Abstract
Neurogenic pulmonary edema (NPE) is found in many epilepsy patients at autopsy. It is a life-threatening complication, known for almost 100 years, but its etiopathogenesis is still not completely understood. In this study, we used the tremor rat (TRM: tm/tm) as an animal model of epilepsy to investigate the potential mechanisms of NPE under epileptic conditions. We performed reverse-phase high-pressure liquid chromatography assay, H&E and Masson staining, TUNEL assay, and Western blot experiments to determine the role of seizures in NPE. We found the level of catecholamine was higher in TRM rats. Also the occurrence of alveolar cell apoptosis was increased. Moreover, pulmonary vascular remodeling including the deposition of collagen and medial thickening was also found in TRM rats. Further study showed that cell apoptosis was mediated by increasing Bax, decreasing Bcl-2, and activating caspase-3. In addition, the protein level of phosphorylated ERK (p-ERK) was found to be decreased while phosphorylated JNK and phosphorylated p38 were upregulated in TRM rats. Thus, these findings suggest that pulmonary vascular remodeling and alveolar cell apoptosis might be involved in epilepsy-induced NPE and that the mitogen-activated protein kinase signal pathway was involved.
Similar content being viewed by others
Introduction
Epilepsy comprises a variety of neurological disorders characterized by recurrent seizures, and it affects 1–2 % of the population worldwide [1]. There are 50 million people with epilepsy worldwide; 40 million live in developing countries [2]. The mortality of patients with epilepsy is two to three times that of the general population [3, 4]. Although most epilepsies are considered multifactorial diseases, some specific types are considered single-gene disorders [1]. Nervous system infections are the most important reason for seizures. Sudden unexpected death in epilepsy (SUDEP) is defined as a sudden, unexpected, nontraumatic, witnessed or unwitnessed death and is a major clinical problem in epilepsy patients, especially those with chronic, uncontrolled epilepsy [5]. There are several pathophysiological events contributing to SUDEP, including central apnea, autonomic dysregulation of cerebral and cardiac blood flow, decreased heart rate variability (HRV), and neurogenic pulmonary edema (NPE). The pulmonary conditions central apnea and NPE are among the most frequently implicated mechanisms in SUDEP cases [6].
NPE is a life-threatening complication following central nervous system injury. It has been well known for almost 100 years, but its etiopathogenesis is still not completely understood. The roles of central nervous system trigger zones, systemic sympathetic discharge, inflammation and anesthesia, and intracranial pressure in the etiopathogenesis of NPE have been considered in detail [7]. NPE develops rapidly following injury and significantly complicates the overall clinical status of the patient. It is characterized by marked pulmonary vascular congestion with perivascular edema, extravasation, and intra-alveolar accumulation of protein- rich edema fluid and intraalveolar hemorrhage [8–10]. Although several pathophysiological mechanisms have been proposed, the exact cascade leading to the development of NPE is unclear [9, 10]. Both a rapid, transient, and severe sympathetic discharge and the release of vasoactive substances are thought to be involved in this process [11]. NPE is found in many cases of epilepsy at autopsy [12]. A proven mechanism of seizure-induced NPE is the intense generalized vasoconstriction from the massive seizure-related outpouring of central sympathetic activity, which leads to an increase in pulmonary vascular resistance [13, 14]. The aim of this study is to explore the exact mechanism of epilepsy-induced NPE.
The tremor rat (TRM) (tm/tm), a single-gene mutant, is the parent strain of the spontaneously epileptic rat (SER: zi/zi, tm/tm) found in the Kyoto:Wistar colony that exhibits both absence-like and convulsive seizures without any external stimuli [15]. Previous works have demonstrated that the absence-like seizures in TRM rats are characterized by paroxysmal occurrence of 5–7-Hz spike-wave-like complexes in hippocampal electroencephalograms (EEGs) at 8 weeks, similar to 3 Hz in human epilepsy [16–18]. Thus, this TRM rat is most likely to be a suitable animal model for epilepsy. In the current study, the TRM rat was selected as an animal model of epilepsy to determine the NPE of seizures, and significant lung injury was observed in the TRM rat. Therefore, the present experiments were designed to investigate the potential mechanisms of NPE in TRM rats. We suspected that pulmonary vascular remodeling and alveolar cell apoptosis might be involved in epilepsy-induced NPE.
Materials and methods
Materials
Antibodies against Bax, Bcl-2, caspase-3, and β-actin were purchased from Santa Cruz Biotechnology, Inc. (CA, USA). Rabbit polyclonal antibodies to ERK, phospho-ERK, JNK, phosphor-JNK, p38, phosphor-p38, collagen I, and collagen III were from Cell Signaling Technology, Inc. (Beverly, MA, USA). The terminal deoxynucleotidyl transferase-mediated dUTP nick end labeling (TUNEL) kit was from Roche (Mannheim, Germany). Enhanced chemiluminescence (ECL) reagent was from Amersham International (Amersham, UK). All other reagents were from common commercial sources.
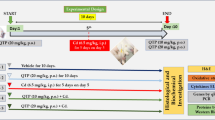
Animal and lung tissue preparation
The animal protocols were approved by the Institutional Animal Care and Use Committee (IACUC). Adult female/male Wistar rats and TRM rats at the age of 6 months were used in this study. Rats with a mean weight of 200 g were conditioned at a controlled ambient temperature of 22 ± 2 °C with 50 ± 10 % relative humidity and at a 12-h light–dark cycle (lights on at 8:00 a.m.). Standard rat chow and water were provided ad libitum to all rats. We anesthetized each rat with pentobarbital injection (120 mg/kg, i.p.), opened the thorax, and removed the heart and lungs to the flat plate. In some experiments, the lungs were quickly removed and further processed for immunostaining as described below.
Morphometric analysis
Rats were anesthetized, and tissue blocks were sliced and perfused with 4 % paraformaldehyde for overnight fixation. Fixed tissues were then dehydrated, cleared, and embedded in paraffin wax. The tissues were cut into 5-μm-thick sections and stained with H&E and Masson staining.
TUNEL assay
Alveolar cell apoptosis was measured by TUNEL assay according to the manufacturer’s protocol. Under the light microscope, the normal nucleolus of alveolar cells was stained blue and the apoptotic nucleolus brown. Apoptotic cells in each group were carefully evaluated under double-blind conditions.
Western blot analysis
Rat lung tissues containing only alveolus were homogenized in lysis buffer (Tris 50 mM, pH 7.4, NaCl 150 mM, Triton X-100 1 %, EDTA 1 mM, and PMSF 2 mM) containing protease inhibitors on ice. The homogenate was sonicated for 1 min and then centrifuged at 14,000 rpm for 15 min at 4 °C. The protein concentrations in the supernatant were confirmed using the Bio-Rad protein assay kit (Bio-Rad Laboratories, Inc., Berkeley, CA, USA). The protocol for Western blot analysis was similar to previous descriptions [19, 20].
Reverse-phase high-pressure liquid chromatography (RP-HPLC) assay
The contents of catecholamine levels in rat blood samples were analyzed by RP-HPLC according to the published method [21]. Each sample was centrifuged at 4,000 rpm for 15 min at 4 °C. HClO4 (200 μl, 0.1 M, Sigma), DHBA (50 μl, 2 μg/ml), and supernatants (250 μl) were added to a test tube. The mixture was shaken for 5 min and centrifuged at 14,000×g for 10 min at 4 °C. The supernatants were filtered with a 0.5-μm filter and then used for catecholamine detection. The levels of adrenaline (AD) and noradrenaline (NA) in rat plasma were measured by HPLC. DHBA (3,4-dihydroxybenzylamine) was used as an internal standard in each sample. The mobile phase contained SDS (sodium dodecyl sulfate, Sigma) 0.144 g, TEA (triethylamine, Merck) 0.5 ml, CA (citric acid, Merck) 10.5 g, SA (sodium acetate, Sigma) 4.1 g, ME (methanol, Merck) 120 ml, EDTA–2Na (ethylenediaminetetraacetic acid disodium salt, Sigma) 0.186 g, and tri-distilled water 880 ml. The flow rate was 0.8 ml/min. The fluorescence detector (RF-10Axl, Shimadzu) was excited at 280 nm while collecting emitted wavelengths at 330 nm.
Statistical analysis
Experimental data are presented as mean ± SEM. Statistical analysis was performed with one-way ANOVA (analysis of variance), followed by Dunnett’s test where appropriate. Differences were considered to be significant at P < 0.05.
Results
Measurement of catecholamine levels in rat plasma by HPLC
Epilepsy has been found to be associated with higher levels of catecholamines, which could cause lung injury and pulmonary vasoconstriction. Pulmonary edema caused by the intravenous administration of epinephrine was similar to NPE [22, 23]. To determine whether the contents of catecholamine in plasma were increased in TRM rats, the levels of AD and NA were measured by HPLC. Our results showed that the products of AD and NA in plasma were both higher in TRM rats than in normal rats (Fig. 1a, b).
Morphometric analysis of pulmonary vascular remodeling in TRM rats
Previous studies have suggested that seizure-induced NPE leads to an increase in pulmonary vascular resistance [13, 14]. Remodeling of the pulmonary vessel wall is a major cause for the elevated pulmonary vascular resistance. The pulmonary vascular remodeling includes the medial thickening and deposition of collagen. Therefore, the morphology of pulmonary vessels was examined with hematoxylin-eosin and Masson staining. We found that pulmonary vascular walls in TRM rats were thicker than the vessels from normal rats observed with H&E (Fig. 2a). In addition, Masson staining showed that the deposition of collagen was significantly increased in TRM rats (Fig. 2b). The expression of collagen I and collagen III protein in rat alveolar homogenates from normoxic and TRM rats had similar results (Fig. 2c).
H&E and Masson staining in pulmonary vessels from control and TRM rats. a H&E staining showed that the wall thickness in TRM rats was higher compared to normal rats. b The deposition of collagen in pulmonary artery vessels was increased in TRM rats. c Collagen I and collagen III protein expression in rat alveolar homogenates from normoxic and TRM rats. All values are denoted as mean ± SEM from at least three separate experiments. **p < 0.05 vs. control
Alveolar cell apoptosis in TRM rats was analyzed by TUNEL staining and the effects of NPE in epilepsy on apoptotic protein expression
NPE was thought to be a potential mechanism of epilepsy-induced lung injury. To elucidate the cause of NPE in TRM rats, alveolar cell apoptosis was analyzed using TUNEL staining. As shown in Fig. 3a, the apoptotic numbers of alveolar cells in TRM rats increased significantly compared to the control group. To further examine the lung injury induced by spontaneous epilepsy in TRM rats, we analyzed the expression of apoptotic proteins in alveolar homogenates. We found that the expression of Bcl-2 was downregulated and the expression of caspase-3 and Bax was increased in alveolar homogenates in TRM rats (Fig. 3b–d).
Alveolar cell apoptosis in TRM rats was analyzed by TUNEL staining and detection of Bax, Bcl-2, and caspase-3 protein expression in rat alveolar homogenate by Western blot. a Nuclei with brown staining were increased in TRM rats, which were defined as apoptotic cells. b–d Western blot assay was examined for Bax, Bcl-2, and caspase-3 expression. Average data are represented by mean ± SEM (n = 6). **p < 0.05 vs. control
Seizure-induced NPE influenced MAPK cascades in TRM rats
To examine whether epilepsy-induced lung injury led to alveolar cell apoptosis through the mitogen-activated protein kinase (MAPK) signal pathway, extracellular signal-regulated protein kinase (ERK), c-Jun NH2-terminal protein kinase (JNK), and p38 protein expression were analyzed by Western blot. JNK and p38 have been reported to regulate apoptotic or death signals, whereas ERK1/2 mediates the cell growth and differentiation signal in the cell. We found that the total ERK1/2, JNK, and p38 were equivalent in the two groups, while p-ERK1/2 expression was decreased (Fig. 4a). In addition, the expression levels of phosphorylated JNK (p-JNK) and phosphorylated p38 (p-p38) were upregulated in TRM rats (Fig. 4b, c).
Discussion
Epilepsy is one of the most common neurologic diseases worldwide, affecting 3 % of the world’s population. NPE is a complication following several central nervous system injuries, including severe head injury, subarachnoid hemorrhage, and epileptic seizures. NPE is found in many epilepsy patients at autopsy [12]. However, the exact pathogenic mechanism leading to its development is still unclear. In the present study, we used the spontaneously epileptic rat-TRM rat as an animal model of epilepsy to determine the NPE of seizures. This study reported for the first time that epilepsy-induced lung injury led to alveolar cell apoptosis through the mitogen-activated protein kinase (MAPK) signal pathway in TRM rats. In addition, the levels of AD and NA in plasma were both higher in TRM rats than in normal rats. This can cause pulmonary vascular vasoconstriction, leading to pulmonary vascular resistance. Another major discovery is that pulmonary vascular walls in TRM rats were thicker than the vessels from normal rats, and Masson staining showed that the deposition of collagen was significantly increased in TRM rats.
NPE in patients with epilepsy has been reported in previous studies [12, 24–27]. It creates an increase in pulmonary interstitial and alveolar fluid. In adults, it has been reported with prolonged seizure activity. NPE patients developed acute respiratory distress syndrome rapidly after the onset of status epilepticus. The etiopathogenesis of NPE is still not completely understood. Up to now, there are hemodynamic assays, the pulmonary capillary permeability doctrine and blast injury theory. The first two are more recognized. In order to obtain a concept of lung damage, hemodynamic measurements were examined, including left ventricular systolic pressure (LVSP) and left ventricular end-diastolic pressure (LVEDP), and the maximum rates of the left ventricular pressure rise and fall (+dp/dt max and −dp/dt max) were measured at the same time by a pressure transducer interfaced with a BL-420E organism function experiment system [28]. A number of studies have found that epilepsy produces activation of the sympathetic nervous system in both patient and animal models [29]. Therefore, we measured the catecholamine product. Our results showed that the levels of AD and NA were significantly increased in TRM rat plasma. The level of catecholamines could cause lung injury and pulmonary vasoconstriction [22, 23]. Vasoconstriction, remodeling of the pulmonary vessel wall, and deposition of collagen are major causes of elevated pulmonary vascular resistance and pulmonary arterial pressure (PAP) [30, 31]. Consistent with this notion, we found that pulmonary vascular walls in TRM rats were thicker than vessels from normal rats. Meanwhile, Masson staining showed that the deposition of collagen was significantly increased in TRM rats.
Apoptosis, also called programmed cell death, has attracted much attention in some studies [32, 33]; it plays a fundamental role in the genesis of various diseases. The mitochondrial membrane potential is greatly influenced by proteins that belong to the Bcl-2 family [34]. The proapoptotic protein BAX and the antiapoptotic protein Bcl-2 are often studied together as indicators of apoptosis. In the present study, we found that the amount of apoptosis in alveolar cells increased significantly in TRM rats and was consistent with the downregulation of Bcl-2, the upregulation of Bax, and the activation of caspase-3.
MAPKs are phosphorylated in response to a series of extracellular stimuli. At least three subfamilies of the MAPK superfamily have been identified: ERK, JNK, and p38-MAPK [35]. An original study has proved that ERKs are important for cell survival, whereas JNKs and p38-MAPKs were deemed stress responsive and thus involved in apoptosis. JNK and p38-MAPK are potently activated by various forms of inflammatory signals or stress [36]. Activation of p38 MAPK has been shown to be involved in acute lung injury [37]. The differential contribution of different MAPK family members to cell death has been examined after withdrawal of nerve growth factor (NGF) from rat PC-12 pheochromocytoma cells. NGF withdrawal led to sustained activation of the JNK and p38 enzymes and inhibition of ERKs [38]. However, the ERK signal cascade is also known to be central to the activation of cellular processes even in the lung microenvironment, including lung inflammatory fibrosis, cytokine-induced ALI and ARDS, etc. [39–41]. In this study, we found that levels of P-JNK and P-p38 were increased in TRM rats, while P-ERK1/2 decreased. The results demonstrated that the epilepsy induced alveolar cell apoptosis may partly through the activation of MAPKs pathway in TRM rats. Distinct MAPK pathways control and determine cell fate in response to a variety of stimuli. MAPK signaling may either protect or enhance sensitivity to apoptosis depending on the cell type, stimuli, and latency of the MAPK activation. Therefore, the conflicting role of the p-ERK signal may be dependent on the various animal models, cell type, or a variety of stimuli.
The whole body develops tremor in TRM rat at 2 weeks of age, and the tremor gradually disappears at 6–8 weeks of age [18]. The 5–7 spike-and-wave complex associated with behavioral absence-like seizures starts at about 14 weeks of age in tm/tm rats and at about 26 weeks of age in tm/+ rats [16, 42]. TRM shows vacuole formation in the CNS and aplastic gonads in both sexes [18]. By positional cloning, a genomic deletion was found within the critical region of more than 200 kb in which the aspartoacylase gene (Aspa) is located [43]. Abnormal accumulation of N-acetyl-l-aspartate (NAA) is observed especially in the pons and thalamus, and leads to epilepsy. Since aspartoacylase is not expressed in the lung, the cause of lung damage may be seizures.
In conclusion, our results imply that pulmonary vascular remodeling and alveolar cell apoptosis were involved in neurogenic pulmonary edema in TRM rats. The mechanisms were likely to include, at least in part, the activation of a mitochondria-initiated pathway as well as the mitogen-activated protein kinase pathway. These findings might provide us with good therapeutic targets for prompt intervention to treat this disorder in genetic epilepsy. Prompt respiratory support and treatment of the acute neurological insult can prevent further cerebral hypoxic injury.
References
McNamara JO (1999) Emerging insights into the genesis of epilepsy. Nature 399:A15–A22
Singhi P (2011) Infectious causes of seizures and epilepsy in the developing world. Dev Med Child Neurol 53:600–609
Cockerell OC, Johnson AL, Sander JW, Hart YM, Goodridge DM, Shorvon SD (1994) Mortality from epilepsy: results from a prospective population-based study. Lancet 344:918–921
Nashef L, Fish DR, Sander JW, Shorvon SD (1995) Incidence of sudden unexpected death in an adult outpatient cohort with epilepsy at a tertiary referral centre. J Neurol Neurosurg Psychiatry 58:462–464
Nashef L (1997) Sudden unexpected death in epilepsy: terminology and definitions. Epilepsia 38:S6–S8
Schuele SU, Widdess-Walsh P, Bermeo A, Luders HO (2007) Sudden unexplained death in epilepsy: the role of the heart. Cleve Clin J Med 74(Suppl 1):S121–S127
Sedy J, Zicha J, Kunes J, Jendelova P, Sykova E (2008) Mechanisms of neurogenic pulmonary edema development. Physiol Res 57:499–506
Kandatsu N, Nan YS, Feng GG, Nishiwaki K, Hirokawa M, Ishikawa K et al (2005) Opposing effects of isoflurane and sevoflurane on neurogenic pulmonary edema development in an animal model. Anesthesiology 102:1182–1189
Leal Filho MB, Morandin RC, de Almeida AR, Cambiucci EC, Metze K, Borges G et al (2005) Hemodynamic parameters and neurogenic pulmonary edema following spinal cord injury: an experimental model. Arq Neuropsiquiatr 63:990–996
Leal Filho MB, Morandin RC, de Almeida AR, Cambiucci EC, Borges G, Gontijo JA et al (2005) Importance of anesthesia for the genesis of neurogenic pulmonary edema in spinal cord injury. Neurosci Lett 373:165–170
Urdaneta F, Layon AJ (2003) Respiratory complications in patients with traumatic cervical spine injuries: case report and review of the literature. J Clin Anesth 15:398–405
Terrence CF, Rao GR, Perper JA (1981) Neurogenic pulmonary edema in unexpected, unexplained death of epileptic patients. Ann Neurol 9:458–464
Swallow RA, Hillier CE, Smith PE (2002) Sudden unexplained death in epilepsy (SUDEP) following previous seizure-related pulmonary oedema: case report and review of possible preventative treatment. Seizure 11:446–448
Johnston SC, Darragh TM, Simon RP (1996) Postictal pulmonary edema requires pulmonary vascular pressure increases. Epilepsia 37:428–432
Yan HD, Ishihara K, Serikawa T, Sasa M (2003) Activation by N-acetyl-l-aspartate of acutely dissociated hippocampal neurons in rats via metabotropic glutamate receptors. Epilepsia 44:1153–1159
Serikawa T, Ohno Y, Sasa M, Yamada J, Takaori S (1987) A new model of petit mal epilepsy: spontaneous spike and wave discharges in tremor rats. Lab Anim 21:68–71
Hanaya R, Sasa M, Ujihara H, Fujita Y, Amano T, Matsubayashi H et al (1995) Effect of antiepileptic drugs on absence-like seizures in the tremor rat. Epilepsia 36:938–942
Yamada J, Serikawa T, Ishiko J, Inui T, Takada H, Kawai Y et al (1985) Rats with congenital tremor and curled whiskers and hair. Jikken Dobutsu 34:183–188
Mao X, Ma P, Cao D, Sun C, Ji Z, Min D et al (2011) Altered expression of GABAA receptors (alpha4, gamma2 subunit), potassium chloride cotransporter 2 and astrogliosis in tremor rat hippocampus. Brain Res Bull 86:373–379
Cao Y, Mao X, Sun C, Zheng P, Gao J, Wang X et al (2011) Baicalin attenuates global cerebral ischemia/reperfusion injury in gerbils via anti-oxidative and anti-apoptotic pathways. Brain Res Bull 85:396–402
Maier KG, Henderson L, Narayanan J, Alonso-Galicia M, Falck JR, Roman RJ (2000) Fluorescent HPLC assay for 20-HETE and other P-450 metabolites of arachidonic acid. Am J Physiol Heart Circ Physiol 279:H863–H871
Dai S, Xue Q, Sun R, Wang S, Li C, Wu Y et al (1993) Hemodynamic and nonhemodynamic mechanisms of experimental pulmonary edema in rats and the effect of anisodamine and tetramethylpyrazine. Part 1: survival rate, pulmonary index, pathological change and pulmonary vascular permeability. Chin Med Sci J 8:72–76
Dai S, Su S, Cao Y, Sun R, Fan Y, Zhang H et al (1993) Hemodynamic and nonhemodynamic mechanism of experimental pulmonary edema in rats and the effect of anisodamine and tetramethylpyrazine–electron microscopic observation and measurement of pulmonary arterial, pulmonary arterial wedge and systemic arterial pressure (Part 2). Chin Med Sci J 8:129–133
Nguyen TT, Hussain E, Grimason M, Goldstein J, Wainwright MS (2012) Neurogenic pulmonary edema and acute respiratory distress syndrome in a healthy child with febrile status epilepticus. J Child Neurol
Wasowska-Krolikowska K, Krogulska A, Modzelewska-Holynska M (2000) Neurogenic pulmonary oedema in a 13-year-old boy in the course of symptomatic epilepsy–case report. Med Sci Monit 6:1003–1007
Mulroy JJ, Mickell JJ, Tong TK, Pellock JM (1985) Postictal pulmonary edema in children. Neurology 35:403–405
Reuter-Rice K, Duthie S, Hamrick J (2011) Neurogenic pulmonary edema associated with pediatric status epilepticus. Pediatr Emerg Care 27:957–958
Chen F, Cao Y, Qi H, Li L, Huang W, Wang Y, Sun H (2013) Involvement of cardiomyocyte apoptosis in myocardial injury of hereditary epileptic rats. Can J Physiol Pharmacol 91(10):804-811
Shimizu M, Kagawa A, Takano T, Masai H, Miwa Y (2008) Neurogenic stunned myocardium associated with status epileptics and postictal catecholamine surge. Intern Med 47:269–273
Chan SY, Loscalzo J (2008) Pathogenic mechanisms of pulmonary arterial hypertension. J Mol Cell Cardiol 44:14–30
Humbert M, Sitbon O, Simonneau G (2004) Treatment of pulmonary arterial hypertension. N Engl J Med 351:1425–1436
Peter ME, Heufelder AE, Hengartner MO (1997) Advances in apoptosis research. Proc Natl Acad Sci USA 94:12736–12737
Stephanou A, Scarabelli TM, Townsend PA, Bell R, Yellon D, Knight RA et al (2002) The carboxyl-terminal activation domain of the STAT-1 transcription factor enhances ischemia/reperfusion-induced apoptosis in cardiac myocytes. FASEB J 16:1841–1843
Lalier L, Cartron PF, Juin P, Nedelkina S, Manon S, Bechinger B et al (2007) Bax activation and mitochondrial insertion during apoptosis. Apoptosis 12:887–896
Wada T, Penninger JM (2004) Mitogen-activated protein kinases in apoptosis regulation. Oncogene 23:2838–2849
Irigoyen JP, Besser D, Nagamine Y (1997) Cytoskeleton reorganization induces the urokinase-type plasminogen activator gene via the Ras/extracellular signal-regulated kinase (ERK) signaling pathway. J Biol Chem 272:1904–1909
Lin WC, Lin CF, Chen CL, Chen CW, Lin YS (2011) Inhibition of neutrophil apoptosis via sphingolipid signaling in acute lung injury. J Pharmacol Exp Ther 339:45–53
Xia Z, Dickens M, Raingeaud J, Davis RJ, Greenberg ME (1995) Opposing effects of ERK and JNK-p38 MAP kinases on apoptosis. Science 270:1326–1331
Galuppo M, Esposito E, Mazzon E, Di Paola R, Paterniti I, Impellizzeri D et al (2011) MEK inhibition suppresses the development of lung fibrosis in the bleomycin model. Naunyn Schmiedebergs Arch Pharmacol 384:21–37
Fudala R, Krupa A, Matthay MA, Allen TC, Kurdowska AK (2007) Anti-IL-8 autoantibody: IL-8 immune complexes suppress spontaneous apoptosis of neutrophils. Am J Physiol Lung Cell Mol Physiol 293:L364–L374
Krupa A, Kato H, Matthay MA, Kurdowska AK (2004) Proinflammatory activity of anti-IL-8 autoantibody: IL-8 complexes in alveolar edema fluid from patients with acute lung injury. Am J Physiol Lung Cell Mol Physiol 286:L1105–L1113
Kondo A, Nagara H, Akazawa K, Tateishi J, Serikawa T, Yamada J (1991) CNS pathology in the neurological mutant rats zitter, tremor and zitter-tremor double mutant (spontaneously epileptic rat, SER). Exaggeration of clinical and neuropathological phenotypes in SER. Brain 114(Pt 2):979–999
Kitada K, Akimitsu T, Shigematsu Y, Kondo A, Maihara T, Yokoi N et al (2000) Accumulation of N-acetyl-l-aspartate in the brain of the tremor rat, a mutant exhibiting absence-like seizure and spongiform degeneration in the central nervous system. J Neurochem 74:2512–2519
Acknowledgments
This work was supported by the Natural Science Foundation of Heilongjiang Province (No. D201264).
Conflict of interest
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding authors
Additional information
H. Zhao and G. Lin contributed equally to this study.
About this article
Cite this article
Zhao, H., Lin, G., Shi, M. et al. The mechanism of neurogenic pulmonary edema in epilepsy. J Physiol Sci 64, 65–72 (2014). https://doi.org/10.1007/s12576-013-0291-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12576-013-0291-6