Abstract
Objectives
The frail elderly have an increased risk of frailty because of reduced physical activity, cognitive ability and quality of life. This study aims to evaluate the effects of integrated exercise intervention on the attenuation of frailty in elderly nursing home residents.
Design
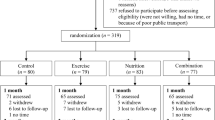
This study was a cluster randomized controlled trial. SETTING AND PARTICIPANTS: 146 elderly frailty people from 8 elderly nursing homes in Harbin, China, were randomly assigned into the intervention group and control group after obtaining their informed consent.
Intervention
The intervention group performed integrated exercise interventions for 12 months, while the control group only continued with their daily activities.
Measurements
Sociodemographic, health-related data, frailty levels, gait parameters, cognition, and quality of life were evaluated.
Results
The mean age of participants was 80.74± 2.89 years, and 70.37% (n=95) were female. The Difference-in-difference regression showed that, compared with the control group, phenotypic frailty score (β3 =−1.40, p < 0.001) and stride time (β3 = −0.38, p < 0.001) decreased significantly in the intervention group, stride velocity (β3 = 0.24, p < 0.001), step length (β3 = 0.08, p <0.001), cadence (β3 = 17.79, p < 0.001), MMSE total score (β3 = 1.90, p < 0.001) and QOL total score (β3 = 11.84, p < 0.001) increased significantly in the intervention group.
Conclusion
The integrated exercise intervention can effectively improve the attenuation of frailty, gait parameters, cognitive function, and quality of life in elderly nursing homes. We can use the findings of this study as a reference for the design of activities for the elderly nursing home residents, to provide them with appropriate exercises, improve their physical functions, and improve or delay their frailty level, which is principally important for developing countries in east Asia where rehabilitation resources are generally scarce.

Similar content being viewed by others
References
Hoogendijk EO, Afilalo J, Ensrud KE, Kowal P, Onder G, Fried LP. Frailty: implications for clinical practice and public health. The Lancet 2019;394:1365–1375. doi: https://doi.org/10.1016/S0140-6736(19)31786-6.
Choi J, Ahn A, Kim S, Won CW. Global Prevalence of Physical Frailty by Fried’s Criteria in Community-Dwelling Elderly With National Population-Based Surveys. J Am Med Dir Assoc 2015;16:548–550. doi: https://doi.org/10.1016/j.jamda.2015.02.004.
Liu L-K, Lee W-J, Chen L-Y, Hwang A-C, Lin M-H, Peng L-N, Chen L-K. Association between Frailty, Osteoporosis, Falls and Hip Fractures among Community-Dwelling People Aged 50 Years and Older in Taiwan: Results from I-Lan Longitudinal Aging Study. PLoS One 2015;10:e0136968. doi: https://doi.org/10.1371/journal. pone.0136968.
Ng TP, Feng L, Nyunt MSZ, Feng L, Niti M, Tan BY, Chan G, Khoo SA, Chan SM, Yap P, Yap KB. Nutritional, Physical, Cognitive, and Combination Interventions and Frailty Reversal Among Older Adults: A Randomized Controlled Trial. Am J Med 2015;128:1225–1236.e1. doi: https://doi.org/10.1016/j.amjmed.2015.06.017.
National Bureau of statistics of the people’s Republic of China China Statistical Yearbook — 2020. Available at: http://www.stats.gov.cn/tjsj/ndsj/2020/indexch.htm. Accessed September 30, 2021.
Survey report on the living conditions of the elderly in urban and rural China, 2018. Available at: http://www.raduga.com.cn/skwx_eypt/BookReading.aspx?ID=2715#top. Accessed September 30, 2021.
Dent E, Martin FC, Bergman H, Woo J, Romero-Ortuno R, Walston JD. Management of frailty: opportunities, challenges, and future directions. The Lancet 2019;394:1376–1386. doi: https://doi.org/10.1016/S0140-6736(19)31785-4.
Bandeen-Roche K, Seplaki CL, Huang J, Buta B, Kalyani RR, Varadhan R, Xue Q-L, Walston JD, Kasper JD. Frailty in Older Adults: A Nationally Representative Profile in the United States. J Gerontol A Biol Sci Med Sci 2015;70:1427–1434. doi: https://doi.org/10.1093/gerona/glv133.
Kojima G. Prevalence of Frailty in Nursing Homes: A Systematic Review and Meta-Analysis. J Am Med Dir Assoc 2015;16:940–945. doi: https://doi.org/10.1016/j.jamda.2015.06.025.
Xiaolin H, Jing G, Chenxi W, Dingxi B, Yuping X, Xing L, Xiaoxiao G, Jingya Y. Prevalence and factors associated with frailty among institutional older adults. Chinese Journal of nursing 2018;53:88–93. doi:https://doi.org/10.3761/j.issn.0254-1769.2018.01.016.
Yayi Z, Yaping D, Xianwen L, Yan C. Frailty among institutionalized elderly people in Nanjing city: prevalence and risk factors. Public health in China 2018;34:550–553. doi: https://doi.org/10.11847/zgggws1112389.
van de Rest O, van der Zwaluw NL, Tieland M, Adam JJ, Hiddink GJ, van Loon LJC, de Groot LCPGM. Effect of resistance-type exercise training with or without protein supplementation on cognitive functioning in frail and pre-frail elderly: secondary analysis of a randomized, double-blind, placebo-controlled trial. Mech Ageing Dev 2014;136–137:85–93. doi: https://doi.org/10.1016/j.mad.2013.12.005
Yoon DH, Lee J-Y, Song W. Effects of Resistance Exercise Training on Cognitive Function and Physical Performance in Cognitive Frailty: A Randomized Controlled Trial. J Nutr Health Aging 2018;22:944–951. doi: https://doi.org/10.1007/s12603-018-1090-9.
Tousignant M, Corriveau H, Roy P-M, Desrosiers J, Dubuc N, Hbert R. Efficacy of supervised Tai Chi exercises versus conventional physical therapy exercises in fall prevention for frail older adults: a randomized controlled trial. Disabil Rehabil 2013;35:1429–1435. doi: https://doi.org/10.3109/09638288.2012.737084.
Cadore EL, Casas-Herrero A, Zambom-Ferraresi F, Idoate F, Millor N, Gmez M, Rodriguez-Maas L, Izquierdo M. Multicomponent exercises including muscle power training enhance muscle mass, power output, and functional outcomes in institutionalized frail nonagenarians. Age (Dordr) 2014;36:773–785. doi: https://doi.org/10.1007/s11357-013-9586-z.
Aguirre LE, Villareal DT. Physical Exercise as Therapy for Frailty. Nestle Nutr Inst Workshop Ser 2015;83:83–92. doi: https://doi.org/10.1159/000382065.
Francisco José Tarazona-Santabalbina, Gómez-Cabrera MC, Pérez-Ros P, Martinez-Arnau FM, Cabo H, Tsaparas K, Salvador-Pascual A, Rodriguez-Mañas L, Viña J. A Multicomponent Exercise Intervention that Reverses Frailty and Improves Cognition, Emotion, and Social Networking in the Community-Dwelling Frail Elderly: A Randomized Clinical Trial. J Am Med Dir Assoc 2016;17:426–433. doi: https://doi.org/10.1016/j.jamda.2016.01.019.
Kito N, Matsuo K, Ogawa K, Izumi A, Kishima M, Itoda M, Masuda Y. Positive Effects of “Textured Lunches” Gatherings and Oral Exercises Combined with Physical Exercises on Oral and Physical Function in Older Individuals: A Cluster Randomized Controlled Trial. J Nutr Health Aging 2019;23:669–676. doi: https://doi.org/10.1007/s12603-019-1216-8.
Puffer S, Torgerson DJ, Watson J. Cluster randomized controlled trials. J Eval Clin Pract 2005;11:479–483. doi: https://doi.org/10.1111/j.1365-2753.2005.00568.x.
Campbell MK, Piaggio G, Elbourne DR, Altman DG, CONSORT Group. Consort 2010 statement: extension to cluster randomised trials. BMJ 2012;345:e5661. doi:https://doi.org/10.1136/bmj.e5661
Pezzotti P, Scalmana S, Mastromattei A, Di Lallo D. The accuracy of the MMSE in detecting cognitive impairment when administered by general practitioners: A prospective observational study. BMC Fam Pract 2008;9:29. doi: https://doi.org/10.1186/1471-2296-9-29.
Lan C, Lai JS, Chen SY, Wong MK. Tai Chi Chuan to improve muscular strength and endurance in elderly individuals: a pilot study. Arch Phys Med Rehabil 2000;81:604–607. doi: https://doi.org/10.1016/s0003-9993(00)90042-x.
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, Seeman T, Tracy R, Kop WJ, Burke G, McBurnie MA, Cardiovascular Health Study Collaborative Research Group. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 2001;56:M146–156. doi: https://doi.org/10.1093/gerona/56.3.m146.
Folstein MF, Folstein SE, McHugh PR. ‘Mini-mental state’. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975;12:189–198. doi: https://doi.org/10.1016/0022-3956(75)90026-6.
WHOQOL — Measuring Quality of Life| The World Health Organization Available at: https://www.who.int/tools/whoqol. Accessed October 8, 2021.
Meyer BD. Natural and quasi-experiments in economics. Journal of Business and Economic Statistics 1995;13:151–161. doi: https://doi.org/10.1080/07350015.1995.10524589.
Hartman CA, Manos TM, Winter C, Hartman DM, Li B, Smith JC. Effects of T’ai Chi training on function and quality of life indicators in older adults with osteoarthritis. J Am Geriatr Soc 2000;48:1553–1559. doi: https://doi.org/10.1111/j.1532-5415.2000.tb03863.x.
Yeh GY, Wood MJ, Lorell BH, Stevenson LW, Eisenberg DM, Wayne PM, Goldberger AL, Davis RB, Phillips RS. Effects of tai chi mind-body movement therapy on functional status and exercise capacity in patients with chronic heart failure: a randomized controlled trial. Am J Med 2004;117:541–548. doi: https://doi.org/10.1016/j.amjmed.2004.04.016.
Romera L, Orfila F, Segura JM, Ramirez A, Mller M, Fabra ML, Lancho S, Bastida N, Foz G, Fabregat MA, Mart N, Cullell M, Martinez D, Gin M, Bistuer A, Cendrós P, Pérez E. Effectiveness of a primary care based multifactorial intervention to improve frailty parameters in the elderly: a randomised clinical trial: rationale and study design. BMC Geriatr 2014;14:125. doi: https://doi.org/10.1186/1471-2318-14-125.
Fairhall N, Sherrington C, Kurrle SE, Lord SR, Lockwood K, Howard K, Hayes A, Monaghan N, Langron C, Aggar C, Cameron ID. Economic evaluation of a multifactorial, interdisciplinary intervention versus usual care to reduce frailty in frail older people. J Am Med Dir Assoc 2015;16:41–48. doi: https://doi.org/10.1016/j.jamda.2014.07.006.
Fairhall N, Sherrington C, Lord SR, Kurrle SE, Langron C, Lockwood K, Monaghan N, Aggar C, Cameron ID. Effect of a multifactorial, interdisciplinary intervention on risk factors for falls and fall rate in frail older people: a randomised controlled trial. Age Ageing 2014;43:616–622. doi: https://doi.org/10.1093/ageing/aft204.
de Labra C, Guimaraes-Pinheiro C, Maseda A, Lorenzo T, Mill n-Calenti JC. Effects of physical exercise interventions in frail older adults: a systematic review of randomized controlled trials. BMC Geriatr 2015;15:154. doi: https://doi.org/10.1186/s12877-015-0155-4.
Vogler CM, Sherrington C, Ogle SJ, Lord SR. Reducing risk of falling in older people discharged from hospital: a randomized controlled trial comparing seated exercises, weight-bearing exercises, and social visits. Arch Phys Med Rehabil 2009;90:1317–1324. doi: https://doi.org/10.1016/j.apmr.2009.01.030.
Cordes T, Bischoff LL, Schoene D, et al. A multicomponent exercise intervention to improve physical functioning, cognition and psychosocial well-being in elderly nursing home residents: a study protocol of a randomized controlled trial in the PROCARE (prevention and occupational health in long-term care) project. BMC Geriatr 2019;19:369. doi: https://doi.org/10.1186/s12877-019-1386-6
Cadore EL, Rodrguez-Maas L, Sinclair A, Izquierdo M. Effects of Different Exercise Interventions on Risk of Falls, Gait Ability, and Balance in Physically Frail Older Adults: A Systematic Review. Rejuvenation Research 2013;16:105–114. doi: https://doi.org/10.1089/rej.2012.1397.
Haider S, Grabovac I, Dorner TE. Effects of physical activity interventions in frail and prefrail community-dwelling people on frailty status, muscle strength, physical performance and muscle mass—a narrative review. Wien Klin Wochenschr 2019;131:244–254. doi: https://doi.org/10.1007/s00508-019-1484-7.
Langlois F, Vu TTM, Chass K, Dupuis G, Kergoat M-J, Bherer L. Benefits of Physical Exercise Training on Cognition and Quality of Life in Frail Older Adults. The Journals of Gerontology: Series B 2013;68:400–404. doi: https://doi.org/10.1093/geronb/gbs069.
Campbell E, Petermann-Rocha F, Welsh P, Celis-Morales C, Pell JP, Ho FK, Gray SR. The effect of exercise on quality of life and activities of daily life in frail older adults: A systematic review of randomised control trials. Exp Gerontol 2021;147:111287. doi: https://doi.org/10.1016/j.exger.2021.111287.
Li P-S, Hsieh C-J, Miao N-F. A Study of Physical Activity, Frailty, and Health-Related Quality of Life Among Community-Dwelling Older Adults in Taiwan. J Nurs Res 2020;28:e124. doi: https://doi.org/10.1097/JNR.0000000000000402.
Sartor-Glittenberg C, Lehmann S, Okada M, Rosen D, Brewer K, Bay RC. Variables explaining health-related quality of life in community-dwelling older adults. J Geriatr Phys Ther 2014;37:83–91. doi: https://doi.org/10.1519/JPT.0b013e3182a4791b.
Van Dyck D, Teychenne M, McNaughton SA, De Bourdeaudhuij I, Salmon J. Relationship of the perceived social and physical environment with mental healthrelated quality of life in middle-aged and older adults: mediating effects of physical activity. PLoS One 2015;10:e0120475. doi: https://doi.org/10.1371/journal.pone.0120475.
Halaweh H, Willen C, Grimby-Ekman A, Svantesson U. Physical Activity and Health-Related Quality of Life Among Community Dwelling Elderly. J Clin Med Res 2015;7:845–852. doi: https://doi.org/10.14740/jocmr2307w.
Renne I, Gobbens RJ. Effects of frailty and chronic diseases on quality of life in Dutch community-dwelling older adults: a cross-sectional study. Clin Interv Aging 2018;13:325–334. doi: https://doi.org/10.2147/CIA.S156116.
Kanauchi M, Kubo A, Kanauchi K, Saito Y. Frailty, health-related quality of life and mental well-being in older adults with cardiometabolic risk factors. Int J Clin Pract 2008;62:1447–1451. doi: https://doi.org/10.1111/j.1742-1241.2008.01830.x.
Acknowledgments
The authors are thankful to the support, coordination and cooperation from the nurses, trainers and principals of the 8 local elderly nursing homes, and sample elderly for their participation. We also gratefully acknowledge the members of our team for excellent assistance. This research was funded by Japan-China Medical Association Foundation Project, Heilongjiang Province Education Science «14th Five-year plan» 2021 Key Project (Project Approval Number: GJB1421328), and Heilongjiang Natural Science Foundation Project (Project Approval Number: LH2020H083).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study has been approved by the Institutional Review Board of Heilongjiang University of Chinese Medicine (protocol number: 2020-K131). Prior to the start of the study, we explained the purpose and methods of the study to the participants and sought the written informed consent of all study participants.
Additional information
Conflict of Interest
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Liu, T., Wang, C., Sun, J. et al. The Effects of an Integrated Exercise Intervention on the Attenuation of Frailty in Elderly Nursing Homes: A Cluster Randomized Controlled Trail. J Nutr Health Aging 26, 222–229 (2022). https://doi.org/10.1007/s12603-022-1745-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-022-1745-4