Abstract
Objectives
Community-dwelling older adults with sarcopenia are likely to fall. However, few studies have investigated whether sarcopenia is associated with falls during hospitalization in older adults. The purpose of this study was to determine whether the SARC-F when used as a simple screening tool for sarcopenia at the time of admission, predicts in-hospital falls.
Design
A retrospective, observational study.
Setting
A 900-bed university hospital.
Participants
A total of 9,927 patients aged 65 years and older were hospitalized at the hospital between April 2019 and March 2020.
Measurements
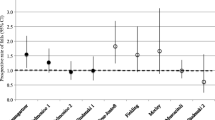
The SARC-F contains five items: strength, assistance in walking, rise from a chair, climb stairs, and falls were evaluated at hospital admission. To investigate the relationship between the SARC-F score and falls, a ROC curve analysis was performed. Multivariate analysis adjusted for fall-related confounding factors such as age, gender, ADL, and disease were performed.
Results
Mean age: 75.9±6.7 years; male: 56.2% were analyzed, and 159 patients (1.6%) fell during hospitalization. SARC-F scores at admission were significantly higher in the fall group than in the control group (3 [1–6] points vs. 0 [¬0–2] point, p<0.001). Statistical association was observed between the SARC-F and in-hospital fall (area under the curve = 0.721 [0.678–0.764], p < 0.001). The cut-off value for the highest sensitivity and specificity of the SARC-F score for in-hospital falls was two (sensitivity = 0.679, specificity = 0.715). Among the subitem of the SARC-F, the hazard ratios for climbing stairs were significantly higher (HR = 1.52 [1.10–2.09], p = 0.011) and for a history of fall was significantly higher (HR = 1.41 [1.02–1.95], p = 0.036). A SARC-F score ≥ 2 had a significantly higher incidence of in-hospital falls compared to a SARC-F score <2 (3.7% vs. 0.7%, p < 0.001). Also, a SARC-F score ≥ 2 had a significantly higher hazard ratio for falls (2.11 [1.37–3.26], p < 0.001).
Conclusion
SARC-F can help predict falls among hospitalized older adults.


Similar content being viewed by others
References
Cruz-Jentoft AJ, Bahat G, Bauer J, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019;48(1):16–31.
Chen LK, Woo J, Assantachai P, et al. Asian Working Group for Sarcopenia: 2019 Consensus Update on Sarcopenia Diagnosis and Treatment. J Am Med Dir Assoc. 2020;21(3):300–7e2.
Malmstrom TK, Morley JE. SARC-F: a simple questionnaire to rapidly diagnose sarcopenia. J Am Med Dir Assoc. 2013;14(8):531–2.
Ishida Y, Maeda K, Nonogaki T, et al. SARC-F as a Screening Tool for Sarcopenia and Possible Sarcopenia Proposed by AWGS 2019 in Hospitalized Older Adults. J Nutr Health Aging. 2020;24(10):1053–60.
Scuffham P, Chaplin S, Legood R. Incidence and costs of unintentional falls in older people in the United Kingdom. J Epidemiol Community Health. 2003;57(9):740–4.
Ambrose AF, Paul G, Hausdorff JM. Risk factors for falls among older adults: a review of the literature. Maturitas. 2013;75(1):51–61.
Moreland JD, Richardson JA, Goldsmith CH, Clase CM. Muscle weakness and falls in older adults: a systematic review and meta-analysis. J Am Geriatr Soc. 2004;52(7):1121–9.
Ishida Y, Maeda K, Nonogaki T, et al. Malnutrition at Admission Predicts In-Hospital Falls in Hospitalized Older Adults. Nutrients. 2020;12(2).
Tanimoto Y, Watanabe M, Sun W, et al. Sarcopenia and falls in community-dwelling elderly subjects in Japan: Defining sarcopenia according to criteria of the European Working Group on Sarcopenia in Older People. Arch Gerontol Geriatr. 2014;59(2):295–9.
Hendrich A, Nyhuis A, Kippenbrock T, Soja ME. Hospital falls: development of a predictive model for clinical practice. Appl Nurs Res. 1995;8(3):129–39.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83.
Oken MM, Creech RH, Tormey DC, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982;5(6):649–55.
Landi F, Liperoti R, Russo A, et al. Sarcopenia as a risk factor for falls in elderly individuals: results from the ilSIRENTE study. Clin Nutr. 2012;31(5):652–8.
Lima DP, de Almeida SB, Bonfadini JC, et al. Clinical correlates of sarcopenia and falls in Parkinson’s disease. PLoS One. 2020;15(3):e0227238.
Brown CJ, Redden DT, Flood KL, Allman RM. The underrecognized epidemic of low mobility during hospitalization of older adults. J Am Geriatr Soc. 2009;57(9):1660–5.
Coker RH, Wolfe RR. Bedrest and sarcopenia. Curr Opin Clin Nutr Metab Care. 2012;15(1):7–11.
Sullivan DH, Sun S, Walls RC. Protein-energy undernutrition among elderly hospitalized patients: a prospective study. JAMA. 1999;281(21):2013–9.
Cruz-Jentoft AJ, Sayer AA. Sarcopenia. Lancet. 2019;393(10191):2636–46.
Chang BC, Khan MI, Prado A, Yang N, Ou J, Agrawal SK. Biomechanical differences during ascent on regular stairs and on a stairmill. J Biomech. 2020;104:109758.
Riwniak C, Simon JE, Wages NP, et al. Comparison of a Multi-Component Physical Function Battery to Usual Walking Speed for Assessing Lower Extremity Function and Mobility Limitation in Older Adults. J Nutr Health Aging. 2020;24(8):906–13.
Morita M, Takamura N, Kusano Y, et al. Relationship between falls and physical performance measures among community-dwelling elderly women in Japan. Aging Clin Exp Res. 2005;17(3):211–6.
Luukinen H, Koski K, Laippala P, Kivela SL. Predictors for recurrent falls among the home-dwelling elderly. Scand J Prim Health Care. 1995;13(4):294–9.
Deandrea S, Lucenteforte E, Bravi F, Foschi R, La Vecchia C, Negri E. Risk factors for falls in community-dwelling older people: a systematic review and meta-analysis. Epidemiology. 2010;21(5):658–68.
Acknowledgments
This work was funded by the Japan Society for the Promotion of Science (grant number: JP20H01144 to Ishida Y and 18K11142 to Maeda K).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical standards: This work was performed according to the ethical standards laid down in the 1964 Declaration of Helsinki and later amendments.
Conflict of Interest: The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Ishida, Y., Maeda, K., Ueshima, J. et al. The SARC-F Score on Admission Predicts Falls during Hospitalization in Older Adults. J Nutr Health Aging 25, 399–404 (2021). https://doi.org/10.1007/s12603-021-1597-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-021-1597-3