Abstract
Objectives
Assessment of the progression of abdominal aortic calcification (AAC) may be a surrogate marker of the impact of physical function on cardiovascular risk. Our aim was to assess the risk of rapid AAC progression in older men with low relative appendicular lean mass (RALM) and poor physical function.
Design
Prospective cohort study.
Setting
Community-dwelling older men.
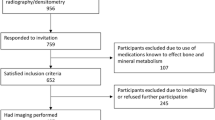
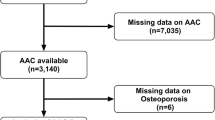
Participants
621 men aged 50–85 followed prospectively (baseline, 3 and 7.5 years).
Measurements
Body composition was assessed by DXA. Poor physical function was defined as incapacity to perform ≥1 of 5 clinical tests (balance, muscle strength). AAC was assessed using Kauppila’s semiquantitative score. Reclassification improvement was assessed by comparing the areas under the curve (AUC) using DeLong’s method.
Results
Rapid AAC progression (>0.6 point/year) was found in 168 men (27.1%). After adjustment for confounders including baseline AAC, the risk of rapid AAC progression increased with lower RALM (OR=1.42/SD, 95%CI: 1.09–1.86, p<0.01) and was higher in the lowest (<7.5kg/m2) vs. highest (>8.6kg/m2) quartile (OR=2.15, 95%CI: 1.17–3.95, p<0.01). Poor physical performance was associated with rapid AAC progression (OR=2.76, 95%CI: 1.48–5.91, p<0.005). Low RALM (<7.84kg/m2 defined using Youden’s index) and poor physical function contributed to the risk of rapid AAC progression jointly. Men who had low RALM and poor physical function had higher risk of rapid AAC progression vs. men without these traits (OR=4.66, 95%CI: 1.72–12.62, p<0.05). RALM and physical function improved the identification of men with rapid AAC progression (AAUC=0.026, 95%CI: 0.005–0.046, p<0.05) after adjustment for confounders including baseline AAC score.
Conclusions
Low RALM and poor physical function are associated with higher risk of rapid AAC progression and possibly represent another measure of cardiovascular risk.

Similar content being viewed by others
References
Leow K, Szulc P, Schousboe JT et al. Prognostic Value of Abdominal Aortic Calcification: A Systematic Review and Meta-Analysis of Observational Studies. J Am Heart Assoc 2021;10:e017205. doi: https://doi.org/10.1161/JAHA.120.017205
Lewis JR, Wong G, Taverniti A, Vucak-Dzumhur M, Elder GJ. Association between Aortic Calcification, Cardiovascular Events, and Mortality in Kidney and Pancreas-Kidney Transplant Recipients. Am J Nephrol 2019;50:177–186. doi: https://doi.org/10.1159/000502328.
Oishi H, Horibe H, Yamase Y et al. Predictive value of abdominal aortic calcification index for mid-term cardiovascular events in patients with acute coronary syndrome. Heart Vessels 2020;35:620–629. doi: https://doi.org/10.1007/s00380-019-01527-6.
Schousboe JT, Taylor BC, Kiel DP, Ensrud KE, Wilson KE, McCloskey EV. Abdominal aortic calcification detected on lateral spine images from a bone densitometer predicts incident myocardial infarction or stroke in older women. J Bone Miner Res 2008;23:409–16. doi: https://doi.org/10.1359/jbmr.071024.
Wannamethee SG, Shaper AG, Lennon L, Whincup PH. Decreased muscle mass and increased central adiposity are independently related to mortality in older men. Am J Clin Nutr. 2007 86:1339–46. doi: https://doi.org/10.1093/ajcn/86.5.1339.
Keevil VL, Luben R, Hayat S, Sayer AA, Wareham NJ, Khaw KT. Physical capability predicts mortality in late mid-life as well as in old age: Findings from a large British cohort study. Arch Gerontol Geriatr. 2018 74:77–82. doi: https://doi.org/10.1016/j.archger.2017.10.001.
Leong DP, Teo KK, Rangarajan S et al. Prognostic value of grip strength: findings from the Prospective Urban Rural Epidemiology (PURE) study. Lancet. 2015 386:266–73. doi: https://doi.org/10.1016/S0140-6736(14)62000-6.
Brown JC, Harhay MO, Harhay MN. Sarcopenia and mortality among a population-based sample of community-dwelling older adults. J Cachexia Sarcopenia Muscle. 2016 7:290–8. doi: https://doi.org/10.1002/jcsm.12073.
Szulc P, Munoz F, Marchand F, Chapurlat R, Delmas PD. Rapid loss of appendicular skeletal muscle mass is associated with higher all-cause mortality in older men: the prospective MINOS study. Am J Clin Nutr 2010;91:1227–36. doi: https://doi.org/10.3945/ajcn.2009.28256.
Newman AB, Simonsick EM, Naydeck BL et al. Association of long-distance corridor walk performance with mortality, cardiovascular disease, mobility limitation, and disability. JAMA. 2006 295:2018–26. doi: https://doi.org/10.1001/jama.295.17.2018.
Lopez-Jaramillo P, Cohen DD, Gómez-Arbeláez D et al. Association of handgrip strength to cardiovascular mortality in pre-diabetic and diabetic patients: a subanalysis of the ORIGIN trial. Int J Cardiol. 2014 174:458–61. doi: https://doi.org/10.1016/j.ijcard.2014.04.013.
Chun S, Shin DW, Han K et al. The Timed Up and Go test and the ageing heart: Findings from a national health screening of 1,084,875 community-dwelling older adults. Eur J Prev Cardiol. 2019;2047487319882118. doi: https://doi.org/10.1177/2047487319882118.
Pavasini R, Serenelli M, Celis-Morales CA et al. Grip strength predicts cardiac adverse events in patients with cardiac disorders: an individual patient pooled meta-analysis. Heart. 2019 105:834–841. doi: https://doi.org/10.1136/heartjnl-2018-313816.
Lee HS, Park KW, Kang J et al. Sarcopenia Index as a Predictor of Clinical Outcomes in Older Patients with Coronary Artery Disease. J Clin Med 2020;9:3121. doi: https://doi.org/10.3390/jcm9103121.
Campo G, Maietti E, Tonet E et al. The Assessment of Scales of Frailty and Physical Performance Improves Prediction of Major Adverse Cardiac Events in Older Adults with Acute Coronary Syndrome. J Gerontol A Biol Sci Med Sci. 2020;75:1113–1119. doi: https://doi.org/10.1093/gerona/glz123.
Sousa N, Mendes R, Abrantes C, Sampaio J, Oliveira J. A randomized 9-month study of blood pressure and body fat responses to aerobic training versus combined aerobic and resistance training in older men. Exp Gerontol. 2013 48:727–33. doi: https://doi.org/10.1016/j.exger.2013.04.008.
Kemmler W, Kohl M, von Stengel S, Schoene D. Effect of high-intensity resistance exercise on cardiometabolic health in older men with osteosarcopenia: the randomised controlled Franconian Osteopenia and Sarcopenia Trial (FrOST). BMJ Open Sport Exerc Med. 2020 6:e000846. doi: https://doi.org/10.1136/bmjsem-2020-000846.
Saeidifard F, Medina-Inojosa JR, West CP et al. The association of resistance training with mortality: A systematic review and meta-analysis. Eur J Prev Cardiol. 2019 26:1647–1665. doi: https://doi.org/10.1177/2047487319850718.
Sanchis-Gomar F, Lavie CJ, Marín J et al. Exercise Effects On Cardiovascular Disease: From Basic Aspects To Clinical Evidence. Cardiovasc Res. 2021 cvab272. doi: https://doi.org/10.1093/cvr/cvab272.Online.
Barua RS, Ambrose JA. Mechanisms of coronary thrombosis in cigarette smoke exposure. Arterioscler Thromb Vasc Biol 2013;33:1460–7. doi: https://doi.org/10.1161/ATVBAHA.112.300154.
Bendix EF, Johansen E, Ringgaard T, Wolder M, Starup-Linde J. Diabetes and Abdominal Aortic Calcification-a Systematic Review. Curr Osteoporos Rep 2018;16:42–57. doi: https://doi.org/10.1007/s11914-018-0418-z.
Naves-Díaz M, Cabezas-Rodríguez I, Barrio-Vázquez S, Fernández E, Díaz-López JB, Cannata-Andía JB. Low calcidiol levels and risk of progression of aortic calcification. Osteoporos Int 2012;23:1177–82. doi: https://doi.org/10.1007/s00198-011-1550-0.
Renoud A, Ecochard R, Marchand F, Chapurlat R, Szulc P. Predictive parameters of accelerated muscle loss in men-MINOS study. Am J Med 2014;127:554–61. doi: https://doi.org/10.1016/j.amjmed.2014.02.004.
van Setten J, Isgum I, Smolonska J et al. Genome-wide association study of coronary and aortic calcification implicates risk loci for coronary artery disease and myocardial infarction. Atherosclerosis 2013;228:400–5. doi: https://doi.org/10.1016/j.atherosclerosis.2013.02.039.
Kim ED, Kim JS, Kim SS et al. Association of abdominal aortic calcification with lifestyle and risk factors of cardiovascular disease. Korean J Fam Med 2013;34:213–20. doi: https://doi.org/10.4082/kjfm.2013.34.3.213.
Hak AE, Witteman JCM, de Jong FH, Geerlings MI, Hofman A, Pols HAP. Low levels of endogenous androgens increase the risk of atherosclerosis in elderly men: the Rotterdam study. J Clin Endocrinol Metab 2002;87:3632–9. doi: https://doi.org/10.1210/jcem.87.8.8762.
Alexandersen P, Tankó LB, Bagger YZ, Jespersen J, Skouby SO, Christiansen C. Associations between aortic calcification and components of body composition in elderly men. Obesity 2006;14:1571–8. doi: https://doi.org/10.1038/oby.2006.181.
Idoate F, Cadore E, Casas-Herrero A et al. Noncoronary Vascular Calcification, Bone Mineral Density, and Muscle Mass in Institutionalized Frail Nonagenarians. Rejuvenation Res 2017;20:298–308. doi: https://doi.org/10.1089/rej.2016.1868.
Jensky NE, Criqui MH, Wright CM, Wassel CL, Alcaraz JE, Allison MA. The association between abdominal body composition and vascular calcification. Obesity 2011;19:2418–24. doi: https://doi.org/10.1038/oby.2011.70.
Ramírez-Vélez R, García-Hermoso A, Correa-Rodríguez M, Lobelo F, González-Ruiz K, Izquierdo M. Abdominal aortic calcification is associated with decline in handgrip strength in the U.S. adult population 40 years of age. Nutr Metab Cardiovasc Dis. 2020 S0939-4753(20)30479-8. doi: https://doi.org/10.1016/j.numecd.2020.11.003.
Ko BJ, Chang Y, Jung HS et al. Relationship Between Low Relative Muscle Mass and Coronary Artery Calcification in Healthy Adults. Arterioscler Thromb Vasc Biol 2016;36:1016–21. doi: https://doi.org/10.1161/ATVBAHA.116.307156.
Crawford MA, Criqui MH, Forbang N, Unkart JT, Allison M, Larsen BA. Associations of abdominal muscle area and density with coronary artery calcium volume and density: The multi-ethnic study of atherosclerosis. Metabolism 2020;107:154230. doi: https://doi.org/10.1016/j.metabol.2020.154230.
Lee SY, Chao CT, Huang JW, Huang KC. Vascular calcification as an underrecognized risk factor for frailty in 1783 community-dwelling elderly individuals. J Am Heart Assoc 2020;9:e017308. doi: https://doi.org/10.1161/JAHA.120.017308.
Hamer M, Kivimaki M, Lahiri A et al. Walking speed and subclinical atherosclerosis in healthy older adults: the Whitehall II study. Heart 2010;96:380–4. doi: https://doi.org/10.1136/hrt.2009.183350.
Szulc P, Samelson EJ, Kiel DP, Delmas PD. Increased bone resorption is associated with increased risk of cardiovascular events in men: the MINOS study. J Bone Miner Res 2009;24:2023–31. doi: https://doi.org/10.1359/jbmr.090531.
Kauppila LI, Polak JF, Cupples LA, Hannan MT, Kiel DP, Wilson PW. New indices to classify location, severity and progression of calcific lesions in the abdominal aorta: a 25-year follow-up study. Atherosclerosis 1997;132:245–50. doi: https://doi.org/10.1016/s0021-9150(97)00106-8.
Nevitt MC, Cummings SR, Kidd S, Black D. Risk factors for recurrent non-syncopal falls. A prospective study. JAMA 1989;261:2663–2668. doi: https://doi.org/10.1001/jama.261.18.2663
Guralnik JM, Ferruci L, Simonsick EM, Salive ME, Wallace RB Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. N Engl J Med 1995;332:556–561. doi: https://doi.org/10.1056/NEJM199503023320902.
Tinetti ME, Ginter SF Identifying mobility dysfunctions in elderly patients. Standard neuromuscular examination or direct assessment? JAMA 1988;259:1190–1193. doi: https://doi.org/10.1001/jama.259.8.1190
Szulc P, Maurice C, Marchand F, Delmas PD. Increased bone resorption is associated with higher mortality in community-dwelling men >or=50 years of age: the MINOS study J Bone Miner Res 2009;24:1116–24. doi: https://doi.org/10.1359/jbmr.081251.
Confavreux CB, Szulc P, Casey R et al. Higher serum osteocalcin is associated with lower abdominal aortic calcification progression and longer 10-year survival in elderly men of the MINOS cohort. J Clin Endocrinol Metab 2013;98:1084–92. doi: https://doi.org/10.1210/jc.2012-3426.
Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 1972;18: 499–502.
Vermeulen A, Verdonck L, Kaufman JM. A critical evaluation of simple methods for the estimation of free testosterone in serum. J Clin Endocrinol Metab 1999;84:3666–72. doi: https://doi.org/10.1210/jcem.84.10.6079
Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med 2009;150:604–12. doi: https://doi.org/10.7326/0003-4819-150-9-200905050-00006
Komori T. Functions of Osteocalcin in Bone, Pancreas, Testis, and Muscle. Int J Mol Sci 2020 21:7513. doi: https://doi.org/10.3390/ijms21207513
Minn YK, Suk SH. Higher skeletal muscle mass may protect against ischemic stroke in community-dwelling adults without stroke and dementia: The PRESENT project. BMC Geriatr 2017;17:45. doi: https://doi.org/10.1186/s12877-017-0433-4.
Ochi M, Kohara K, Tabara Y et al. Arterial stiffness is associated with low thigh muscle mass in middle-aged to elderly men. Atherosclerosis 2010 212:327–32. doi: https://doi.org/10.1016/j.atherosclerosis.2010.05.026.
Imran TF, Patel Y, Ellison RC et al. Walking and Calcified Atherosclerotic Plaque in the Coronary Arteries: The National Heart, Lung, and Blood Institute Family Heart Study. Arterioscler Thromb Vasc Biol 2016;36:1272–7. doi: https://doi.org/10.1161/ATVBAHA.116.307284.
Westerhof N, Lankhaar JW, Westerhof BE. The arterial Windkessel. Med Biol Eng Comput 2009;47:131–41. doi: https://doi.org/10.1007/s11517-008-0359-2.
Lu Y, Cheng Z, Zhao Y et al Efficacy and safety of long-term treatment with statins for coronary heart disease: A Bayesian network meta-analysis. Atherosclerosis 2016;254:215–227. doi: https://doi.org/10.1016/j.atherosclerosis.2016.10.025.
Saremi A, Bahn G, Reaven PD. Progression of vascular calcification is increased with statin use in the Veterans Affairs Diabetes Trial (VADT). Diabetes Care 2012;35:2390–2. doi: https://doi.org/10.2337/dc12-0464.
Zhang X, Li Y, Yang P et al. Trimethylamine-N-oxide promotes vascular calcification through activation of NLRP3 (Nucleotide-Binding Domain, Leucine-Rich-Containing Family, Pyrin Domain-Containing-3) Inflammasome and NF-kappaB (Nuclear Factor kappaB) Signals. Arterioscler Thromb Vasc Biol 2020;40:751–765. doi: https://doi.org/10.1161/ATVBAHA.119.313414.
Szulc P. Abdominal aortic calcification: A reappraisal of epidemiological and pathophysiological data. Bone 2016;84:25–37. doi: https://doi.org/10.1016/j.bone.2015.12.004.
Jeon YK, Shin MJ, Saini SK et al. Vascular dysfunction as a potential culprit of sarcopenia. Exp Gerontol. 2021 145:111220. doi: https://doi.org/10.1016/j.exger.2020.111220.
Watanabe H, Enoki Y, Maruyama T. Sarcopenia in Chronic Kidney Disease: Factors, Mechanisms, and Therapeutic Interventions. Biol Pharm Bull. 2019;42:1437–1445. doi: https://doi.org/10.1248/bpb.b19-00513.
Acknowledgements
Authors’ roles: Funding acquisition: PS. Study design and conceptualization: PS, RC. Study conduct: PS. Data collection: PS. Data analysis: PS. Data interpretation: PS, RC. Drafting manuscript: PS. Revising manuscript content and editing: PS, RC. Approving final version of manuscript: PS, RC. PS takes responsibility for the integrity of the data analysis. Sponsor’s role: The funding organization did not have access to the data, nor was involved in any analysis of this study.
Funding
Funding: Grants from INSERM/Merck Sharp & Dohme Chibret, France.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical standard: The protocol of the MINOS study complied with the law in France which was valid when the study was performed.
Conflict of interest: All the authors have no conflict of interest concerning this study.
Additional information
Abstract presented: (plenary oral) during the 47th European Calcified Tissue Society Congress, 2020, doi:10.1016/j.bonr.2020.100323.
Electronic supplementary material
Supplementary Table 1
Comparison of men who were or were not followed up
Supplemental Table 2
Bivariate comparisons according to the quartiles of the progression of the abdominal aortic calcification (AAC) in 621 men
Suppl. Figure 1
Average (median, interquartile range) yearly progression of abdominal aortic calcification per age group.
Rights and permissions
About this article
Cite this article
Szulc, P., Chapurlat, R. Rapid Progression of Aortic Calcification in Older Men with Low Appendicular Lean Mass and Poor Physical Function. J Nutr Health Aging 25, 1217–1225 (2021). https://doi.org/10.1007/s12603-021-1697-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-021-1697-0