Abstract
Objectives
To investigate the prevalence of sarcopenia and dysphagia in nursing homes and to analyze the associations between sarcopenic parameters and dysphagia.
Design
A cross-sectional study.
Setting
Nursing homes in Chengdu, Sichuan, China.
Participants
The study included 365 participants (122 men and 243 women) aged 60 years or older who could walk independently or with walking aids for at least 50 meters.
Measurements
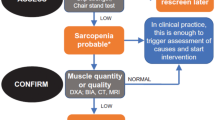
Dysphagia was defined by the water swallow test and sarcopenia and its components were evaluated by the criteria of the Asian Working Group for Sarcopenia, 2019. The values and percentages of sarcopenia associated parameters in relation to dysphagia were analyzed in both male and female residents. The Benjamini-Hochberg method was used to adjust for multiple comparisons. The relationship between sarcopenic components and dysphagia was analyzed using multivariate logistic regression analysis by sex.
Results
A total of 365 residents (mean age: 84.28 years; 122 men and 243 women) were included in the study. Sarcopenia was diagnosed in 63.0% (n=230) and dysphagia in 75.3% (n = 275) of residents. For men, the percentage of sarcopenia was higher in residents with dysphagia. However, the sarcopenia percentage did not differ significantly between women with and without dysphagia. In both men and women, the handgrip strength (HGS) values were significantly lower in the dysphagic residents. The calf circumference (CC) value and appendicular skeletal muscle index (ASMI) were significantly lower in dysphagic men, while the SARC-CalF scores were higher. In women, the SPPB score was lower in residents with dysphagia. Furthermore, multivariate logistic regression analysis showed that low calf circumference (OR 4.415, 95% CI 1.561–12.490) and sarcopenia (OR 2.968, 95% CI 1.121–7.858) were significantly associated with dysphagia in men after adjusting for co-factors.
Conclusion
There is a high percentage of both dysphagia and sarcopenia in nursing home residents in West China. Low calf circumference and sarcopenia had strong associations with dysphagia among male nursing home residents.


Similar content being viewed by others
References
Cruz-Jentoft, A. et al. (2010) Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age and ageing 39, 412–423, doi:https://doi.org/10.1093/ageing/afq034.
Chang, S. & Lin, P. (2016) Systematic Literature Review and Meta-Analysis of the Association of Sarcopenia With Mortality. Worldviews on evidence-based nursing 13, 153–162, doi:https://doi.org/10.1111/wvn.12147.
Janssen, I., Heymsfield, S. & Ross, R. (2002) Low relative skeletal muscle mass (sarcopenia) in older persons is associated with functional impairment and physical disability. Journal of the American Geriatrics Society 50, 889–896, doi:https://doi.org/10.1046/j.1532-5415.2002.50216.x.
Chang, K., Hsu, T., Wu, W., Huang, K. & Han, D. (2016) Association Between Sarcopenia and Cognitive Impairment: A Systematic Review and Meta-Analysis. Journal of the American Medical Directors Association 17, 1164.e1167–1164.e1115, doi:https://doi.org/10.1016/j.jamda.2016.09.013.
Cruz-Jentoft, A. et al. (2014) Prevalence of and interventions for sarcopenia in ageing adults: a systematic review. Report of the International Sarcopenia Initiative (EWGSOP and IWGS). Age and ageing 43, 748–759, doi:https://doi.org/10.1093/ageing/afu115.
Shen, Y. et al. (2019) Prevalence and Associated Factors of Sarcopenia in Nursing Home Residents: A Systematic Review and Meta-analysis. Journal of the American Medical Directors Association 20, 5–13, doi:https://doi.org/10.1016/j.jamda.2018.09.012.
Morisaki, N. (2017) Relationship between swallowing functions and health-related quality of life among community-dwelling dependent older individuals. Japan journal of nursing science: JJNS 14, 353–363, doi:https://doi.org/10.1111/jjns.12168.
Miura, H., Yamasaki, K., Morizaki, N., Moriya, S. & Sumi, Y. (2010) Factors influencing oral health-related quality of life (OHRQoL) among the frail elderly residing in the community with their family. Archives of gerontology and geriatrics 51, e62–65, doi:https://doi.org/10.1016/j.archger.2009.12.003.
Serra-Prat, M. et al. (2011) Prevalence of oropharyngeal dysphagia and impaired safety and efficacy of swallow in independently living older persons. Journal of the American Geriatrics Society 59, 186–187, doi:https://doi.org/10.1111/j.1532-5415.2010.03227.x.
Carrión, S. et al. (2015) Oropharyngeal dysphagia is a prevalent risk factor for malnutrition in a cohort of older patients admitted with an acute disease to a general hospital. Clinical nutrition (Edinburgh, Scotland) 34, 436–442, doi:https://doi.org/10.1016/j.clnu.2014.04.014.
Lin, L., Wu, S., Chen, H., Wang, T. & Chen, M. (2002) Prevalence of impaired swallowing in institutionalized older people in taiwan. Journal of the American Geriatrics Society 50, 1118–1123, doi:https://doi.org/10.1046/j.1532-5415.2002.50270.x.
Maeda, K. & Akagi, J. (2016) Sarcopenia is an independent risk factor of dysphagia in hospitalized older people. Geriatrics & gerontology international 16, 515–521, doi:https://doi.org/10.1111/ggi.12486.
Carrión, S. et al. (2017) Nutritional status of older patients with oropharyngeal dysphagia in a chronic versus an acute clinical situation. Clinical nutrition (Edinburgh, Scotland) 36, 1110–1116, doi:https://doi.org/10.1016/j.clnu.2016.07.009.
Wakabayashi, H. & Sakuma, K. (2014) Rehabilitation nutrition for sarcopenia with disability: a combination of both rehabilitation and nutrition care management. Journal of cachexia, sarcopenia and muscle 5, 269–277, doi:https://doi.org/10.1007/s13539-014-0162-x.
Wakabayashi, H. (2014) Presbyphagia and Sarcopenic Dysphagia: Association between Aging, Sarcopenia, and Deglutition Disorders. The Journal of frailty & aging 3, 97–103, doi:https://doi.org/10.14283/jfa.2014.8.
Chen, L. et al. (2020) Asian Working Group for Sarcopenia: 2019 Consensus Update on Sarcopenia Diagnosis and Treatment. Journal of the American Medical Directors Association 21, 300–307.e302, doi:https://doi.org/10.1016/j.jamda.2019.12.012.
Kuroda, Y. & Kuroda, R. (2012) Relationship between thinness and swallowing function in Japanese older adults: implications for sarcopenic dysphagia. Journal of the American Geriatrics Society 60, 1785–1786, doi:https://doi.org/10.1111/j.1532-5415.2012.04123.x.
Clavé, P. & Shaker, R. (2015) Dysphagia: current reality and scope of the problem. Nature reviews. Gastroenterology & hepatology 12, 259–270, doi:https://doi.org/10.1038/nrgastro.2015.49.
Wakabayashi, H., Takahashi, R. & Murakami, T. (2019) The Prevalence and Prognosis of Sarcopenic Dysphagia in Patients Who Require Dysphagia Rehabilitation. The journal of nutrition, health & aging 23, 84–88, doi:https://doi.org/10.1007/s12603-018-1117-2.
Patterson, J., McColl, E., Carding, P., Kelly, C. & Wilson, J. (2009) Swallowing performance in patients with head and neck cancer: a simple clinical test. Oral oncology 45, 904–907, doi:https://doi.org/10.1016/j.oraloncology.2009.03.012.
Horiguchi, S. & Suzuki, Y. (2011) Screening tests in evaluating swallowing function. Japan Medical Association Journal 54, 31–34.
Vasunilashorn, S. et al. (2009) Use of the Short Physical Performance Battery Score to predict loss of ability to walk 400 meters: analysis from the InCHIANTI study. The journals of gerontology. Series A, Biological sciences and medical sciences 64, 223–229, doi:https://doi.org/10.1093/gerona/gln022.
Malmstrom, T. & Morley, J. (2013) SARC-F: a simple questionnaire to rapidly diagnose sarcopenia. Journal of the American Medical Directors Association 14, 531–532, doi:https://doi.org/10.1016/j.jamda.2013.05.018.
Mahoney, F. & Barthel, D. (1965) Functional evaluation: the Barthel index. Maryland state medical journal 14, 61–65.
Lawton, M. & Brody, E. (1969) Assessment of older people: self-maintaining and instrumental activities of daily living. The Gerontologist 9, 179–186.
Ertan, T. & Eker, E. (2000) Reliability, validity, and factor structure of the geriatric depression scale in Turkish elderly: are there different factor structures for different cultures? International psychogeriatrics 12, 163–172, doi:https://doi.org/10.1017/s1041610200006293.
Folstein, M., Folstein, S. & McHugh, P. (1975) “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. Journal of psychiatric research 12, 189–198, doi:https://doi.org/10.1016/0022-3956(75)90026-6.
Chen, P., Golub, J., Hapner, E. & Johns, M. (2009) Prevalence of perceived dysphagia and quality-of-life impairment in a geriatric population. Dysphagia 24, 1–6, doi:https://doi.org/10.1007/s00455-008-9156-1.
Matsuo, H. & Yoshimura, Y. (2018) Calf circumference is associated with dysphagia in acute-care inpatients. Geriatric nursing (New York, N.Y.) 39, 186–190, doi:https://doi.org/10.1016/j.gerinurse.2017.08.003.
Hu, F. et al. (2021) Mid-Upper Arm Circumference as an Alternative Screening Instrument to Appendicular Skeletal Muscle Mass Index for Diagnosing Sarcopenia. Clinical interventions in aging 16, 1095–1104, doi:https://doi.org/10.2147/cia.S311081.
Zhao, W. et al. (2018) Systematic Review and Meta-Analysis of the Association between Sarcopenia and Dysphagia. The journal of nutrition, health & aging 22, 1003–1009, doi:https://doi.org/10.1007/s12603-018-1055-z.
Fırat Ozer, F., Akın, S., Soysal, T., Gokcekuyu, B. & Erturk Zararsız, G. (2021) Relationship Between Dysphagia and Sarcopenia with Comprehensive Geriatric Evaluation. Dysphagia 36, 140–146, doi:https://doi.org/10.1007/s00455-020-10120-3.
Kurosawa, Y. et al. (2019) Calf Circumference Is a Useful Index for Assessing Dysphagia among Community Dwelling Elderly Recipients of Long-Term Care. The Tohoku journal of experimental medicine 248, 201–208, doi:https://doi.org/10.1620/tjem.248.201.
Trevisan, C., Vetrano, D., Calvani, R., Picca, A. & Welmer, A. (2021) Twelve-year sarcopenia trajectories in older adults: results from a population-based study. Journal of cachexia, sarcopenia and muscle, doi:https://doi.org/10.1002/jcsm.12875.
Bonnefoy, M., Jauffret, M., Kostka, T. & Jusot, J. (2002) Usefulness of calf circumference measurement in assessing the nutritional state of hospitalized elderly people. Gerontology 48, 162–169, doi:https://doi.org/10.1159/000052836.
Baijens, L. et al. (2016) European Society for Swallowing Disorders — European Union Geriatric Medicine Society white paper: oropharyngeal dysphagia as a geriatric syndrome. Clinical interventions in aging 11, 1403–1428, doi:https://doi.org/10.2147/cia.S107750.
Yoshimura, Y., Uchida, K., Jeong, S. & Yamaga, M. (2016) Effects of Nutritional Supplements on Muscle Mass and Activities of Daily Living in Elderly Rehabilitation Patients with Decreased Muscle Mass: A Randomized Controlled Trial. The journal of nutrition, health & aging 20, 185–191, doi:https://doi.org/10.1007/s12603-015-0570-4.
Acknowledgments
The authors are grateful to the staffs of Chengdu Jinxin Geriatrics Hospital for their support.
Funding
Funding: This study was supported by National Natural Science Foundation of China (81501197), Sichuan Province Science and Technology Support Program (2020YFG0086), Chengdu Science and Technology Bureau (2021-YF05-00987-SN), National Clinical Research Center for Geriatrics, West China Hospital, Sichuan University (Z20191010).
Author information
Authors and Affiliations
Contributions
Author Contributions:Conceptualization, Y.L. and B.D.; data curation, Y.L, J.S., R.X., Y.J. and X.Y.; project administration, Y.L., Y.J. and Y.X.; writing — original draft preparation, J.Y. and Y.L.; funding acquisition, Y.L.
Corresponding author
Ethics declarations
Informed Consent Statement: Informed consent was obtained from all subjects involved in the study.
Conflicts of Interest: The authors declare no conflicts of interest.
Additional information
Institutional Review Board Statement: The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the research ethics committee of Sichuan University (protocol code 2019–64, and approval date February 21st, 2019).
Rights and permissions
About this article
Cite this article
Yuan, J., Lin, Y., Song, J. et al. Associations of Sarcopenic Parameters with Dysphagia in Older Nursing Home Residents: A Cross-Sectional Study. J Nutr Health Aging 26, 339–345 (2022). https://doi.org/10.1007/s12603-022-1768-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-022-1768-x