Abstract
Objectives
Although serum uric acid (sUA) is not a criterion for diagnosing metabolic syndrome (MetS), many studies have identified a positive association between sUA and MetS in patients of various ages and ethnicities. This association has not been fully established in the very elderly.
Design
Cross-sectional and longitudinal study.
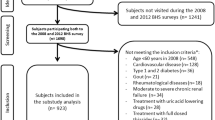
Setting and participants
A total of 18,906 Chinese elderly aged 65 and older undergoing routine health checkups in Taiwan were enrolled.
Measurements
Modified Adult Treatment Panel III criteria were used to define MetS. All participants were further divided into nine groups with gender specification according to age (the young-old, 65 to 74; old-old, 75 to 84; and oldest-old, 85 and over) and sUA concentration tertile (males: sUAG1, <5.7 mg/dL; sUAG2, 5.7–6.7 mg/dL; and sUAG3, > 6.7 mg/dL; females: sUAG1, <4.9 mg/dL; sUAG2, 4.9–5.9 mg/dL; and sUAG3, > 5.9 mg/dL). A cross-sectional study was first performed to determine the correlation between sUA and MetS and its components. A longitudinal study then excluded subjects with MetS at baseline to explore the risk of MetS according to sUA levels in 3 age groups.
Results
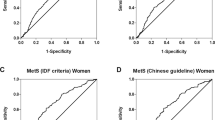
In the cross-sectional study, we observed a graded, positive association between sUA and MetS components that diminished after age 75. Subjects with higher sUA levels had higher odds ratios (OR) for the occurrence of MetS in the young-old and old-old groups of both sexes (P <0.001) except sUAG2 males in the old-old group. However, the association diminished with age and only a higher OR was observed in sUAG2 males in the oldestold group (OR, 3.38; 95% CI, 1.11–10.30; P = 0.032). In the longitudinal study, the Kaplan–Meier plot showed that higher sUA levels were associated with a higher risk of MetS in the young-old group of both genders (P < 0.001 sUAG3 vs. sUAG1 and sUAG2). Cox regression analysis further confirmed these results (young-old group: sUAG3 HR, 1.90; 95% CI, 1.42-2.54; P < 0.001; old-old group males: HR, 2.20; 95% CI, 1.04-4.65; P = 0.039; young-old females: HR, 1.83; 95% CI, 1.38 - 2.43; P < 0.001).
Conclusions
Higher sUA levels in the young-old group of Chinese elderly were associated with a higher risk of developing MetS. sUA levels are thus regarded as a potential tool for early diagnosis of MetS. However, this association diminished in those over 75 years of age.

Similar content being viewed by others
References
Mottillo S, Filion KB, Genest J et al. The metabolic syndrome and cardiovascular risk: a systematic review and meta-analysis. J Am Coll Cardiol 2010;56:1113–1132
Ford ES, Li C, Sattar N. Metabolic syndrome and incident diabetes: Current state of the evidence. Diabetes Care 2008;31:1898–1904
Chen J, Muntner P, Hamm LL et al. The Metabolic Syndrome and Chronic Kidney Disease in U.S. Adults. Ann Intern Med 2004;140:167–174
Stone NJ, Bilek S, Rosenbaum S. Recent National Cholesterol Education Program Adult Treatment Panel III Update: Adjustments and Options. Am J Cardiol 2005;96:53E–59E
So A, Thorens B. Uric acid transport and disease. J Clin Invest 2010;120:1791–1799
Chen JH, Chuang SY, Chen HJ et al. Serum uric acid level as an independent risk factor for all-cause, cardiovascular, and ischemic stroke mortality: A Chinese cohort study. Arthritis Rheum 2009;61:225–232
Ebrahimpour P, Fakhrzadeh H, Heshmat R et al. Serum Uric Acid Levels and Risk of Metabolic Syndrome in Healthy Adults. Endocr Pract 2008;14:298–304
Lohsoonthorn V, Dhanamun B, Williams MA. Prevalence of Hyperuricemia and its Relationship with Metabolic Syndrome in Thai Adults Receiving Annual Health Exams. Arch Med Res 2006;37:883–889
Choi HK, Ford ES. Prevalence of the Metabolic Syndrome in Individuals with Hyperuricemia. Am J Med 2007;120:442–447
Lin SD, Tsai DH, Hsu SR. Association Between Serum Uric Acid Level and Components of the Metabolic Syndrome. J Chin Med Assoc 2006;69:512–516
Ford ES, Li C, Cook S et al. Serum Concentrations of Uric Acid and the Metabolic Syndrome Among US Children and Adolescents. Circulation 2007;15;115:2526–2532
Li C, Hsieh MC, Chang SJ. Metabolic syndrome, diabetes, and hyperuricemia. Curr Opin Rheumatol 2013;25:210–216
Wu HW, Yu KH, Lin SR et al. Positive Association between Hyperuricemia and Metabolic Syndrome: A Large Health Check-up Population in Taiwan. Chung Shan Medical Journal 2012;123:11–20
Richette P, Perez-Ruiz F. Serum uric acid and metabolic risk. Curr Med Res Opin 2013;29 Suppl 3:9–15
Department of Health. Nutrition and Health Survey in Taiwan: The status of metabolic syndrome in 2005–2008. http://nahsit.nhri.org.tw/node/21. Accessed 22 February 2010.
Council for Economic Planning and Development. 2008-2056 Population Projection in Taiwan ROC. Accessed September 2008
Lee MS, Lin SC, Chang HY, Lyu, LC. High prevalence of hyperuricemia in elderly Taiwanese. Asia Pac J Clin Nutr 2005;14:285–292
Wei SH, Lin JD, Hsu CH et al. Higher uric acid is associated with higher rate of metabolic syndrome in Chinese elderly. Eur Geriatr Med 2014;5: 26–30
Liu M, He Y, Jiang B. Association between Serum Uric Acid Level and Metabolic Syndrome and Its Sex Difference in a Chinese Community Elderly Population. Int J Endocrinol 2014:754678
Babio N, Martínez-González MA, Estruch R et al. Associations between serum uric acid concentrations and metabolic syndrome and its components in the PREDIMED study. Nutr Metab Cardiovasc Dis 2015;25:173–180
A Report of a Joint Rural Health Advisory Committee and State Community Health Services Advisory Committee Work Group. Creating Healthy Communities for an Aging Population. http://www.health.state.mn.us/divs/orhpc/pubs/healthyaging/hareportnofs.pdf Accessed May 2006
Alberti KG, Eckel RH, Grundy SM et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009;120:1640–1645
Health Promotion Administration, M.o.H.a.W., R.O.C. http://www.hpa.gov.tw/BHPNet/Web/HealthTopic/TopicArticle.aspx?No=200712250123&parentid=200712250023 Accessed May 2007
Yang T, Chu CH, Bai CH et al. Uric acid level as a risk marker for metabolic syndrome: A Chinese cohort study. Atherosclerosis 2012;220:525–531
Oda E. Serum uric acid is an independent predictor of metabolic syndrome in a Japanese health screening population. Heart Vessels 2014;29:496–503
Gonçalves JP, Oliveira A, Severo M, Santos AC, Lopes C. Cross-sectional and longitudinal associations between serum uric acid and metabolic syndrome. Endocrine 2012;41:450–457
Sui X, Church TS, Meriwether RA, Lobelo F, Blair SN. Uric acid and the development of metabolic syndrome in women and men. Metabolism 2008;57:845–852
Liu PW, Chang TY, Chen JD. Serum uric acid and metabolic syndrome in Taiwanese adults. Metabolism 2010;59:802–807
Chiou WK, Huang DH, Wang MH, Lee YJ, Lin JD. Significance and association of serum uric acid (UA) levels with components of metabolic syndrome (MS) in the elderly. Arch Gerontol Geriatr 2012;55:724–728
Lin JD, Chiou WK, Chang HY Liu FH, Weng HF. Serum uric acid and leptin levels in metabolic syndrome: a quandary over the role of uric acid. Metabolism 2007;56:751–756
Choi HK, Ford ES. Haemoglobin A1c, fasting glucose, serum C-peptide and insulin resistance in relation to serum uric acid levels—the Third National Health and Nutrition Examination Survey. Rheumatology (Oxford) 2008;47:713–717
Dai CY, Chuang WL, Ho CK, Ou TT, Huang JF, Hsieh MY, Yu ML. High Serum Uric Acid As A Novel Risk Factor for Type 2 Diabetes: Response to Dehghan et al. Diabetes Care 2008;31: e67
Nagahama K, Iseki K, Inoue T, Touma T, Ikemiya Y, Takishita S. Hyperuricemia and cardiovascular risk factor clustering in a screened cohort in Okinawa, Japan. Hypertens Res 2004;27:227–233
Kawamoto R, Tabara Y, Kohara K, Kusunoki T, Abe M, Miki T. Serum Uric Acid Is More Strongly Associated with Impaired Fasting Glucose in Women than in Men from a Community-Dwelling Population. PLoS One 2013;13;8:e65886
Chou P, Lin KC, Lin HY et al. Gender differences in the relationships of serum uric acid with fasting serum insulin and plasma glucose in patients without diabetes. J Rheumatol 2001;28:571–576
Lin KC, Tsai ST, Lin HY, Chou P. Different progressions of hyperglycemia and diabetes among hyperuricemic men and women in the kinmen study. J Rheumatol 2004;31:1159–1165
Sun X, Zhang R, Jiang F. Common Variants Related to Serum Uric Acid Concentrations are Associated with Glucose Metabolism and Insulin Secretion in a Chinese Population. PLoS One 2015;24;10:e0116714.
Kolz M, Johnson T, Sanna S et al. Meta-analysis of 28,141 Individuals Identifies Common Variants within Five New Loci That Influence Uric Acid Concentrations. PLoS Genet 5:e1000504
Christensen PJ, Steestrup O. Uric Acid Excretion with Increasing Plasma Glucose Concentration (Pregnant and Nonpregnant Cases). Scand J Clin Lab Invest 1958;10:182–185
Herman JB, Keynan A. Hyperglycemia and uric acid. Isr J Med Sci 1969;5:1048–1052
Hairong Nan, Zengchang Pang, Shaojie Wang et al. Serum uric acid, plasma glucose and diabetes. Diab Vasc Dis Res 2010;7:40–46.
Rowe JW, Kahn RL. Human aging: usual and successful. Science 1987;10;237:143–149
Depp CA, Jeste DV. Definitions and Predictors of Successful Aging: A Comprehensive Review of Larger Quantitative Studies. Am J Geriatr Psychiatry 2006;14:6–20
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chen, JH., Hsieh, CH., Liu, JS. et al. The power of serum uric acid in predicting metabolic syndrome diminishes with age in an elderly Chinese population. J Nutr Health Aging 20, 912–917 (2016). https://doi.org/10.1007/s12603-015-0633-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-015-0633-6