Abstract
Background
Parkinson’s Disease (PD) and sarcopenia share a number of common pathways, and they can potentially affect each other.
Objective
We aimed to investigate the relationship between dysphagia and sarcopenia in elderly patients with PD compared to healthy controls.
Methods
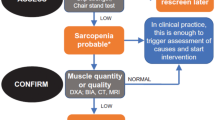
This case-control study was conducted on 54 elderly PD patients and age-, sex- and body mass index-matched 54 healthy elder persons. Demographic and disease characteristics such as disease duration, stage of disease and Unified Parkinson’s disease rating scale were recorded. All subjects were assessed by 10- item Eating Assessment Tool, Gugging Swallowing Screen tests and flexible fiberoptic endoscopic evaluation of swallowing (FEES) as well as Mini nutritional test short form. Also, A simplified screening tool for assessing sarcopenia (SARC-F), five times sit-to-stand and gait speed tests as well as lumbar magnetic resonance imaging (MRI) cross-sectional area of psoas and paraspinal muscles were used for evaluation of sarcopenia. Patients were divided as «with normal swallowing» or «with dysphagia» according to the FEES results. Three groups were compared among themselves in terms of evaluation methods.
Results
Sarcopenia evaluation parameters were significantly higher in patient groups compared to the control group. Moreover, muscle measurements evaluated by MRI in patients with dysphagia are lower than both patients with normal swallowing and control group (p value between 0.001 and 0.011).
Conclusions
Patients with PD have lower muscle mass compared to healthy controls, and the situation is more pronounced in dysphagic PD patients.
Similar content being viewed by others
References
Dorsey ER, Constantinescu R, Thompson JP, et al. Projected number of people with Parkinson disease in the most populous nations, 2005 through 2030. Neurology. 2007;68:384–86.
Pringsheim T, Jette N, Frolkis A, Steeves TD. The prevalence of Parkinson’s disease: a systematic review and meta-analysis. J Mov Disord. 2014;29:1583–1590.
Nienstedt JC, Bihler M, Niessen A, et al. Predictive clinical factors for penetration and aspiration in Parkinson’s disease. Neurogastroenterol Motil. 2019;31(3):e13524.
Umay E, Ozturk E, Gurcay E, Delibas O, Celikel F. Swallowing in Parkinson’s disease: How is it affected? Clin Neurol Neurosurg. 2019;177:37–41.
Katunina E, Titova N. The Epidemiology of Nonmotor Symptoms in Parkinson’s Disease (Cohort and Other Studies). Int Rev Neurobiol. 2017;133:91–110.
Umay E, Eyigor S, Karahan AY, et al. Which swallowing difficulty of food consistency is best predictor for oropharyngeal dysphagia risk in older person? Eur Geriatr Med. 2019;10:609–617.
Bianchetti A, Novelli A. Sarcopenia in the elderly: from clinical aspects to therapeutic options. Geriatric Care. 2019;5(1). https://doi.org/10.4081/gc.2019.8033.
Cruz-Jentoft AJ, Bahat G, Bauer J, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019;48(1):16–31.
Vetrano DL, Pisciotta MS, Laudisio A, et al. Sarcopenia in Parkinson Disease: Comparison of Different Criteria and Association With Disease Severity. J Am Med Dir Assoc.2018;19(6):523–527.
Paul BS, Singh T, Paul G, et al. Prevalence of Malnutrition in Parkinson’s Disease and Correlation with Gastrointestinal Symptoms. Ann Indian Acad Neurol. 2019;22(4):447–452.
Goetz CG, Tilley BC, Shaftman SR, et al. Movement Disorder Society-sponsored revision of the Unified Parkinson’s Disease Rating Scale (MDS-UPDRS): scale presentation and clinimetric testing results. J Mov Disord. 2008;23:2129–70.
Goetz CG, Poewe W, Rascol O, et al. Movement Disorder Society Task Force on rating scales for Parkinson’s disease. Movement Disorder Society Task Force report on the Hoehn and Yahr staging scale: status and recommendations. J Mov Disord. 2004;19:1020–28.
Belafsky PC, Mouadeb DA, Rees CJ, et al. Validity and reliability of the Eating Assessment Tool (EAT-10). Ann Otol Rhinol Laryngol.2008;117: 919–24.
Trapl M, Enderle P, Nowotny M, et al. Dysphagia bedside screening for acute-stroke patients: the Gugging Swallowing Screen. Stroke. 2007;38:2948–52.
Umay E, Eyigor S, Karahan AY, et al. The GUSS test as a good indicator to evaluate dysphagia in healthy older people: a multicenter reliability and validity study. Eur Geriatr Med. 2019;10:879–887.
Dziewas R, Warnecke T, Olenberg S, Teismann I, Zimmermann J, Kramer C. Towards a basic endoscopic assessment of swallowing in acute stroke-development and evaluation of a simple dysphagia score. Cerebrovasc Dis.2008;26(1):41–7.
Kaiser MJ, Bauer JM, Ramsch C, et al. Validation of the Mini Nutritional Assessment Short-Form(MNA®-SF): A practical tool for identification of nutritional status. J Nutr Health Aging. 2009;13:782–788.
Malmstrom TK, Morley JE. SARC-F: a simple questionnaire to rapidly diagnose sarcopenia. J Am Med Dir Assoc. 2013;14(8):531–2.
Chen LK, Woo J, Assantachai P, et al. Asian Working Group for Sarcopenia: 2019 Consensus Update on Sarcopenia Diagnosis and Treatment. J Am Med Dir Assoc. 2020;21(3):300–307.
Makizako H, Nakai Y, Tomioka K, Taniguchi Y. Prevalence of sarcopenia defined using the Asia Working Group for Sarcopenia criteria in Japanese community-dwelling older adults: A systematic review and meta-analysis. Phys Ther Res. 2019;22(2):53–57.
Schweitzer L, Geisler C, Pourhassan M, et al. What is the best reference site for a single MRI slice to assess whole-body skeletal muscle and adipose tissue volumes in healthy adults? Am J Clin Nutr. 2015;102(1):58–65.
Hanaoka M, Yasuno M, Ishiguro M, et al. Morphologic change of the psoas muscle as a surrogate marker of sarcopenia and predictor of complications after colorectal cancer surgery. Int J Colorectal Dis. 2017;32: 847–56.
Baracos VE. Psoas as a sentinel muscle for sarcopenia: a flawed premise. J Cachexia Sarcopenia Muscle. 2017;8:527–28.
Morrell GR, Ikizler TA, Chen X, et al. Psoas Muscle Cross-sectional Area as a Measure of Whole-body Lean Muscle Mass in Maintenance Hemodialysis Patients. J Ren Nutr. 2016;26(4):258–64.
Chang MY, Park Y, Ha JW, et al. Paraspinal Lean Muscle Mass Measurement Using Spine MRI as a Predictor of Adjacent Segment Disease After Lumbar Fusion: A Propensity Score-Matched Case-Control Analysis. AJR Am J Roentgenol. 2019;12:1–8.
Yip C, Dinkel C, Mahajan A, Siddique M, Cook GJ, Goh V. Imaging body composition in cancer patients: visceral obesity, sarcopenia and sarcopenic obesity may impact on clinical outcome. Insights Imaging. 2015;6(4):489–97.
Ranson CA, Burnett AF, Kerslake R, Batt ME, O’Sullivan PB. An investigation into the use of MR imaging to determine the functional cross sectional area of lumbar paraspinal muscles. Eur Spine J. 2006;15:764–773.
King LA, Priest KC, Nutt J, et al. Comorbidity and functional mobility in persons with Parkinson disease. Arch Phys Med Rehabil.2014;95(11):2152–7.
Zhang SF, Zhang Y, Li B, Chen N. Physical inactivity induces the atrophy of skeletal muscle of rats through activating AMPK/FoxO3 signal pathway. Eur Rev Med Pharmaco. 2018;22:199–209.
Baijens LW, Speyer R, Passos VL, Pilz W, Roodenburg N, Clave P. Swallowing in Parkinson patients versus healthy controls: reliability of measurements in videofluoroscopy. Gastroenterol Res Pract.2011;1–9.
Mu L, Sobotka S, Chen J, et al. Altered pharyngeal muscles in Parkinson disease. J Neu-ropathol Exp Neurol. 2012;71:520–530.
Kwon M, Lee JH. Oro-Pharyngeal Dysphagia in Parkinson’s Disease and Related Movement Disorders. J Mov Disord. 2019;12(3):152–160.
Simons JA. Swallowing Dysfunctions in Parkinson’s Disease. Int Rev Neurobiol. 2017;134:1207–1238.
Cereda E, Cilia R, Klersy C, et al. Swallowing disturbances in Parkinson’s disease: A multivariate analysis of contributing factors. Parkinsonism Relat D. 2014;20(12):1382–1387.
Simons JA, Eisemann N, Fietzek UM, Katalinic A. High-risk defining clinical parameters for dysphagia in Parkinson’s disease. J Mov Disord. 2015;30(1): S422–S423.
Pflug C, Bihler M, Emich K, et al. Critical Dysphagia is Common in Parkinson Disease and Occurs Even in Early Stages: A Prospective Cohort Study. Dysphagia. 2018;33(1):41–50
Funding
Funding: There is no funding source in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest: There is no conflict interest among the authors.
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Subjects were informed about the study and their written informed consents were obtained at the beginning of the study.
Informed consent: Informed consent was obtained from all individual participant’s caregivers included in the study.
Rights and permissions
About this article
Cite this article
Umay, E., Yigman, Z.A., Ozturk, E.A. et al. Is Dysphagia in Older Patients with Parkinson’s Disease Associated With Sarcopenia?. J Nutr Health Aging 25, 742–747 (2021). https://doi.org/10.1007/s12603-021-1618-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-021-1618-2