Abstract
Objectives
To evaluate the characteristics of sarcopenic dysphagia (SD) and the prognosis of swallowing function in convalescent rehabilitation hospital patients; and to investigate the association between malnutrition severity and SD.
Design
A prospective, multi-center, cohort study.
Setting
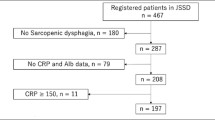
We extracted registry data from the Japanese Sarcopenic Dysphagia Database, focusing on patients admitted to convalescent rehabilitation hospitals.
Participants
A total of 207 participants were recruited and stratified according to the presence or absence of SD. Next, the participants were divided into groups based on nutrition status using the Global Leadership Initiative on Malnutrition criteria normal nutrition, moderate malnutrition, and severe malnutrition. We also compared the outcomes between patients with SD (SD group) and those without SD (no-SD group) according to malnutrition status.
Measurements
The Food Intake LEVEL Scale (FILS) score was the outcome measure. Higher scores on the FILS indicate better swallowing function. We compared the patient characteristics between the SD and non-SD groups among all patients and then according to the severity of malnutrition.
Results
A total of 207 patients were recruited. 11 were diagnosed with normal nutrition, 72 with moderate malnutrition, and 124 with severe malnutrition. There were 128 participants with SD and 79 participants without SD; the prevalence of SD was 61.8%. Hip fracture was the most common disease among the SD patients (34.4%). The median time to the end of follow-up was 73.5 days for the SD group and 84.0 days for the no-SD group. There was no significant difference in the FILS score between the SD and no-SD groups, but the increase in the FILS score was significantly lower in the SD group than the no-SD group among patients with severe malnutrition after adjusting for confounding factors (age, sex, FILS at admission, BMI, cognitive functional independence measure, and care level before onset) (β = −0.206, p = 0.011, 95% confidence interval = −0.723, −0.098).
Conclusion
Orthopedic diseases are the most common type of disease among SD patients in convalescent rehabilitation hospitals. Swallowing dysfunction was particularly severe in malnourished patients with SD. This result suggests the importance of the definition of SD for malnourished patients. We should practice nutritional management as soon as possible in severely malnourished patients diagnosed with SD.

Similar content being viewed by others
References
Wakabayashi H. Presbyphagia and sarcopenic dysphagia: Association between aging, sarcopenia, and deglutition disorders. J Frailty Aging 2014;3:97–103. Doi: https://doi.org/10.14283/jfa.2014.8.
Mori T, Fujishima I, Wakabayashi H, Oshima F, Itoda M, Kunieda K, et al. Development, reliability, and validity of a diagnostic algorithm for sarcopenic dysphagia. JCSM Clinical Reports 2017;2:1–10. Doi: https://doi.org/10.17987/jcsm-cr.v2i2.17.
Fujishima I, Fujiu-Kurachi M, Arai H, Hyodo M, Kagaya H, Maeda K, et al. Sarcopenia and dysphagia: Position paper by four professional organizations. Geriatrics & Gerontology International 2019;19:91–7. Doi: https://doi.org/10.1111/ggi.13591.
Wakabayashi H, Takahashi R, Murakami T. The prevalence and prognosis of sarcopenic dysphagia in patients who require dysphagia rehabilitation. J Nutr Health Aging 2019;23:84–8. Doi: https://doi.org/10.1007/s12603-018-1117-2.
Ogawa N, Wakabayashi H, Mori T, Fujishima I, Oshima F, Itoda M, et al. Digastric muscle mass and intensity in older patients with sarcopenic dysphagia by ultrasonography. Geriatr Gerontol Int 2021;21:14–9. Doi: https://doi.org/10.1111/ggi.14079.
Shimizu A, Fujishima I, Maeda K, Wakabayashi H, Nishioka S, Ohno T, et al. Nutritional management enhances the recovery of swallowing ability in older patients with sarcopenic dysphagia. Nutrients 2021;13:596. Doi: https://doi.org/10.3390/nu13020596.
Shimizu A, Maeda K, Koyanagi Y, Kayashita J, Fujishima I, Mori N. The global leadership initiative on malnutrition—defined malnutrition predicts prognosis in persons with stroke-related dysphagia. J Am Med Dir Assoc 2019;20:1628–33. Doi: https://doi.org/10.1016/j.jamda.2019.07.008.
Tagliaferri S, Lauretani F, Pelá G, Meschi T, Maggio M. The risk of dysphagia is associated with malnutrition and poor functional outcomes in a large population of outpatient older individuals. Clin Nutr 2019;38:2684–9. Doi: https://doi.org/10.1016/j.clnu.2018.11.022.
Sella-Weiss O. Association between swallowing function, malnutrition and frailty in community dwelling older people. Clin Nutr ESPEN 2021 Oct;: 476–485. Doi: https://doi.org/10.1016/j.clnesp.2021.06.028.
Ikenaga Y, Nakayama S, Taniguchi H, Ohori I, Komatsu N, Nishimura H, et al. Factors Predicting Recovery of Oral Intake in Stroke Survivors with Dysphagia in a Convalescent Rehabilitation Ward. J Stroke Cerebrovasc Dis 2017;26:1013–1019. Doi: https://doi.org/10.1016/j.jstrokecerebrovasdis.2016.12.005.
Cederholm T, Jensen GL, Correia M, Gonzalez MC, Fukushima R, Higashiguchi T, et al. GLIM criteria for the diagnosis of malnutrition — A consensus report from the global clinical nutrition community. JPEN J Parenter Enteral Nutr 2019;38:1–9. Doi: https://doi.org/10.1016/j.clnu.2018.08.002.
Mizuno S, Wakabayashi H, Fujishima I, Kishima M, Itoda M, Yamakawa M, et al. Construction and quality evaluation of the Japanese Sarcopenic Dysphagia Database. J Nutr Health Aging 2021;25:926–932. Doi: https://doi.org/10.1007/s12603-021-1646-y.
Kunieda K, Ohno T, Fujishima I, Hojo K, Morita T. Reliability and validity of a tool to measure the severity of dysphagia: the Food Intake LEVEL Scale. J Pain Symptom Manage 2013;46:201–6. Doi: https://doi.org/10.1016/j.jpainsymman.2012.07.020.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–81. Doi: https://doi.org/10.1016/j.jbi.2008.08.010.
Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing 2019;48:16–31. Doi: https://doi.org/10.1093/ageing/afy169.
Miyai I, Sonoda S, Nagai S, Takayama Y, Inoue Y, Kakehi A, et al. Results of new policies for inpatient rehabilitation coverage in Japan. Neurorehabil Neural Repair. 2011;25:540–7. Doi: https://doi.org/10.1177/1545968311402696.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987;40:373–83. Doi: https://doi.org/10.1016/0021-9681(87)90171-8.
Ministry of Health, Labour and Welfare. Long-term care, health and welfare services for the elderly. https://www.mhlw.go.jp/nglish/policy/care-welfare/care-welfare-elderly/dl/ltcisj_e.pdf Accessed 28 June 2021.
Shimizu A, Fujishima I, Maeda K, Wakabayashi H, Nishioka S, Ohno T, et al. Effect of low tongue pressure on nutritional status and improvement of swallowing function in sarcopenic dysphagia. Nutrition 2021;90:111295. Doi: https://doi.org/10.1016/j.nut.2021.111295.
Beric E, Smith R, Phillips K, Patterson C, Pain T. Swallowing disorders in an older fractured hip population. Aust J Rural Health 2019;27:304–10. Doi: https://doi.org/10.1111/ajr.12512.
Madsen G, Kristoffersen SM, Westergaard MR, Gjødvad V, Jessen MM, Melgaard D. Prevalence of swallowing and eating difficulties in an elderly postoperative hip fracture population-a multi-center-based pilot study. Geriatrics (Basel) 2020;5. Doi: https://doi.org/10.3390/geriatrics5030052.
Mateos-Nozal J, Sanchez Garcia E, Romero Rodríguez E, Cruz-Jentoft AJ. Oropharyngeal dysphagia in older patients with hip fracture. Age Ageing 2021;50:1416–21. Doi: https://doi.org/10.1093/ageing/afab032.
Skeie E, Tangvik RJ, Nymo LS, Harthug S, Lassen K, Viste A. Weight loss and BMI criteria in GLIM’s definition of malnutrition is associated with postoperative complications following abdominal resections - Results from a National Quality Registry. Clin Nutr 2020;39:1593–9. Doi: https://doi.org/10.1016/j.clnu.2019.07.003.
López-Gómez JJ, Ballesteros-Pomar MD, Torres-Torres B, De la Maza BP, Penacho-Lázaro MÁ, Palacio-Mures JM, et al. Malnutrition at diagnosis in amyotrophic lateral sclerosis (ALS) and its influence on survival: Using glim criteria. Clin Nutr 2021;40:237–44. Doi: https://doi.org/10.1016/j.clnu.2020.05.014.
Zhang X, Tang M, Zhang Q, Zhang K-P, Guo Z-Q, Xu H-X, et al. The GLIM criteria as an effective tool for nutrition assessment and survival prediction in older adult cancer patients. Clin Nutr 2021;40:1224–32. Doi: https://doi.org/10.1016/j.clnu.2020.08.004.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was performed in accordance with the ethical standards of the Declaration of Helsinki 1964 and its later amendments.
Additional information
Conflicts of interest
Kazue Taguchi, Mikio Fujimoto, Shigeru Obayashi, Mitsuru Yamamoto, Shinta Nishioka, and Ryo Momosaki have nothing to disclose.
Disclosure statement
Hidetaka Wakabayashi reports grants from JSPS KAKENHI, Grant Number 19H03979. Kazue Taguchi, Mikio Fujimoto, Shigeru Obayashi, Mitsuru Yamamoto, Shinta Nishioka, and Ryo Momosaki have nothing to disclose.
Rights and permissions
About this article
Cite this article
Taguchi, K., Wakabayashi, H., Fujimoto, M. et al. Association between Malnutrition Severity and Swallowing Function in Convalescent Rehabilitation Wards: A Multi-Center Cohort Study in Malnourished Patients with Sarcopenic Dysphagia. J Nutr Health Aging 26, 469–476 (2022). https://doi.org/10.1007/s12603-022-1782-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-022-1782-z