Abstract
Objectives: Objectives
Sarcopenia, the involuntary loss of skeletal muscle with age, affects up to onequarter of older adults. Evidence indicates a positive association between dietary protein intake and lean muscle mass and strength among older persons, but information on dietary protein's effect on physical performance in older adults has received less attention.
Design
Cross-sectional observational analysis of the relationship of dietary protein on body composition and physical performance.
Setting
Clinical research center.
Participants
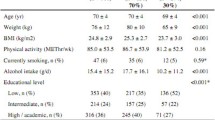
387 healthy women aged 60–90 years (mean 72.7 ± 7.0 y).
Measurements
Measures included body composition (fat-free mass, appendicular skeletal mass and fat mass) via dual x-ray absorptiometry (DXA), physical performance (Physical Performance Test [PPT] and Short Physical Performance Battery [SPPB]), handgrip strength, Physical Activity Scale in the Elderly (PASE), quality of life measure (SF-8), falls, fractures, nutrient and macromolecule intake (four-day food record). Independent samples t-tests determined mean differences between the above or below RDA protein groups.
Statistical Analysis
Analysis of covariance was used to control for body mass index (BMI) between groups when assessing physical performance, physical activity and health-related quality of life.
Results
The subjects consumed an average of 72.2 g protein/day representing 1.1 g protein/kg body weight/day. Subjects were categorized as below the recommended daily allowance (RDA) for protein (defined as less than 0.8 g protein/kg) or at or above the RDA (equal to or higher than 0.8 g protein/kg). Ninety-seven subjects (25%) were in the low protein group, and 290 (75%) were in the higher protein group. Women in the higher protein group had lower body mass, including fat and lean mass, and fat-to-lean ratio than those in the lower-protein group (p <0.001). Composite scores of upper and lower extremity strength were impaired in the group with low protein intake; SPPB score was 9.9±1.9 compared to 10.6±1.6 in those with higher protein intake and PPT was 19.8± 2.9 compared to 20.9±2.1 in the low and higher protein groups, respectively. The results were attenuated by correction for BMI, but remained significant. The physical component of the SF-8 was also lower in the low protein group but did not remain significant when controlling for BMI. No significant differences were found in hand grip strength or reported physical activity.
Conclusion
Healthy, older postmenopausal women consumed, on average, 1.1 g/kg/d protein, although 25% consumed less than the RDA. Those in the low protein group had higher body fat and fat-to-lean ratio than those who consumed the higher protein diet. Upper and lower extremity function was impaired in those who consumed a low protein diet compared to those with a higher protein intake. Protein intake should be considered when evaluating the multi-factorial loss of physical function in older women.
Similar content being viewed by others
References
Iannuzzi-Sucich M, Prestwood KM, Kenny AM. Prevalence of sarcopenia and predictors of skeletal muscle mass in healthy, older men and women. J Gerontol A Biol Sci Med Sci 2002;57:M772–M777.
Evans WJ. Protein nutrition, exercise and aging. J Am Coll Nutr 2004;23:601S–609S.
Evans WJ, Campbell WW. Sarcopenia and age-related changes in body composition and functional capacity. J Nutr 1993;123:465–468.
Genaro Pde S, Martini LA. Effect of protein intake on bone and muscle mass in the elderly. Nutr Rev 2010;68:616–623.
Borsheim E, Bui QU, Tissier S, Kobayashi H, Ferrando AA, Wolfe RR. Effect of amino acid supplementation on muscle mass, strength and physical function in elderly. Clin Nutr 2008;27:189–195.
Houston DK, Nicklas BJ, Ding J, et al. Dietary protein intake is associated with lean mass change in older, community-dwelling adults: the Health, Aging, and Body Composition (Health ABC) Study. Am J Clin Nutr 2008;87:150–155.
Lord C, Chaput JP, Aubertin-Leheudre M, Labonte M, Dionne IJ. Dietary animal protein intake: association with muscle mass index in older women. J Nutr Health Aging 2007;11:383–387.
Beasley JM, LaCroix AZ, Neuhouser ML, et al. Protein intake and incident frailty in the Women's Health Initiative observational study. J Am Geriatr Soc 2010;58:1063–1071.
Baier S, Johannsen D, Abumrad N, Rathmacher JA, Nissen S, Flakoll P. Year-long changes in protein metabolism in elderly men and women supplemented with a nutrition cocktail of beta-hydroxy-beta-methylbutyrate (HMB), L-arginine, and Llysine. JPEN J Parenter Enteral Nutr 2009;33:71–82.
Pannemans DL, Wagenmakers AJ, Westerterp KR, Schaafsma G, Halliday D. Effect of protein source and quantity on protein metabolism in elderly women. Am J Clin Nutr 1998;68:1228–1235.
Symons TB, Schutzler SE, Cocke TL, Chinkes DL, Wolfe RR, Paddon-Jones D. Aging does not impair the anabolic response to a protein-rich meal. Am J Clin Nutr 2007;86:451–456.
Fujita S, Dreyer HC, Drummond MJ, et al. Nutrient signalling in the regulation of human muscle protein synthesis. J Physiol 2007;582:813–823.
Munger RG, Cerhan JR, Chiu BC. Prospective study of dietary protein intake and risk of hip fracture in postmenopausal women. Am J Clin Nutr 1999;69:147–152.
Tkatch L, Rapin CH, Rizzoli R, et al. Benefits of oral protein supplementation in elderly patients with fracture of the proximal femur. J Am Coll Nutr 1992;11:519–525.
Campbell WW, Crim MC, Dallal GE, Young VR, Evans WJ. Increased protein requirements in elderly people: new data and retrospective reassessments. Am J Clin Nutr 1994;60:501–509.
Campbell WW, Trappe TA, Wolfe RR, Evans WJ. The recommended dietary allowance for protein may not be adequate for older people to maintain skeletal muscle. J Gerontol A Biol Sci Med Sci 2001;56:M373–M380.
Gersovitz M, Motil K, Munro HN, Scrimshaw NS, Young VR. Human protein requirements: assessment of the adequacy of the current Recommended Dietary Allowance for dietary protein in elderly men and women. Am J Clin Nutr 1982;35:6–14.
Bunker VW, Lawson MS, Stansfield MF, Clayton BE. Nitrogen balance studies in apparently healthy elderly people and those who are housebound. Br J Nutr 1987;57:211–221.
Morais JA, Chevalier S, Gougeon R. Protein turnover and requirements in the healthy and frail elderly. J Nutr Health Aging 2006;10:272–283.
Chevalier S, Gougeon R, Nayar K, Morais JA. Frailty amplifies the effects of aging on protein metabolism: role of protein intake. Am J Clin Nutr 2003;78:422–429.
Morais JA, Ross R, Gougeon R, Pencharz PB, Jones PJ, Marliss EB. Distribution of protein turnover changes with age in humans as assessed by whole-body magnetic resonance image analysis to quantify tissue volumes. J Nutr 2000;130:784–791.
Fulgoni VL, 3rd. Current protein intake in America: analysis of the National Health and Nutrition Examination Survey, 2003–2004. Am J Clin Nutr 2008;87:1554S–1557S.
Kenny AM, Boxer RS, Kleppinger A, Brindisi J, Feinn R, Burleson JA. Dehydroepiandrosterone combined with exercise improves muscle strength and physical function in frail older women. J Am Geriatr Soc 2010;58:1707–1714.
Kenny AM, Kleppinger A, Annis K, et al. Effects of transdermal testosterone on bone and muscle in older men with low bioavailable testosterone levels, low bone mass, and physical frailty. J Am Geriatr Soc 2010;58:1134–1143.
Hutchins-Wiese HL, Kleppinger A, Annis K, et al. The impact of supplemental n-3 long chain polyunsaturated fatty acids and dietary antioxidants on physical performance in postmenopausal women. J Nutr Health Aging 2013;17:76–80.
Washburn RA, McAuley E, Katula J, Mihalko SL, Boileau RA. The physical activity scale for the elderly (PASE): evidence for validity. J Clin Epidemiol 1999;52:643–651.
Kwon S, Perera S, Pahor M, et al. What is a meaningful change in physical performance? Findings from a clinical trial in older adults (the LIFE-P study). J Nutr Health Aging 2009;13:538–544.
Bartali B, Frongillo EA, Bandinelli S, et al. Low nutrient intake is an essential component of frailty in older persons. J Gerontol A Biol Sci Med Sci 2006;61:589–593.
Martin H, Aihie Sayer A, Jameson K, et al. Does diet influence physical performance in community-dwelling older people? Findings from the Hertfordshire Cohort Study. Age Ageing 2011;40:181–186.
Rolland Y, Lauwers-Cances V, Cristini C, et al. Difficulties with physical function associated with obesity, sarcopenia, and sarcopenic-obesity in community-dwelling elderly women: the EPIDOS (EPIDemiologie de l'OSteoporose) Study. Am J Clin Nutr 2009;89:1895–1900.
Li Z, Heber D. Sarcopenic obesity in the elderly and strategies for weight management. Nutr Rev 2012;70:57–64.
Morley JE, Thomas DR. Anorexia and aging: pathophysiology. Nutrition 1999;15:499–503.
Stipanuk MH. Biochemical, Physiological, Molecular Aspects of Human Nutrition. Second ed. St. Louis: Saunders Elsevier; 2006.
Mendez MA, Popkin BM, Buckland G, et al. Alternative methods of accounting for underreporting and overreporting when measuring dietary intake-obesity relations. Am J Epidemiol 2011;173:448–458.
Walrand S, Boirie Y. Optimizing protein intake in aging. Curr Opin Clin Nutr Metab Care 2005;8:89–94.
Arnal MA, Mosoni L, Boirie Y, et al. Protein pulse feeding improves protein retention in elderly women. Am J Clin Nutr 1999;69:1202–1208.
Kerstetter JE, O’Brien KO, Caseria DM, Wall DE, Insogna KL. The impact of dietary protein on calcium absorption and kinetic measures of bone turnover in women. J Clin Endocrinol Metab 2005;90:26–31.
Gaffney-Stomberg E, Insogna KL, Rodriguez NR, Kerstetter JE. Increasing dietary protein requirements in elderly people for optimal muscle and bone health. J Am Geriatr Soc 2009;57:1073–1079.
Stookey JD, Adair LS, Popkin BM. Do protein and energy intakes explain long-term changes in body composition? J Nutr Health Aging 2005;9:5–17.
Mitchell D, Haan MN, Steinberg FM, Visser M. Body composition in the elderly: the influence of nutritional factors and physical activity. J Nutr Health Aging 2003;7:130–139.
Piatti PM, Monti F, Fermo I, et al. Hypocaloric high-protein diet improves glucose oxidation and spares lean body mass: comparison to hypocaloric high-carbohydrate diet. Metabolism 1994;43:1481–1487.
Layman DK, Boileau RA, Erickson DJ, et al. A reduced ratio of dietary carbohydrate to protein improves body composition and blood lipid profiles during weight loss in adult women. J Nutr 2003;133:411–417.
Tieland M, van de Rest O, Dirks ML, et al. Protein Supplementation Improves Physical Performance in Frail Elderly People: A Randomized, Double-Blind, Placebo-Controlled Trial. J Am Med Dir Assoc 2012.
Barzilay JI, Blaum C, Moore T, et al. Insulin resistance and inflammation as precursors of frailty: the Cardiovascular Health Study. Arch Intern Med 2007;167:635–641.
Fedele MJ, Hernandez JM, Lang CH, et al. Severe diabetes prohibits elevations in muscle protein synthesis after acute resistance exercise in rats. J Appl Physiol 2000;88:102–108.
Barzilay JI, Cotsonis GA, Walston J, et al. Insulin resistance is associated with decreased quadriceps muscle strength in nondiabetic adults aged >or=70 years. Diabetes Care 2009;32:736–738.
Gilber A BN, Tremblay A, Astrup A. Effect of proteins from different sources on body composition. Nutr Metab Cardiovasc Dis 2011:1–16.
Fried LP, Xue QL, Cappola AR, et al. Nonlinear multisystem physiological dysregulation associated with frailty in older women: implications for etiology and treatment. J Gerontol A Biol Sci Med Sci 2009;64:1049–1057.
Goris AH, Westerterp-Plantenga MS, Westerterp KR. Undereating and underrecording of habitual food intake in obese men: selective underreporting of fat intake. Am J Clin Nutr 2000;71:130–134.
Trabulsi J, Schoeller DA. Evaluation of dietary assessment instruments against doubly labeled water, a biomarker of habitual energy intake. Am J Physiol Endocrinol Metab 2001;281:E891–E899.
Sawaya AL, Tucker K, Tsay R, et al. Evaluation of four methods for determining energy intake in young and older women: comparison with doubly labeled water measurements of total energy expenditure. Am J Clin Nutr 1996;63:491–499.
Black AE, Prentice AM, Goldberg GR, et al. Measurements of total energy expenditure provide insights into the validity of dietary measurements of energy intake. J Am Diet Assoc 1993;93:572–579.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gregorio, L., Brindisi, J., Kleppinger, A. et al. Adequate dietary protein is associated with better physical performance among post-menopausal women 60–90 years. J Nutr Health Aging 18, 155–160 (2014). https://doi.org/10.1007/s12603-013-0391-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-013-0391-2