States elderly adults: the National Health and Nutrition Examination Survey (NHANES) 2011–2014. Aging Clin Exp Res 2021; 33: 3245–55. doi: https://doi.org/10.1007/s40520-021-01874-3
Kurnat-Thoma EL, Murray MT, Juneau P. Frailty and Determinants of Health Among Older Adults in the United States 2011–2016. Journal of aging and health 2021: 8982643211040706. doi: https://doi.org/10.1177/08982643211040706
Kim H, Awata S, Watanabe Y, et al. Cognitive frailty in community-dwelling older Japanese people: Prevalence and its association with falls. Geriatrics & gerontology international 2019; 19: 647–53. doi: https://doi.org/10.1111/ggi.l3685
Qiu Y, Li G, Wang X, et al. Prevalence of cognitive frailty among community-dwelling older adults: A systematic review and meta-analysis. International journal of nursing studies 2022; 125: 104112. doi: https://doi.org/10.1016/j.ijnurstu.2021.104112
Sugimoto T, Sakurai T, Ono R, et al. Epidemiological and clinical significance of cognitive frailty: A mini review. Ageing Research Reviews 2018; 44: 1–7. doi: https://doi.org/10.1016/j.arr.2018.03.002
Hakeem FF, Bernabé E, Sabbah W. Association between oral health and frailty: A systematic review of longitudinal studies. Gerodontology 2019; 36: 205–15. doi: https://doi.org/10.1111/ger.12406
Zhang Y, Ge M, Zhao W, et al. Association Between Number of Teeth, Denture Use and Frailty: Findings from the West China Health and Aging Trend Study. The journal of nutrition, health & aging 2020; 24: 423–28. doi: https://doi.org/10.1007/s12603-020-1346-z
de Andrade FB, Lebrão ML, Santos JL, Duarte YA. Relationship between oral health and frailty in community-dwelling elderly individuals in Brazil. J Am Geriatr Soc 2013; 61: 809–14. doi: https://doi.org/10.1111/jgs.l2221
St John PD, Tyas SL, Griffith LE, Menec V. The cumulative effect of frailty and cognition on mortality — results of a prospective cohort study. International psychogeriatrics 2017; 29: 535–43. doi: https://doi.org/10.1017/sl041610216002088
Lee Y, Kim J, Chon D, et al. The effects of frailty and cognitive impairment on 3-year mortality in older adults. Maturitas 2018; 107: 50–55. doi: https://doi.org/10.1016/j.maturitas.2017.10.006
Facal D, Maseda A, Pereiro AX, et al. Cognitive frailty: A conceptual systematic review and an operational proposal for future research. Maturitas 2019; 121: 48–56. doi: https://doi.org/10.1016/j.maturitas.2018.12.006
Mosaddad SA, Tahmasebi E, Yazdanian A, et al. Oral microbial biofilms: an update. European journal of clinical microbiology & infectious diseases: official publication of the European Society of Clinical Microbiology 2019; 38: 2005–19. doi: https://doi.org/10.1007/s10096-019-03641-9
Curtis MA, Diaz PI, Van Dyke TE. The role of the microbiota in periodontal disease. Periodontology 2000 2020; 83: 14–25. doi: 10.1111/prd.12296
Azzolino D, Passarelli PC, De Angelis P, Piccirillo GB, D’Addona A, Cesari M. Poor Oral Health as a Determinant of Malnutrition and Sarcopenia. Nutrients 2019; 11. doi: https://doi.org/10.3390/nu11122898
Harding A, Gonder U, Robinson SJ, Crean S, Singhrao SK. Exploring the Association between Alzheimer’s Disease, Oral Health, Microbial Endocrinology and Nutrition. Frontiers in aging neuroscience 2017; 9: 398. doi: https://doi.org/10.3389/fnagi.2017.00398
Fang WL, Jiang MJ, Gu BB, et al. Tooth loss as a risk factor for dementia: systematic review and meta-analysis of 21 observational studies. BMC psychiatry 2018; 18: 345. doi: https://doi.org/10.1186/s12888-018-1927-0
Teixeira FB, Pereira Fernandes Lde M, Noronha PA, et al. Masticatory deficiency as a risk factor for cognitive dysfunction. International journal of medical sciences 2014; 11: 209–14. doi: https://doi.org/10.7150/ijms.6801
Dibello V, Lozupone M, Manfredini D, et al. Oral frailty and neurodegeneration in Alzheimer’s disease. Neural regeneration research 2021; 16: 2149–53. doi: https://doi.org/10.4103/1673-5374.310672
Patil MS, Patil SB. Geriatric patient - psychological and emotional considerations during dental treatment. Gerodontology 2009; 26: 72–7. doi: https://doi.org/10.1111/j.1741-2358.2008.00245.x
Kayombo CM, Mumghamba EG. Self-Reported Halitosis in relation to Oral Hygiene Practices, Oral Health Status, General Health Problems, and Multifactorial Characteristics among Workers in Ilala and Temeke Municipals, Tanzania. International journal of dentistry 2017; 2017: 8682010. doi: https://doi.org/10.1155/2017/8682010
Davis DM, Fiske J, Scott B, Radford DR. The emotional effects of tooth loss in a group of partially dentate people: a quantitative study. The European journal of prosthodontics and restorative dentistry 2001; 9: 53–7.
Kunrath I, Silva AER. Oral health and depressive symptoms among older adults: longitudinal study. Aging & mental health 2021; 25: 2265–71. doi: https://doi.org/10.1080/13607863.2020.1855104
Koyama S, Saito M, Cable N, et al. Examining the associations between oral health and social isolation: A cross-national comparative study between Japan and England. Social science & medicine (1982) 2021; 277: 113895. doi: https://doi.org/10.1016/j.socscimed.2021.113895
Qi X, Pei Y, Wang K, Han S, Wu B. Social isolation, loneliness and accelerated tooth loss among Chinese older adults: A longitudinal study. Community dentistry and oral epidemiology 2022doi: https://doi.org/10.1111/cdoe.l2727
Malek Rivan NF, Shahar S, Rajab NF, et al. Cognitive frailty among Malaysian older adults: baseline findings from the LRGS TUA cohort study. Clinical interventions in aging 2019; 14: 1343–52. doi: https://doi.org/10.2147/cia.S211027
De Roeck EE, van der Vorst A, Engelborghs S, Zijlstra GAR, Dierckx E. Exploring Cognitive Frailty: Prevalence and Associations with Other Frailty Domains in Older People with Different Degrees of Cognitive Impairment. Gerontology 2020; 66: 55–64. doi: https://doi.org/10.1159/000501168
Clark D, Kotronia E, Ramsay SE. Frailty, aging, and periodontal disease: Basic biologic considerations. Periodontology 2000 2021; 87: 143–56. doi: https://doi.org/10.1111/prd.12380
Soysal P, Stubbs B, Lucato P, et al. Inflammation and frailty in the elderly: A systematic review and meta-analysis. Ageing Research Reviews 2016; 31: 1–8. doi: https://doi.org/10.1016/j.arr.2016.08.006
Singhrao SK, Harding A, Simmons T, Robinson S, Kesavalu L, Crean S. Oral inflammation, tooth loss, risk factors, and association with progression of Alzheimer’s disease. Journal of Alzheimer’s disease: JAD 2014; 42: 723–37. doi: https://doi.org/10.3233/jad-140387
Acknowledgments
The authors acknowledge the community-dwelling older American adults who agreed to participate in the National Health and Nutrition Examination Survey. Xiaoming Zhang especially acknowledges Xing-lin Chen for supporting the statistical data guidance.
Funding
Funding: No organization or sponsors provided funding for this study.
Author information
Authors and Affiliations
Contributions
Author contributions: Xiaoming Zhang wrote the first draft. Xinjuan Wu and Wei-Chen were responsible for the research question and for critically revising the manuscript. Xiaoming Zhang and Xinjuan Wu performed the data analysis.
Corresponding authors
Ethics declarations
Conflict of interest: There are no author conflicts of interest.
Ethical approval and consent to participate: Not applicable.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Zhang, XM., Wu, X. & Chen, W. The Association between Number of Teeth and Cognitive Frailty in Older Adults: A Cross-Sectional Study. J Nutr Health Aging 26, 430–438 (2022). https://doi.org/10.1007/s12603-022-1783-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-022-1783-y