Abstract
Objective
The aim of this study was to estimate MS prevalence according to three criteria and its risk factors among men in rural China.
Design
Cross-sectional study.
Setting
The Nantong Metabolic Syndrome Study (NMSS) was conducted during 2007–2008 in Nantong, China.
Participants
6997 male participants aged 18–74 years.
Measurements
In person interviews, blood glucose and lipid measurements were accomplished.
Results
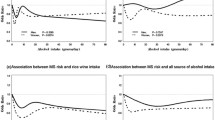
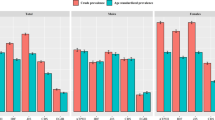
The prevalence of MS was 12.86%, 8.55% and 15.28% according to IDF, ATPIII and ATPIII-modified criteria, respectively. The IDF and ATP III–modified criteria agreed only moderately with ATP III criteria (ϰ= 0.56 and 0.68), whereas ATP III–modified and the IDF criteria agreed perfectly (ϰ= 0.90). Vigorous occupational physical activity was associated with a low prevalence of MS with Odds ratio (OR) of 0.58 (95% confidence interval (CI): 0.45-0.74). Beer drinkers (alcohol ≤ 6.2 g/day) and rice wine drinkers (alcohol ≤ 9.0 g/day) had about 34% and 33% low risks of developing MS respectively, compared with non-drinkers. OR of MS was 1.95 (95% CI: 1.39-2.73) in men who had familial history of at least two diseases, including hypertension and diabetes, compared with men without familial history of those diseases.
Conclusions
Our data suggested that MS is highly prevalent among men in rural China. Family history of diabetes and hypertension is a risk factor in MS development. Physical activity, rice wine and beer consumption are associated with a significantly lower risk.






Similar content being viewed by others
Abbreviations
- MS:
-
Metabolic syndrome
- NMSS:
-
The Nantong Metabolic Syndrome Study
- T2D:
-
Type 2 diabetes
- CVD:
-
Cardiovascular disease
- CHD:
-
Coronary heart disease
- ATPIII:
-
Adult Treatment Panel
- IDF:
-
The International Diabetes Federation
- BMI:
-
Body mass index
- WC:
-
Waist circumference
- CDC:
-
Center for Disease Control and Prevention
- LPA:
-
Physical activity during leisure time
- OPA:
-
Occupational physical activity
- CPA:
-
Commuting physical activity
- OR:
-
Odds ratio
- ANOVA:
-
Analysis of variance
References
Yamaoka K, Tango T. Effects of lifestyle modification on metabolic syndrome: a systematic review and meta-analysis. BMC medicine 2012;10: 138.
Kassi E, Pervanidou P, Kaltsas G, Chrousos G. Metabolic syndrome: definitions and controversies. BMC Med 2011;9: 48.
Tal S, Melzer E, Chsherbakov T, Malnick S. Metabolic syndrome is associated with increased prevalence of advanced colorectal polyps. J Nutr Health Aging 2014;18: 22–25.
Rouch I, Achour-Crawford E, Roche F, Castro-Lionard C, Laurent B, et al. Sevenyear predictors of self-rated health and life satisfaction in the elderly: the PROOF study. J Nutr Health Aging 2014;18: 840–847.
Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med 1998;15: 539–553.
Ford ES, Giles WH, Dietz WH. Prevalence of the metabolic syndrome among US adults: findings from the third National Health and Nutrition Examination Survey. Jama 2002;287: 356–359.
Alberti KGM, Zimmet P, Shaw J. The metabolic syndrome—a new worldwide definition. The Lancet 2005;366: 1059–1062.
Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute scientific statement: Executive Summary. Crit Pathw Cardiol 2005;4: 198–203.
WHO EC. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004;363: 157.
Tan CE, Ma S, Wai D, Chew SK, Tai ES. Can we apply the National Cholesterol Education Program Adult Treatment Panel definition of the metabolic syndrome to Asians? Diabetes Care 2004;27: 1182–1186.
Gu D, Reynolds K, Wu X, Chen J, Duan X, et al. Prevalence of the metabolic syndrome and overweight among adults in China. The Lancet 2005;365: 1398–1405.
Song QB, Zhao Y, Liu YQ, Zhang J, Xin SJ, et al. Sex difference in the prevalence of metabolic syndrome and cardiovascular-related risk factors in urban adults from 33 communities of China: The CHPSNE study. Diab Vasc Dis Res, 2015.
Villegas R, Xiang YB, Yang G, Cai Q, Fazio S, et al. Prevalence and determinants of metabolic syndrome according to three definitions in middle-aged Chinese men. Metab Syndr Relat Disord 2009;7: 37–45.
Cai H, Huang J, Xu G, Yang Z, Liu M, et al. Prevalence and determinants of metabolic syndrome among women in Chinese rural areas. PloS one 2012;7: e36936.
Shu XO, Hatch MC, Mills J, Clemens J, Susser M. Maternal smoking, alcohol drinking, caffeine consumption, and fetal growth: results from a prospective study. Epidemiology 1995;6: 115–120.
Trivedi T, Liu J, Probst JC, Martin AB. The metabolic syndrome: are rural residents at increased risk? J Rural Health 2013;29: 188–197.
Lao XQ, Zhang YH, Wong MC, Xu YJ, Xu HF, et al. The prevalence of metabolic syndrome and cardiovascular risk factors in adults in southern China. BMC Public Health 2012;12: 64.
Zhao Y, Yan H, Yang R, Li Q, Dang S, et al. Prevalence and determinants of metabolic syndrome among adults in a rural area of Northwest China. PLoS One 2014;9: e91578.
Lao XQ, Ma WJ, Sobko T, Zhang YH, Xu YJ, et al. Dramatic escalation in metabolic syndrome and cardiovascular risk in a Chinese population experiencing rapid economic development. BMC Public Health 2014;14: 983.
Wang Z, Zhai F, Du S, Popkin B. Dynamic shifts in Chinese eating behaviors. Asia Pac J Clin Nutr 2008;17: 123–130.
Xu WH, Ruan XN, Fu XJ, Zhu QL, Zhang H, et al. Prevalence of the metabolic syndrome in Pudong New Area of Shanghai using three proposed definitions among Chinese adults. BMC Public Health 2010;10: 246.
Sung KC, Kim BJ, Kim BS, Lee WY, Park JB, et al. A comparison of the prevalence of the MS and its complications using three proposed definitions in Korean subjects. Am J Cardiol 2009;103: 1732–1735.
Katulanda P, Ranasinghe P, Jayawardena R, Sheriff R, Matthews DR (2015) The influence of family history of diabetes on disease prevalence and associated metabolic risk factors among Sri Lankan adults. Diabet Med 2015;32: 314–323.
Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009;120: 1640–1645.
Gao M, Ding D, Huang J, Qu Y, Wang Y, et al. Association of genetic variants in the adiponectin gene with metabolic syndrome: a case-control study and a systematic meta-analysis in the Chinese population. PLoS One 2013;8: e58412.
Gayda M, Brun C, Juneau M, Levesque S, Nigam A. Long-term cardiac rehabilitation and exercise training programs improve metabolic parameters in metabolic syndrome patients with and without coronary heart disease. Nutr Metab Cardiovasc Dis 2008;18: 142–151.
Halldin M, Rosell M, de Faire U, Hellenius ML. The metabolic syndrome: prevalence and association to leisure-time and work-related physical activity in 60-year-old men and women. Nutr Metab Cardiovasc Dis 2007;17: 349–357.
Myong JP, Kim HR, Jung-Choi K, Baker D, Choi B. Disparities of metabolic syndrome prevalence by age, gender and occupation among Korean adult workers. Ind Health 2012;50: 115–122.
Kwon CS, Lee JH (2013) The Association between Type of Work and Insulin Resistance and the Metabolic Syndrome in Middle-Aged Korean Men: Results from the Korean National Health and Nutrition Examination Survey IV (2007~2009). World J Mens Health 2013;31: 232–238.
Santos AC, Ebrahim S, Barros H. Alcohol intake, smoking, sleeping hours, physical activity and the metabolic syndrome. Prev Med 2007;44: 328–334.
Slagter SN, van Vliet-Ostaptchouk JV, Vonk JM, Boezen HM, Dullaart RP, et al. Combined effects of smoking and alcohol on metabolic syndrome: the LifeLines cohort study. PLoS One 2014;9: e96406.
Barrio-Lopez MT, Bes-Rastrollo M, Sayon-Orea C, Garcia-Lopez M, Fernandez-Montero A, et al. Different types of alcoholic beverages and incidence of metabolic syndrome and its components in a Mediterranean cohort. Clin Nutr 2013;32:797–804.
Carlsson S, Hammar N, Grill V. Alcohol consumption and type 2 diabetes Metaanalysis of epidemiological studies indicates a U-shaped relationship. Diabetologia 2005;48: 1051–1054.
Xin X, He J, Frontini MG, Ogden LG, Motsamai OI, et al. Effects of alcohol reduction on blood pressure: a meta-analysis of randomized controlled trials. Hypertension 2001;38: 1112–1117.
Rimm EB, Williams P, Fosher K, Criqui M, Stampfer MJ. Moderate alcohol intake and lower risk of coronary heart disease: meta-analysis of effects on lipids and haemostatic factors. BMJ 1999;319: 1523–1528.
Jequier E (1999) Alcohol intake and body weight: a paradox. Am J Clin Nutr 1999;69: 173–174.
Chen CC, Lin WY, Li CI, Liu CS, Li TC, et al. The association of alcohol consumption with metabolic syndrome and its individual components: the Taichung community health study. Nutr Res 2012;32: 24–29.
Athyros VG, Liberopoulos EN, Mikhailidis DP, Papageorgiou AA, Ganotakis ES, et al. Association of drinking pattern and alcohol beverage type with the prevalence of metabolic syndrome, diabetes, coronary heart disease, stroke, and peripheral arterial disease in a Mediterranean cohort. Angiology 2007;58: 689–697.
Liu L, Wang Y, Lam KS, Xu A. Moderate wine consumption in the prevention of metabolic syndrome and its related medical complications. Endocr Metab Immune Disord Drug Targets 2008;8: 89–98.
Churilla JR, Johnson TM, Curls R, Richardson MR, Boyer WR, et al. Association between alcohol consumption patterns and metabolic syndrome. Diabetes Metab Syndr 2014;8: 119–123.
Jin L, Huang Y, Bi Y, Zhao L, Xu M, et al. Association between alcohol consumption and metabolic syndrome in 19,215 middle-aged and elderly Chinese. Diabetes Res Clin Pract 2011;92: 386–392.
Hucker B, Wakeling L, Vriesekoop F. The quantitative analysis of thiamin and riboflavin and their respective vitamers in fermented alcoholic beverages. J Agric Food Chem 2011;59: 12278–12285.
Bian S, Gao Y, Zhang M, Wang X, Liu W, et al. Dietary nutrient intake and metabolic syndrome risk in Chinese adults: a case-control study. Nutr J 2013;12: 106.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Yi Shen and Hui Cai contributed equally to this work.
Rights and permissions
About this article
Cite this article
Liu, Y., Huang, J., Xu, G. et al. Prevalence and determinants of metabolic syndrome-identified by three criteria among men in rural China: A population-based cross-sectional study conducted during 2007–2008. J Nutr Health Aging 20, 574–582 (2016). https://doi.org/10.1007/s12603-015-0615-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-015-0615-8