Abstract
Objective
To determine the physical indicators associated with oral intake status and swallowing function in gastrostomy patients under long-term care.
Design
Cross-sectional study.
Setting
Thirty-one hospitals that perform gastrostomy insertion, replacement and management.
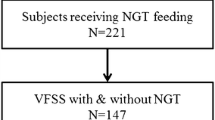
Participants
A total of 117 respondents from 31 hospitals in Japan underwent gastrostomy tube replacement and management between September 2012 and January 2014. Each participant underwent a gastrostomy at least 6 months prior to the study, and received long-term care either at home, a care facility, or a hospital.
Measurements
We conducted a questionnaire survey at Japanese hospitals and used the data obtained from 117 respondents for analysis. The survey was conducted using a questionnaire form that collected information about the following items: oral intake status, sex, age, disease history, number of days elapsed since gastrostomy, residence status, modified Rankin Scale score, consciousness, oral hygiene status, articulation and phonation, voluntary saliva swallow, Modified Water Swallow Test, and Food Test.
Results
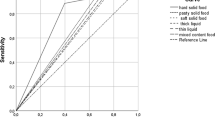
Results revealed significant differences in modified Rankin Scale scores, sputum production, articulation and phonation, and voluntary saliva swallowing between patients who were orally fed and those who were not. Moreover, sputum production and voluntary saliva swallowing were strongly associated with oral intake status. Finally, sputum production, articulation and phonation, and voluntary saliva swallowing were strongly associated with swallowing function test results.
Conclusion
Results from this study suggested that sputum production, articulation and phonation, and voluntary saliva swallowing could be used as indicators for estimating oral intake status and swallowing function in gastrostomy patients under long-term care.
Similar content being viewed by others
References
Gauderer MWL, Ponsky JL, Izant IL. Gastrostomy without laparotomy: A percutaneous endoscopic technique. J Pedi atr Surg. 1980;15: 872–875.
Gauderer MW. Percutaneous endoscopic gastrostomy-20 years later: a historical perspective. J Pediatr Surg. 2001;36: 217–219.
Sako A, Yasunaga H, Horiguchi H, et al. Prevalence and in-hospital mortality of gastrostomy and jejunostomy in Japan: a retrospective study with a national administrative database. Gastrointest Endosc. 2014;80: 88–96.
Sugiyama M, Takada K, Shinde M, et al. National survey of the prevalence of swallowing difficulty and tube feeding use as well as implementation of swallowing evaluation in long-term care settings in Japan. Geriatr Gerontol Int. 2014;14: 577–581.
Gomes CA, Andriolo RB, Bennett C, et al. Percutaneous endoscopic gastrostomy versus nasogastric tube feeding for adults with swallowing disturbances. 2015;22:CD008096.
Yutaka Suzuki, Mitsuyoshi Urashima, et al. The Effects of Percutaneous Endoscopic Gastrostomy on Quality of Life in Patients With Dementia. Gastroenterology Research. 2012;5: 10–20.
Löser C, Aschl G, Hébuterne X, et al. ESPEN guidelines on artificial enteral nutrition—percutaneous endoscopic gastrostomy (PEG). Clin Nutr. 2005;24: 848–861.
Nakanishi M, Hattori K. Percutaneous endoscopic gastrostomy (PEG) tubes are placed in elderly adults in Japan with advanced dementia regardless of expectation of improvement in quality of life. J Nutr Health. 2014;18: 503–509.
Poisson P, Laffond T, Campos S, et al. Relationships between oral health, dysphagia and undernutrition in hospitalised elderly patients. Gerodontology. Epub 2014/03/11.
Galan Sanchez-Heredero MJ, Santander Vaquero C, Cortazar Saez M, et al. Relationship between dysphagia and malnutritition in patients over 65 years of age. Enfermeria clinica. 2014;24: 183–90.
Cvejic L, Harding R, Churchward T, et al. Laryngeal penetration and aspiration in individuals with stable COPD. 2011;16: 269–275.
Kidd D, Lawson J, Nesbitt R, MacMahon J. The natural history and clinical consequences of aspiration in acute stroke. QJM. 1995;88: 409–413.
Mann G, Hankey GJ, Cameron D. Swallowing function after stroke: prognosis and prognostic factors at 6 months. Stroke. 1999;30: 744–748.
Knol W, van Marum RJ, Jansen PA, et al. Antipsychotic drug use and risk of pneumonia in elderly people. J Am Geriatr Soc.2008;56: 661–666.
Rudolph JL, Gardner KF, Gramigna GD, McGlinchey RE. Antipsychotics and oropharyngeal dysphagia in hospitalized older patients. J Clin Psychopharmacol. 2008;28: 532–535.
van Swieten JC, Koudstaal PJ, Visser MC, et al. Interobserver agreement for the assessment of handicap in stroke patients. Stroke. 1988;19: 604–607.
Shinohara Y, Minematsu K, Amano T, Ohashi Y. Modified Rankin Scale with expanded guidance scheme and interview questionnaire: Interrater agreement and reproducibility of assessment. Cerevrovasc Dis. 2006;21: 271–278.
Tohara H, Saitoh E, Mays KA, et al. Three tests for predicting aspiration without videofluorography. Dysphagia. 2003;18: 126–134.
Yokohama S, Aoshima M, Koyama S, et al. Possibility of oral feeding after induction of percutaneous endoscopic gastrostomy. J Gastroenterol Hepatol. 2010;25: 1227–1231.
Ickenstein GW, Kelly PJ, Furie KL, et al. Predictors of feeding gastrostomy tube removal in stroke patients with dysphagia. J Stroke Cerebrovasc Dis. 2003;12: 169–174.
Chong VH, Vu C. Percutaneous endoscopic gastrostomy outcomes: can patient profiles predict mortality and weaning? Singapore Med J. 2006;47: 383–387.
Naik AD, Abraham NS, Roche VM, Concato J. Predicting which patients can resume oral nutrition after percutaneous endoscopic gastrostomy tube placement. Aliment Pharmacol Ther. 2005;21: 1155–1161.
Fumi Mizuhashi, Kaoru Koide, Toya Shuji, et al. Examination of Oral Dryness Patients; Comparison of Four Tests: Flow Rate of Rest Saliva, Saxon Test, Oral Moisture, and RSST. Japanese Society of Gerodontology. 2009;24: 374–380.
Young Sik Won. Influence of Manual Facilitation Technique on Swallowing Disorder and Aspiration Pneumonia Caused by Severe Dysphagia with Stroke. J. Phys. Ther. Sci. 2012;24: 909–913.
Altman KW, Richards A, Goldberg L, et al. Dysphagia in stroke, neurodegenerative disease, and advanced dementia. Otolaryngol Clin North Am. 2013;46: 1137–1149.
Baikie G, Reddihough DS, South M, Cook DJ. The salivagram in severe cerebral palsy and able-bodied adults. J Paediatr Child Health. 2009;45: 342–345.
McCullough GH, Wertz RT, Rosenbek JC. Sensitivity and specificity of clinical/bedside examination signs for detecting aspiration in adults subsequent to stroke. J Commun Disord. 2001;34: 55–57.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nakayama, E., Tohara, H., Sakai, K. et al. Predictive factors associated with oral intake ability in gastrostomy patients under long-term care. J Nutr Health Aging 21, 715–720 (2017). https://doi.org/10.1007/s12603-016-0796-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-016-0796-9