Abstract
Objectives
According to the recently proposed diagnostic criteria for sarcopenic dysphagia, sarcopenic dysphagia can be classified as probable or possible based on tongue pressure. However, it is unclear whether patients with probable and possible sarcopenic dysphagia have different characteristics. Therefore, this study aimed to investigate whether patients with possible and probable sarcopenic dysphagia have different clinical characteristics.
Design
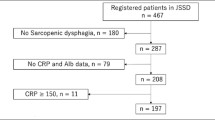
A cross-sectional study. Setting: A rehabilitation hospital. PARTICIPANTS: In total, 129 patients aged ≥65 years with sarcopenic dysphagia were included.
Methods
A tongue pressure of <20 kPa was indicative of probable sarcopenic dysphagia, and a tongue pressure of ≥20 kPa was indicative of possible sarcopenic dysphagia. Kuchi-Kara Taberu (KT) index scores were compared between the probable or possible sarcopenic dysphagia groups.
Results
According to the tongue pressure, 76 and 53 patients were classified into the probable and possible sarcopenic dysphagia groups, respectively. In multiple linear regression analysis, the presence of probable sarcopenic dysphagia was independently associated with the total KT index score (standardized coefficient: −0.313, regression coefficient: −4.500, 95% confidence interval [CI], −6.920 to −2.080, P < 0.001). The presence of probable sarcopenic dysphagia was independently associated with some subitems of the KT index (willingness to eat, cognitive function while eating, oral preparatory and propulsive phase, severity of pharyngeal dysphagia, eating behavior, and daily living activities).
Conclusions
Patients with probable sarcopenic dysphagia were characterized by poor overall eating-related conditions, especially poor swallowing ability, ability to perform activities of daily living, and nutritional status.
Similar content being viewed by others
References
Ortega O, Martín A, Clavé P. Diagnosis and management of oropharyngeal dysphagia among older persons, state of the art. J Am Med Dir Assoc 2017;18:576–582.
Fujishima I, Fujiu-Kurachi M, Arai H, Hyodo M, Kagaya H, Maeda K, Mori T, Nishioka S, Oshima F, Ogawa S, Ueda K, Umezaki T, Wakabayashi H, Yamawaki M, Yoshimura Y. Sarcopenia and dysphagia: position paper by four professional organizations. Geriatr Gerontol Int 2019;19:91–97.
Maeda K, Akagi J. Sarcopenia is an independent risk factor of dysphagia in hospitalized older people. Geriatr Gerontol Int 2016;16:515–521.
Nagano A, Maeda K, Shimizu A, Nagami S, Takigawa N, Ueshima J, Suenaga M. Association of sarcopenic dysphagia with underlying sarcopenia following hip fracture surgery in older women. Nutrients 2020;12. doi:https://doi.org/10.3390/nu12051365.
Maeda K, Takaki M, Akagi J. Decreased skeletal muscle mass and risk factors of sarcopenic dysphagia: a prospective observational cohort study. J Gerontol A Biol Sci Med Sci 2017;72:1290–1294.
Maeda K, Ishida Y, Nonogaki T, Shimizu A, Yamanaka Y, Matsuyama R, Kato R, Mori N. Development and predictors of sarcopenic dysphagia during hospitalization of older adults. Nutrients 2019;12. doi:https://doi.org/10.3390/nu12010070.
Wakabayashi H, Takahashi R, Murakami T. The prevalence and prognosis of sarcopenic dysphagia in patients who require dysphagia rehabilitation. J Nutr Health Aging 2019;23:84–88.
Shimizu A, Fujishima I, Maeda K, Wakabayashi H, Nishioka S, Ohno T, Nomoto A, Kayashita J, Mori N, the Japanese Working Group on Sarcopenic Dysphagia. Nutritional management enhances the recovery of swallowing ability in older patients with sarcopenic dysphagia. Nutrients 2021;13:596.
Mori T, Fujishima I, Wakabayashi H, Oshima F, Itoda M, Kunieda K, Kayashita J, Nishioka S, Sonoda A, Kuroda Y, Yamada M, Ogawa S. Development, reliability, and validity of a diagnostic algorithm for sarcopenic dysphagia. JCSM Clin Rep 2017;2:1–10.
Shimizu A, Maeda K, Nagami S, Nagano A, Yamada Y, Shimizu M, Ishida Y, Kayashita J, Fujishima I, Mori N, Murotani K, Suenaga M. Low tongue strength is associated with oral and cough-related abnormalities in older inpatients. Nutrition 2020;83:111062.
Namasivayam-MacDonald AM, Morrison JM, Steele CM, Keller H. How swallow pressures and dysphagia affect malnutrition and mealtime outcomes in long-term care. Dysphagia 2017;32:785–796.
Sakai K, Nakayama E, Tohara H, Maeda T, Sugimoto M, Takehisa T, Takehisa Y, Ueda K. Tongue strength is associated with grip strength and nutritional status in older adult inpatients of a rehabilitation hospital. Dysphagia 2017;32:241–249.
Maeda K, Akagi J. Decreased tongue pressure is associated with sarcopenia and sarcopenic dysphagia in the elderly. Dysphagia 2015;30:80–87.
Maeda K, Shamoto H, Wakabayashi H, Enomoto J, Takeichi M, Koyama T. Reliability and validity of a simplified comprehensive assessment tool for feeding support: kuchi-kara taberu index. J Am Geriatr Soc 2016;64:e248–e252.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987;40:373–383.
Kaiser MJ, Bauer JM, Ramsch C, Uter W, Guigoz Y, Cederholm T, Thomas DR, Anthony P, Charlton KE, Maggio M, Tsai AC, Grathwohl D, Vellas B, Sieber CC, MNA-International Group. Validation of the Mini Nutritional Assessment short-form (MNA-SF): a practical tool for identification of nutritional status. J Nutr Health Aging 2009;13:782–788.
Perneczky R, Wagenpfeil S, Komossa K, Grimmer T, Diehl J, Kurz A. Mapping scores onto stages: Mini-Mental State Examination and clinical dementia rating. Am J Geriatr Psychiatry 2006;14:139–144.
Kidd D, Stewart G, Baldry J, Johnson J, Rossiter D, Petruckevitch A, Thompson AJ. The Functional Independence Measure: a comparative validity and reliability study. Disabil Rehabil 1995;17:10–14.
Chen L-K, Woo J, Assantachai P, et al. Asian Working Group for Sarcopenia: 2019 consensus update on sarcopenia diagnosis and treatment. J Am Med Dir Assoc 2020;21:300–307.e2.
Kunieda K, Ohno T, Fujishima I, Hojo K, Morita T. Reliability and validity of a tool to measure the severity of dysphagia: the Food Intake LEVEL Scale. J Pain Symptom Manage 2013;46:201–206.
Waza M, Maeda K, Katsuragawa C, Sugita A, Tanaka R, Ohtsuka A, Matsui T, Kitagawa K, Kishimoto T, Fukui H, Kawai K, Yamamoto M, Isono M. Comprehensive tool to assess oral feeding support for functional recovery in post-acute rehabilitation. J Am Med Dir Assoc 2019;20:426–431.
Cohen J. A power primer. Psychol Bull 1992;112:155–159.
Nakazawa Y, Kikutani T, Igarashi K, Yajima Y, Tamura F. Associations between tongue strength and skeletal muscle mass under dysphagia rehabilitation for geriatric out patients. J Prosthodont Res 2020;64:188–192.
Hara K, Tohara H, Kenichiro K, Yamaguchi K, Ariya C, Yoshimi K, Nakane A, Minakuchi S. Association between tongue muscle strength and masticatory muscle strength. J Oral Rehabil 2019;46:134–139.
Ono T, Kumakura I, Arimoto M, Hori K, Dong J, Iwata H, Nokubi T, Tsuga K, Akagawa Y. Influence of bite force and tongue pressure on oro-pharyngeal residue in the elderly. Gerodontology 2007;24:143–150.
Namasivayam AM, Steele CM, Keller H. The effect of tongue strength on meal consumption in long term care. Clin Nutr 2016;35:1078–1083.
Shimizu A, Maeda K, Koyanagi Y, Kayashita J, Fujishima I, Mori N. The Global Leadership Initiative on Malnutrition-Defined Malnutrition Predicts Prognosis in Persons With Stroke-Related Dysphagia. J Am Med Dir Assoc 2019;20:1628–1633.
Acknowledgments
This research was supported by a research grant from Japanese Society of Dysphagia Rehabilitation (Shimizu A) and Research Funding of Longevity Sciences (Grant number: 20–57) of the Ministry of Health, Labour and Welfare of Japan (Maeda K). The authors would like thank the following members of the Japanese Working Group on Sarcopenic Dysphagia for their dedicated guidance: Takashi Mori, Department of Oral and Maxillofacial Surgery, Southern Tohoku General Hospital; Dr. Masataka Itoda, Department of Oral Rehabilitation, Osaka Dental University Hospital; Dr. Nami Ogawa, Department of Dysphagia Rehabilitation, Tokyo Medical and Dental University; Dr. Fumiko Oshima, Department of Rehabilitation Medicine, Suwa Red Cross Hospital; Dr. Kenjiro Kunieda, Department of Neurology, Gifu University Graduate School of Medicine Takashi Shigematsu, Department of Rehabilitation Medicine, Hamamatsu City Rehabilitation Hospital; Dr. Minoru Yamada, Graduate School of Comprehensive Human Sciences, University of Tsukuba; Dr. Sumito Ogawa, Department of Geriatric Medicine, Graduate School of Medicine, University of Tokyo; Dr. Kazuki Fukuma, Department of Neurology, National Cerebral and Cardiovascular Center; Dr. Ai Hirano, Department of Otolaryngology and Head and Neck Surgery, Tohoku University Graduate School of Medicine; and Dr. Keishi Okamoto, Department of Rehabilitation, Hamamatsu City Rehabilitation Hospital.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Ethical standards: This study was performed in accordance with the ethical standards of the Declaration of Helsinki 1964 and its later amendments.
Conflict of Interest: The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Shimizu, A., Maeda, K., Wakabayashi, H. et al. Sarcopenic Dysphagia with Low Tongue Pressure Is Associated with Worsening of Swallowing, Nutritional Status, and Activities of Daily Living. J Nutr Health Aging 25, 883–888 (2021). https://doi.org/10.1007/s12603-021-1641-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-021-1641-3