Abstract
Background
Because of the lack of sufficient data, we aimed to investigate the role of serum 25(OH) vitamin D level on COVID severity and related mortality.
Methods
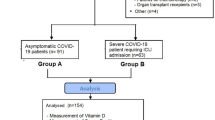
This was a retrospective observational study. Data, including sociodemographic features, clinical characteristics, and laboratory data, and 25(OH) vitamin D levels were recorded for each study participant. Patients were stratified into different vitamin D groups; Normal (Serum 25(OH) vitamin D level >30 ng/mL), Vitamin D insufficiency (21–29 ng/mL), and deficiency (<20 ng/ mL). The severity of COVID was classified according to the Chinese Clinical Guideline for classification of COVID-19 severity. Mortality data were determined for participants. Univariate and multivariate Logistic regression analysis was performed to determine independent predictors of in-hospital mortality.
Results
Overall, 149 COVID-19 patients (females 45.6%, mean age 63.5 ± 15.3 (range 24–90 years) years) were included. Forty-seven patients (31.5%) had moderate COVID-19, whereas 102 patients (68.5%) had severe-critical COVID-19. The mean 25(OH) vitamin D level was 15.2 ± 10.3 ng/mL. Thirty-four (22.8%) and 103 (69.1%) patients had vitamin D insufficiency and deficiency, respectively. Mean serum 25(OH) vitamin D level was significantly lower in patients with severe-critical COVID-19 compared with moderate COVID-19 (10.1 ± 6.2 vs. 26.3 ± 8.4 ng/mL, respectively, p<0.001). Vitamin D insufficiency was present in 93.1% of the patients with severe-critical COVID-19. Multivariate logistic regression analysis revealed that only lymphocyte count, white blood cell count, serum albumin and, 25(OH) vitamin D level were independent predictors of mortality.
Conclusion
Serum 25(OH) vitamin D was independently associated with mortality in COVID-19 patients.
Similar content being viewed by others
Introduction
Coronavirus disease 2019 (COVID-19) has become a pandemic and claimed more than 400.000 lives throughout the world as the time of the writing of this manuscript (1). Advanced age and underlying chronic medical conditions, particularly chronic pulmonary and cardiac diseases, appeared as the most conspicuous predisposing factors for the development of severe COVID-19 and consequent death (2, 3). However, recent observations regarding the relatively greater impact of the disease on the northern latitudes led to the generation of the hypothesis that vitamin D deficiency, to some extent, might have caused a tendency for an increased burden of the disease in vitamin D deficient COVID-19 patients, especially among the elderly (4–6).
Vitamin D is a multi-faceted hormone, the best-known effect of which is on the calcium and phosphorus metabolism. However, multiple lines of experimental and clinical evidence point to its essential regulatory role in both the innate and adaptive immune systems (7). Through several different but additive mechanisms, vitamin D produces anti-viral effects (8). Although not all included studies supported its conclusion, a meta-analysis found a protective effect of vitamin D supplementation against upper respiratory tract viral infections (9). First reports with respect to the role of vitamin D serum levels on contraction of SARS-CoV2 revealed that patients with PCR-proven COVID-19 had significantly lower serum 25(OH) D levels compared with patients without COVID-19, even after controlling for the effect of age (10). However, a larger study did not confirm the results of this latter study (11).
To the best of our knowledge, despite the extensive discussion of the role of vitamin D in COVID-19 susceptibility and development of severe disease through editorials and review articles, only one study evaluated the effect of vitamin D status on mortality in COVID-19 patients. Raharusun and colleagues (12) reported that in 780 patients with laboratory-confirmed COVID-19 in Indonesia, vitamin D status was an independent predictor of mortality. Considering the ongoing high death toll of COVID-19 along with the prevalent nature of vitamin D deficiency, we think that it is of utmost importance to delineate the role of vitamin D status on the prognosis of patients with COVID-19.
Hence, the primary objective of this study was to evaluate the association of vitamin D status with disease severity and mortality in patients with COVID-19.
Methods
Patients, study design and data collection
This was a retrospective observational study that included adult COVID-19 patients in Health Sciences University, Bagcilar Training and Research Hospital, Istanbul, Turkey between April 1st, 2020 and May 20th, 2020. The study protocol was approved by the Hospital Clinical Studies Ethical Committee (2020.06.1.01.072 and 12 June 2020).
The primary outcome measure of the study was all-cause mortality in CO VID-19 patients.
Data, including sociodemographic features, clinical characteristics, and laboratory data comprising complete blood counts, serum albumin, calcium, and 25(OH) vitamin D levels were retrieved from the hospital electronic database system and recorded for each study participant.
Patients who did not have 25(OH) vitamin D values, who had clinical presentation compatible with COVID-19, but did not have a positive PCR-based test for SARS-CoV2, and pediatric patients were excluded from the study.
Measurement of serum 25(OH) vitamin D level and Vitamin D groups
Serum 25(OH) vitamin D levels were studied by electrochemiluminescence method. Patients were stratified into different groups according to their serum 25(OH) vitamin D levels. Serum 25(OH) vitamin D level >30 ng/mL was accepted as normal. Vitamin D insufficiency and deficiency were defined as serum 25(OH) vitamin D levels of 21–29 ng/mL and <20 ng/ mL, respectively (13).
Classification of the severity of COVID-19
We used the Chinese Clinical Guideline for classification of COVID-19 severity, which was devised by the China Health Committee (14). According to this guideline, COVID-19 has four levels of the severity: mild, moderate, severe, and critical. Patient symptoms, laboratory values, and results of imaging studies performed at admission are used to determine severity of COVID-19. Based on this classification system, disease severity groups were defined as follows;
-
Mild disease: Mild clinical symptoms and normal lung on radiologic imaging
-
Moderate disease: Fever and pulmonary symptoms along with pneumonia on radiologic imaging
-
Severe disease: The presence of any of the following criteria: i) respiratory distress (≥ 30 breaths/min); ii) oxygen saturation ≤ 93% at rest; iii) PaO2/FiO2 ≤ 300 mmHg or chest imaging shows obvious lesion progression > 50% within 24–48 hours)
-
Critical disease: The presence of any of the following criteria: i) respiratory failure and need for mechanical ventilation; ii) shock; iii) other organ failures that requires ICU care.
Since patients with mild COVID-19 were not hospitalized according to our National guidelines, our study did not involve any patient with mild disease. Furthermore, for practical purposes for our study aims, we combined severe and critical COVID-19 in a single group named “severe-critical disease”. In the end, we stratified all included patients either to moderate or critical-severe COVID-19 groups.
Statistical analysis
In summarization of the study data, descriptive statistics were presented for continuous variables as either mean +/- standard deviation or median-interquartile range depending on the distribution type of the data. Categorical variables were reported as numbers and percentages. The normality check of numerical variables was performed via the Kolmogorov-Smirnov test. According to groups, to compare categoric variables, chi-square/Fisher exact test used, while Independent Samples t-test or Mann-Whitney U tests was used for continuous variables in case of normal and non-normal distribution, respectively. To evaluate the bivariate correlation between the serum 25(OH) vitamin D level and inflammatory marker, Pearson’s correlation was used. We also constructed univariate and multivariate logistic regression analyses to determine the independent associates of mortality. SPSS 26.0 (IBM Corporation, NY, US) was used to perform all statistical analyses. A P-value <0.05 was considered as statistically significant.
Results
Patient characteristics and baseline laboratory values
Overall, 149 COVID-19 patients (females 45.6%) were included. The mean age of the patients was 63.5 ± 15.3 (range 24–90 years) years. The most frequent comorbid condition was hypertension, which was followed by diabetes mellitus (40.9%) and dyslipidemia (26.2%). Almost one-fifth of the whole group had chronic kidney disease, and the mean estimated glomerular filtration rate (eGFR) was 74.7 ± 33.7 mL/minute.
Sixty-two patients (41.6%) had critical COVID-19, whereas forty patients had severe disease. Baseline laboratory values of the entire study cohort were shown in table-1.
Moderate and severe-critical COVID-19
Forty-seven patients (31.5%) had moderate COVID-19, whereas 102 patients (68.5%) had severe-critical COVID-19. Patients with severe-critical COVID-19 had significantly higher rates of coronary artery disease, hypertension, dyslipidemia, diabetes mellitus, chronic kidney disease, chronic atrial fibrillation, and congestive heart failure compared to patients who had moderate COVID-19. Interestingly, chronic obstructive pulmonary disease frequency was comparable between the groups. Patients with severe-critical COVID-19 had significantly lower eGFR, lower hemoglobin, higher neutrophil and lymphocyte counts, and higher serum C-reactive protein values compared to those of patients with moderate COVID-19. Table-2 summarizes the comorbid disease rates and laboratory values in moderate and severe-critical COVID-19 patients.
25(OH) Vitamin D levels and vitamin D status
The mean 25(OH) vitamin D level was 15.2 ±10.3 ng/mL. The numbers of patients with vitamin D insufficiency and deficiency were 34 (22.8%) and 103 (69.1%), respectively. Only 8.1% of the entire study cohort had a normal level of serum 25(OH) vitamin D (table-1).
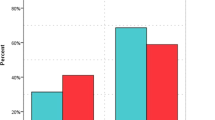
Mean serum 25(OH) vitamin D level was significantly lower in patients with severe-critical COVID-19 compared to that of patients with moderate COVID-19 (10.1 ± 6.2 vs. 26.3 ± 8.4 ng/mL, respectively, p<0.001). Vitamin D insufficiency was present in 93.1% of the patients with severe-critical COVID-19 (table-2, figure-1).
Mean serum 25(OH) vitamin D level was significantly lower among deceased patients compared with the surviving patients (10.4 ± 6.4 vs. 19.3 ± 11.2 ng/mL, respectively, P<0.001). A significantly higher ratio of the deceased patients had vitamin D deficiency compared with surviving patients (92.8% vs. 48.8%, P<0.001) (table-3, figure-2).
Mean serum 25(OH) vitamin D level was negatively correlated with increasing age (r=-0.3, p<0.001).
Correlation of 25(OH) vitamin D and inflammatory markers
Mean serum 25(OH) vitamin D level was significantly and negatively correlated with serum C-reactive protein level (r=−0.253, P=0.002). Mean serum 25(OH) vitamin D level was significantly and negatively correlated with neutrophil count (r=-0.419, P<0.001) and lymphocyte count (r= −0.348, P<0.001).
Mortality and its determinants
In total, 69 out of 149 patients (46.3%) died during the study period. The deceased patients were significantly older compared with surviving patients. As expected, the mortality rate was significantly higher among patients with severe-critical COVID-19 compared with moderate COVID-19 patients (66.7% vs. 2.1%, respectively, P<0.001) (Figure-3).
The deceased COVID-19 patients had significantly higher rates of dyslipidemia, diabetes mellitus, chronic kidney disease, chronic atrial fibrillation, and congestive heart failure compared with surviving patients. The deceased COVID-19 patients had significantly lower eGFR, lower hemoglobin, higher neutrophil and lymphocyte counts, and higher C-reactive protein values compared with their surviving counterparts. The comorbid conditions and laboratory results of the deceased and surviving patients were shown in table-3.
Multivariate logistic regression analysis revealed that only lymphocyte count, white blood cell count, serum albumin, and 25(OH) vitamin D level were independent predictors of mortality. An increase in lymphocyte count, but a decrease in white blood cell count, serum albumin, and 25(OH) vitamin D level was associated with increased mortality in COVID-19 patients (table-4).
Discussion
The salient findings of the present study were as follows: (i) Vitamin D insufficiency (22.8%) and deficiency (69.1%) were quite common among patients with COVID-19. Only 8.1% of the entire study cohort had a normal level of serum 25(OH) vitamin D. (ii) Patients with more severe COVID-19 had lower mean serum 25(OH) vitamin D levels. (iii) A significantly higher ratio of the deceased patients had vitamin D deficiency compared with surviving patients (92.8% vs. 48.8%, P<0.001). (iv) Serum 25(OH) vitamin D level was independently associated with increased mortality in COVID-19 patients in multivariate logistic regression.
Vitamin D has important immune functions. Considering in a context of a viral infection, the beneficial anti-viral effect of vitamin D can be grouped into three categories: enhancing physical barrier against the viruses and beneficial effects on innate and adaptive immunity (15, 16). Vitamin D supports the innate immune system by means of inducing the secretion of several antimicrobial peptides such as defensins. In addition, the active form of vitamin D, calcitriol, has itself several virus suppressive effects. Cytokine storm was found to play an important role in the rapid deterioration of some patients with COVID-19 (17). Importantly, vitamin D can limit the devastating effects of cytokine storm via reducing the release of proinflammatory Th1 derived cytokines such as TNF-alpha and interferon-gamma (18, 19). Last but not least, vitamin D also has an important favorable impact on the adaptive immune system, particularly through the actions of calcitriol. Calcitriol stimulates T regulatory lymphocytes and suppresses cytokine release both from Th1 and Th2 lymphocytes (20, 21).
COVID-19 loaded a proportionately heavy burden on the elderly (22, 23). One of the main reasons for this was the common occurrence of chronic medical conditions in this age group. Moreover, both the presence of comorbidities and advancing age per se are associated with reduced 25(OH) vitamin D levels (24). We should take the effects of the lockdown and avoidance of sun exposure into account on the already insufficient 25(OH) vitamin D levels.
Hypothesis regarding the potential deleterious roles of vitamin D deficiency on COVID-19 patients initially originated from the studies in which 25(OH) vitamin D was shown to be related to increased susceptibility to infection (25, 26). However, some studies did not show the beneficial effects of vitamin D supplementation on the prevention and treatment of viral respiratory infections (27, 28). Then, some authors reported that the mean level of 25(OH) vitamin D level was inversely correlated with COVID-19 infection rates and mortality in 20 European countries (5). The authors emphasized the possible association of severely deficient vitamin D status and very high case fatality rates among the elderly in Spain and Italy. Some others also speculated that COVID-19 related mortality was lower in countries south of Latitude 35 degrees north might be related to vitamin D deficiency that is more prevalent due to limited sun exposure (29).
Despite all the experimental evidence regarding the antiviral and immunity supporting roles of vitamin D, along with indirect clinical evidence showing the potential detrimental effect of vitamin D deficiency on upper respiratory viral infections, to our knowledge, only a few studies evaluated the vitamin D and mortality association in COVID-19 patients. Daneshkhah et al. (30) reported that in COVID-19 patients, serum C-reactive protein levels were inversely correlated with serum 25(OH) D levels. The authors concluded that since CRP is a marker of inflammation, vitamin D deficiency might be related to increased inflammation and cytokine storm in these patients. Alipio first reported the independent association between vitamin D deficiency and increased mortality (31). In another retrospective study, Raharusun and colleagues showed that 25(OH) vitamin D value was an independent predictor of mortality.
Our results present important data regarding the relationship between vitamin D deficiency and prognosis of COVID-19. First of all, the prevalence of vitamin D deficiency/insufficiency was very high among hospitalized moderate-to-severely ill COVID-19 patients. The mean level of 25(OH) vitamin D was 15.2 ± 10.3ng/mL. Moreover, as COVID-19 severity increased, the level of 25(OH) vitamin D further reduced. Multivariable logistic regression analysis revealed that 25(OH) vitamin D level was independently associated with mortality, even after controlling for age and comorbid diseases was performed. Serum 25(OH) vitamin D level was positively correlated with serum C-reactive protein levels and negatively correlated with both neutrophil and lymphocyte counts. Thus, the unfavorable effects of low serum vitamin D levels in terms of disease severity and mortality might be partly due to the increased inflammation. Our results also showed that mean serum 25(OH) vitamin D level was negatively correlated with increasing age (r=−0.3, p<0.001). Thus, we speculate that disproportionately unfavorable clinical outcomes seen in the elderly may be, in part, due to the age-related vitamin D deficiency.
Some limitations of the present study deserve mention. First, since this study was a retrospective analysis, we did not control all the factors that potentially might have impacted the mortality rate. Our sample size is relatively small. However, it should be kept in mind that we only included patients who have moderate-to-severe COVID-19.
Conclusion
In conclusion, our analysis revealed that vitamin D insufficiency/deficiency was quite prevalent among hospitalized COVID-19 patients. The level of 25(OH) vitamin D level was inversely related to the severity of the COVID-19. Moreover, vitamin D level was an independent predictor of COVID-19 related mortality. Since it is still rampant in many areas of the world, and considering the lack of an effective vaccine and specific drugs, measures to strengthen the immune system might be strongly considered. Before recommending the routine application of high-dose vitamin D in vulnerable populations, controlled studies investigating the effects of vitamin D supplementation on the COVID-19 severity and mortality are warranted.
References
Johns Hopkins University Coronavirus Resource Center, https://coronavirus.jhu.edu/map.html, accessed 14th June, 2020.
Guan WJ, Liang WH, Zhao Y, Liang HR, Chen ZS, Li YM, et al. Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis. Eur Respir J. 2020;55(5).
Wang B, Li R, Lu Z, Huang Y. Does comorbidity increase the risk of patients with COVID-19: evidence from meta-analysis. Aging (Albany NY). 2020;12(7):6049–57.
Rhodes JM, Subramanian S, Laird E, Kenny RA. Editorial: low population mortality from COVID-19 in countries south of latitude 35 degrees North supports vitamin D as a factor determining severity. Aliment Pharmacol Ther. 2020;51(12):1434–7.
Ilie PC, Stefanescu S, Smith L. The role of vitamin D in the prevention of Coronavirus disease 2019 infection and mortality. Aging Clin Exp Res. 2020.
Kara M, Ekiz T, Ricci V, Kara O, Chang KV, Ozcakar L. ‘Scientific Strabismus’ or Two Related Pandemics: COVID-19 & Vitamin D Deficiency. Br J Nutr. 2020:1–20.
Aranow C. Vitamin D and the immune system. J Investig Med. 2011;59(6):881–6.
Teymoori-Rad M, Shokri F, Salimi V, Marashi SM. The interplay between vitamin D and viral infections. Rev Med Virol. 2019;29(2):e2032.
Martineau AR, Jolliffe DA, Hooper RL, Greenberg L, Aloia JF, Bergman P, et al. Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data. BMJ. 2017;356:i6583.
D’Avolio A, Avataneo V, Manca A, Cusato J, De Nicolo A, Lucchini R, et al. 25-Hydroxyvitamin D Concentrations Are Lower in Patients with Positive PCR for SARS-CoV-2. Nutrients. 2020;12(5).
Hastie CE, Mackay DF, Ho F, Celis-Morales CA, Katikireddi SV, Niedzwiedz CL, et al. Vitamin D concentrations and COVID-19 infection in UK Biobank. Diabetes Metab Syndr. 2020;14(4):561–5.
Raharusun, Prabowo and Priambada, Sadiah and Budiarti, Cahni and Agung, Erdie and Budi, Cipta, Patterns of COVID-19 Mortality and Vitamin D: An Indonesian Study (April 26, 2020). Available at SSRN: https://ssrn.com/abstract=3585561 or https://doi.org/10.2139/ssrn.3585561.
Holick MF. Vitamin D status: measurement, interpretation, and clinical application. Ann Epidemiol. 2009;19(2):73–8.
Diagnosis and Treatment Protocol for Novel Coronavirus Pneumonia (Trial Version 7). Chin Med J (Engl). 2020;133(9):1087-95.
Grant WB, Lahore H, McDonnell SL, Baggerly CA, French CB, Aliano JL, et al. Evidence that Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths. Nutrients. 2020;12(4).
Rondanelli M, Miccono A, Lamburghini S, Avanzalo I, Riva A, Allegrini P, et al. Self-Care for Common Colds: The Pivotal Role of Vitamin D, Vitamin C, Zinc, and Echinacea in Three Main Immune Interactive Clusters (Physical Barriers, Innate and Adaptive Immunity) Involved during an Episode of Common Colds-Practical Advice on Dosages and on the Time to Take These Nutrients/Botanicals in order to Prevent or Treat Common Colds. Evid Based Complement Alternat Med. 2018;2018:5813095.
Ye Q, Wang B, Mao J. The pathogenesis and treatment of the “Cytokine Storm’ in COVID-19. J Infect. 2020;80(6):607–13.
Sharifi A, Vahedi H, Nedjat S, Rafiei H, Hosseinzadeh-Attar MJ. Effect of single-dose injection of vitamin D on immune cytokines in ulcerative colitis patients: a randomized placebo-controlled trial. APMIS. 2019;127(10):681–7.
Aygun H. Vitamin D can prevent COVID-19 infection-induced multiple organ damage. Naunyn Schmiedebergs Arch Pharmacol. 2020.
Jeffery LE, Burke F, Mura M, Zheng Y, Qureshi OS, Hewison M, et al. 1,25-Dihydroxyvitamin D3 and IL-2 combine to inhibit T cell production of inflammatory cytokines and promote development of regulatory T cells expressing CTLA-4 and FoxP3. J Immunol. 2009;183(9):5458–67.
Cantorna MT, Snyder L, Lin YD, Yang L. Vitamin D and 1,25(OH)2D regulation of T cells. Nutrients. 2015;7(4):3011–21.
Liu K, Chen Y, Lin R, Han K. Clinical features of COVID-19 in elderly patients: A comparison with young and middle-aged patients. J Infect. 2020;80(6):e14–e8.
Zheng Z, Peng F, Xu B, Zhao J, Liu H, Peng J, et al. Risk factors of critical & mortal COVID-19 cases: A systematic literature review and meta-analysis. J Infect. 2020.
Kaur J, Ferguson SL, Freitas E, Miller R, Bemben D, Knehans A, et al. Association of Vitamin D Status with Chronic Disease Risk Factors and Cognitive Dysfunction in 50(-)70 Year Old Adults. Nutrients. 2019;11(1).
Arihiro S, Nakashima A, Matsuoka M, Suto S, Uchiyama K, Kato T, et al. Randomized Trial of Vitamin D Supplementation to Prevent Seasonal Influenza and Upper Respiratory Infection in Patients With Inflammatory Bowel Disease. Inflamm Bowel Dis. 2019;25(6):1088–95.
Cannell JJ, Vieth R, Umhau JC, Holick MF, Grant WB, Madronich S, et al. Epidemic influenza and vitamin D. Epidemiol Infect. 2006;134(6):1129–40.
Aglipay M, Birken CS, Parkin PC, Loeb MB, Thorpe K, Chen Y, et al. Effect of High-Dose vs Standard-Dose Wintertime Vitamin D Supplementation on Viral Upper Respiratory Tract Infections in Young Healthy Children. JAMA. 2017;318(3):245–54.
Hueniken K, Aglipay M, Birken CS, Parkin PC, Loeb MB, Thorpe KE, et al. Effect of High-Dose Vitamin D Supplementation on Upper Respiratory Tract Infection Symptom Severity in Healthy Children. Pediatr Infect Dis J. 2019;38(6):564–8.
Marik PE, Kory P, Varon J. Does vitamin D status impact mortality from SARS-CoV-2 infection? Med Drug Discov. 2020:100041.
Daneshkhah A, Agrawal V, Eshein A, Subramanian H, Roy HK, Backman V. The Possible Role of Vitamin D in Suppressing Cytokine Storm and Associated Mortality in COVID-19 Patients. medRxiv. 2020:2020.04.08.20058578.
Alipio, Mark, Vitamin D Supplementation Could Possibly Improve Clinical Outcomes of Patients Infected with Coronavirus-2019 (COVID-19) (April 9, 2020). Available at SSRN: https://ssrn.com/abstract=3571484 or https://doi.org/10.2139/ssrn.3571484.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest: The authors declare that they have no conflict of interest.
Ethical standards: The study protocol was approved by the Hospital Clinical Studies Ethical Committee (2020.06.1.01.072 and 12 June 2020).
Rights and permissions
About this article
Cite this article
Karahan, S., Katkat, F. Impact of Serum 25(OH) Vitamin D Level on Mortality in Patients with COVID-19 in Turkey. J Nutr Health Aging 25, 189–196 (2021). https://doi.org/10.1007/s12603-020-1479-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-020-1479-0