Abstract
Mean arterial pressure fluctuates depending on physical or psychological activity, but should be stable at rest at around 100 mmHg throughout an entire life in human. The causes of hypertension and the blood pressure regulation mechanisms have been discussed for a long time, and many aspects have recently become more clear. Circulatory shock or short-term hypotension can be treated based on what is now known, but chronic hypertension is still difficult to treat thoroughly. The exact mechanisms for long-term blood pressure regulation have yet not been elucidated. Neuro–humoral interaction has been suggested as one of the mechanisms. Then, from the 1990s, paracrine hormones like nitric oxide or endothelins have been extensively researched in order to develop endothelial local control mechanisms for blood pressure, which have some relationships to long-term control. Although these new ideas and mechanisms are newly developed, no clear explanation for long-term control has yet been discussed, except for renal abnormality. Recently, a central set-point theory has begun to be discussed. This review will discuss the mechanisms for long-term blood pressure control, based on putative biological missions of circulatory function for life support.
Similar content being viewed by others
Introduction
The damage caused by high blood pressure is coming to be understood even by the general population. It is also widely understood that reducing salt intake is a means to prevent lifestyle-related disease. In cases where a person does develop hypertension, a range of various kinds of therapeutic agents and antihypertensive drugs is available. Studies on blood pressure regulation appear in some ways to have reached a natural conclusion. However, while the treatment of hypertension may appear simple, it is actually surprisingly difficult, and often results in a multi-drug regimen. It is frequently found that any type of drug used to treat hypertension deteriorates in its effectiveness. On the other hand, having a lifestyle-related disease may force patients into a constant battle with their natural appetite or salt preference, which can be a constant frustration to them. Doctors also face difficulties in diagnosing and treating hypertension and giving lifestyle advice. For example, it cannot be determined from just a single measurement whether or not a person has hypertension. Even more fundamentally, while symptomatic treatment of hypertension can be accomplished, curative treatment cannot. The mechanisms of short-term blood pressure regulation have become quite clear, but much remains unknown about the mechanisms of long-term regulation.
This review focuses on the mechanisms of long-term blood pressure regulation. Based on the mechanisms of blood pressure regulation that have been understood to date, consideration is given first to what the goals of regulating blood pressure should be, and then to the meaning and methods of blood pressure regulation based on physiological significance, in view of biological implications including maintenance of life. The goal of this review is that readers also sense the dilemma involved in the regulation system of long-term blood pressure control.
Basics for the blood pressure control system
There are many papers, textbooks, and reviews [1–3] on the fundamentals of blood pressure regulation mechanisms. However, here we would like to briefly go back over those matters that are relatively certain and unlikely to change in the future, those which are necessary for the following discussion, and look at factors related to blood pressure regulation that have been discussed to date.
Blood pressure regulation, regardless of whether it is long-term or short-term, is determined by three factors: contractile force of the heart (H), blood volume (VOL), and total peripheral resistance (TPR). There are aspects of cardiac contractile force and blood volume that are difficult to separate via venous return, but today they are simply treated as independent factors. A full discussion of this would become an unnecessary digression, and so we will not go into details about this issue. These three factors are controlled by the central nervous system through the media of nerves and hormones to manage blood pressure. The central nervous system receives blood pressure information from baroreceptors, and controls blood pressure to keep fluctuations small. Meanwhile, the kidneys contribute greatly to blood pressure regulation from the aspect of regulating body fluid volume through their diuretic function. At the same time, hormones secreted from the kidneys and afferent nerves originating in the kidneys are also involved in blood pressure control. The short-term blood pressure regulation mechanism is currently explained by the above, and theoretically this is adequate for the treatment of acute hypotension, such as circulatory shock. However, this information by itself does not enable curative treatment of the long-term blood pressure regulation mechanism, such as in hypertension.
Humoral regulation versus neural regulation
Circulating hormones have a relatively long-acting blood pressure regulation action. However, essential hypertension cannot be explained by the hormonal abnormalities known to date. Since the discovery of atrial natriuretic peptide (ANP) in 1980 [4], new circulatory hormones have been added to what are called the classical circulating hormones, including catecholamines, the renin–angiotensin system, and vasopressin. ANP is also viewed as a new hormone, included among substances such as adrenomedullin [5] and the endogenous digitalis-like factor (EDLF) [6]. Even so, essential hypertension cannot be explained by these newly discovered hormones. Moreover, the resting blood pressure “value” that is supported by these circulating hormones is not that large. Table 1 shows the resting level range of blood pressure with gene knockout of each hormone or its receptor, as determined by several investigators [7–20]. The data vary, some being for systolic blood pressure and others for mean blood pressure, but resting blood pressure with systolic pressure of 35 mmHg/min at most is maintained. As for mean blood pressure, this seems to be around 10–15 mmHg. There are also data suggesting that vasopressin actually acts to lower blood pressure. There may be criticism that this is not a hormone, but EDLF is also thought to be unrelated to the maintenance of resting blood pressure. Circulating hormones do not contribute very much to the formation of the “value” of resting blood pressure.
On the other hand, when hexamethonium was administered to unanesthetized unrestrained rats and sympathetic nerves were completely blocked, arterial pressure decreases largely. The rats moved about and the data were somewhat noisy, but renal sympathetic nerve activity was seen to completely disappear. Mean resting blood pressure at this time was half the normal level (Fig. 1). Vascular constriction from sympathetic nerve activity makes a large contribution to resting blood pressure, supporting about 50% of it. However, as many people know, before long, habituation to nerve signals occurs or receptors are down-regulated, and the effect is not long-lasting. On this point, hormonal action is known to have a relatively long-lasting action.
Neuro–humoral interaction
Therefore, while their acting strength is weak, if long-acting hormones are believed to influence the activity of sympathetic nerves, which have a strong action (Fig. 2), it seems that long-term blood pressure regulation may be possible. This would be convincing if it could be demonstrated that hormones control the sympathetic centers.
When blood vasopressin levels in rabbits was gradually increased, sympathetic activity became suppressed (Fig. 3) [21]. This suppression did not result from arterial baroreceptor reflex, because nerve activity decreases even with the same blood pressure value. The vasopressin-induced sympathetic suppression action is reportedly due to action on baroreceptors [22–25]. It is also reported that since vasopressin acts directly on the heart, the heart rate response is inhibited [26–28]. There is also a report suggesting that vasopressin acts directly on nerve ganglia [29]. These findings are based on the respective experimental results, but even if the receptors and target organs are maintained intact, the vasopressin–sympathetic nerve blocking action disappears completely when the area postrema is abolished [30]. If vasopressin V1 receptors in the area postrema are blocked, the vasopressin-induced sympathetic suppression disappears [31]. In other words, despite acting on baroreceptors and target organs, the level of this action is small, and then the major cause of the sympathoinhibition is a central action of AVP on the area postrema. In addition, this suppression depends on the input volume from baroreceptors (Fig. 4), discussed in a previous report [32]. From the above, it is thought that the mechanism is as shown in Fig. 5 [33]. These results show the neuro–humoral interaction present.
Effects of intravenous infusion of arginine vasopressin (AVP) on the baroreflex curve and the reflex gain curve of renal sympathetic nerve activity (RSNA) in a rabbit, modified from Ref. [21]. MAP mean arterial pressure
Responses of the baroreflex curve of RSNA to the AVP infusions in intact rabbits, 1CSN + 1AoN rabbits, and 1CSN rabbits, modified from Ref. [32]. 1CSN + 1AoN rabbits the rabbits with one carotid sinus nerve intact and one aortic nerve intact but the others severed, 1CSN rabbits the rabbits with just one carotid sinus nerve intact but the other carotid sinus nerve and two aortic nerves severed, RSNA renal sympathetic nerve activity, AVP arginine vasopressin, MAP mean arterial pressure
A hypothetical mechanism of vasopressin effects on the central nervous system to suppress renal sympathetic nerve activity. AVP arginine vasopressin, AP area postrema, NTS nucleus tractus solitarius, RVLM rostral ventrolateral medulla, CVLM caudal ventrolateral medulla, ImL intermediate lateral column, RSNA renal sympathetic nerve activity
An investigation was conducted on whether or not angiotensin II also has this neuro–humoral interaction. Figure 6 shows that the heart rate–blood pressure arterial baroreceptor reflex curve shifts to the right as the dose of angiotensin II is increased. Angiotensin is administered to a vertebral artery, and so the direct action on peripheral vessels or peripheral organs such as the heart is thought to be small, and central nerve action to be strong. In addition, since the simultaneously recorded sympathetic nerve activity is inhibited (Fig. 7) [34], the effect of the shift cannot be explained by sympathetic nerve action and is conjectured to be due to vagal activity inhibition (Fig. 8) [21]. It has also been found that angiotensin II shows a neuro–humoral interaction via circumventricular organs [35]. It is generally thought that angiotensin enhances sympathetic activity [36]. However, the central endogenous angiotensin action and the angiotensin action originating from the blood flow do not necessarily agree.
Typical responses of the baroreflex curve of heart rate to intra-arterial angiotensin II in a rabbit, and average data of the parameters of the sigmoid curves (n = 7), modified from Ref. [34]. va vertebral arterial infusion, A II: angiotensin II, with infusion rate of 5, 10, 20 ng kg−1 min−1 for less than 5 min. HR heart rate, MAP mean arterial pressure
Responses of RSNA and HR baroreflex curves to intra-vertebral angiotensin II in a rabbit, modified from Ref. [34]. RSNA renal sympathetic nerve activity, HR heart rate, va vertebral arterial infusion, A II angiotensin II infused at a rate of 20 ng kg−1 min−1
A hypothetical mechanism of angiotensin II effects on the central nervous system to enhance heart rate and to suppress renal sympathetic nerve activity. AP area postrema, AN ambiguus nucleus, DMN dorsal motor nucleus of the vagus nerve, NTS nucleus tractus solitarius, RVLM rostral ventrolateral medulla, CVLM caudal ventrolateral medulla, ImL intermediate lateral column, HR heart rate, RSNA renal sympathetic nerve activity
Recognition of neuro-humoral interaction has given rise to the possibility of long-term blood pressure regulation from these interactions (Fig. 9). The area postrema, which is the “site” of these interactions, was therefore abolished, and the effect on resting blood pressure of a state in which such an interaction is unlikely to occur was investigated. Although angiotensin II would also have been good in this test, it has many strong effects on various targets in the cardiovascular system. Vasopressin, which has relatively few effects, was therefore selected, and very small doses were administered intravenously for five consecutive days. The results showed that the effect of eliminating interactions in the area postrema was expressed in body fluid balance and heart rate, but not in blood pressure [37] (Fig. 10). In other words, long-term blood pressure regulation action due to neuro–humoral interaction has not been demonstrated. Although it cannot be concluded from this research alone that there is no long-term blood pressure regulation action due to neuro-humoral interactions, the result was disappointing. However, future studies will need to be conducted before any conclusion is reached.
Effects of the 5-day infusion of vasopressin on arterial pressure and heart rate in intact and area postrema-lesioned rabbits, modified from Ref. [37]. INT intact rabbits, APX rabbits with the area postrema lesioned, MAP mean arterial pressure, HR heart rate, AVP arginine vasopressin. *p < 0.05 compared with control, † p < 0.05 between INT and APX
Central set point
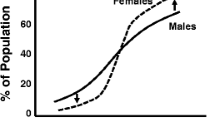
It has long been known that high blood pressure occurs temporarily when baroreceptors are denervated, but after several weeks blood pressure returns to the original resting pressure [38]. Normal systolic blood pressure is thought to be about 130 mmHg or less throughout life [39], although in the case of aged people, opinions are divided. This appears to be just like a “set point” for blood pressure that extends over the long term. In addition, it has been reported that long-term hypertension results when a high-salt diet load is applied after baroreceptors are denervated [40]. Even with baroreceptors intact, it is reported that when the renal nerve is denervated long-term hypotension occurs regardless of the amount of salt intake [41]. These findings suggest that there is probably a central blood pressure set point even in long-term blood pressure regulation [3, 42]. However, is there really a central set point?
Biological significances or missions of circulation
The essential purpose of circulation is to rapidly transport oxygen and other substances to a level that would be impossible with simple diffusion, and to mix the entire body fluid concentration of an individual so that it is as uniform as possible. This links the organs and tissues, which are the parent bodies of various types of specially differentiated functions so that a single, indivisible being is formed. To fulfill this purpose, circulation needs to transport substances and link and integrate all parts of the body in a wide range of states. If this is not done adequately the organism cannot be sustained. Blood pressure is the driving force of circulation, and circulation needs to be able to deal as necessary with various circumstances that occur in the body to fulfill its mission. For example, if oxygen consumption increases as a result of exercise, it is necessary to raise the driving force and increase blood flow. If respiratory function declines, it is necessary to quickly raise the driving force and increase the rate of circulation. Or, when eating, blood flow is concentrated in the gastrointestinal tract. Or when body temperature increases, it is probably necessary to change the driving force so that blood flow is routed to the skin (Fig. 11). While it is certain that the arterial baroreceptor reflex acts to minimize blood pressure fluctuations, it has been found that during exercise even this reflex is suppressed [43]. Thus, even though the arterial baroreceptor reflex system is set mechanically, the reflex can be suppressed by the center when it becomes an interference. These may indicate that the cardiovascular system can achieve its essential function by changing the driving force and acting as needed so that the function of each organ and tissue can be fulfilled in each condition. The meaning here is central drive regulation. If there was a set point in the central nervous system, the blood pressure control system could become a completely closed, self-contained type system so that blood pressure always returns to the set level whatever may happen. Then, the functions of the organs and tissues would not be protected even if the circulatory system itself is. The individual would not even be able to sustain life, so that such a system would be putting the cart before the horse. In this sense, the cardiovascular system should be an open system, and the characteristic of being able to change as circumstances demand is probably essential (Fig. 11).
Phasic control by the neural and hormonal axes
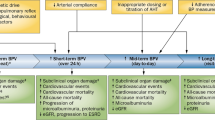
Reconsidering the blood pressure regulation mechanism from this perspective, the nervous and hormonal regulation mechanisms are most likely media that act as regulatory and phasic control systems that transiently regulate blood pressure in time units of seconds and minutes to deal with whatever circumstances arise (Fig. 12a). The results described below might suggest this putative concept.
Rabbit baroreceptors were denervated, and 24-h blood pressure and cardiac output were measured in one study with the time periods divided into when the rabbits were sitting still and when the rabbits were standing and moving in some way. The total peripheral vascular resistance was calculated by blood pressure and cardiac output. Histograms for them were compared with those of rabbits having normal baroreceptors (Figs. 13 and 14). With body movement, blood pressure shifted toward hypertension in the intact baroreceptor animals. There was no shift in blood pressure in the baroreceptor-denervated animals [44]. While no progress has been made in elucidating the detailed mechanism, in animals with normal intact nervous systems, an exercise pressor response occurs when it is necessary for the body. In other words, the neural blood pressure regulation mechanism seems to be a phasic control to the circulatory status demanded for life. It is also generally well known that in times of acute circulatory shock it is not only the sympathetic nerves but also “classic” circulatory hormones, such as sympathetic catecholamine, renin, angiotensin, and aldosterone, that act strongly.
Histograms of 24-h MAP in an intact rabbit and in a SAD rabbit, modified from Ref. [44]. MAP mean arterial pressure, SAD sinoaortic denervated, All all MAP data (8,474 points for intact, 8,398 points for SAD) during 24 h, Rest MAP data (4,059 points for intact, 4,258 points for SAD) during rabbits sitting without movement, Move MAP data (2,507 points for intact, 2,140 points for SAD) during rabbits standing or moving, Other the other data (1,908 points for intact, 2,000 points for SAD) which are recorded during neutral phases
Histograms of 24-h heart rate (HR), aortic blood flow (AoBF) and total peripheral resistance (TPR) in an intact rabbit and a SAD rabbit, modified from Ref. [44]. AoBF equals (cardiac output − coronary flow). TPR is calculated from [(arterial pressure − central venous pressure)/AoBF]. Abbreviations and sampling points are as in Fig. 13
Tonic control by the renal function
In contrast, the long-term stabilization mechanism for resting blood pressure may not be regulated solely by signals that can be easily fluctuated, such as nerves and hormones. It might also be circumscribed by factors like structural alternatives that cannot be directly fluctuated, such as vascular structure. It may probably be the case that “stubborn” tonic control systems are adopted as a life support mechanism (Fig. 12b). The pressure diuresis function of the kidneys may be one such system. Although the mechanism is not completely understood, one aspect of diuresis and blood pressure regulation occurs as a result of a relatively simple pressure-related physical force [45], which is powerful as a long-term blood pressure regulation mechanism in an open system [46]. However, when hypertension has developed, the renal function curve shifts to high blood pressure [47, 48], with the result that the high blood pressure cannot return to the normal level. Another aspect separate from the kidneys may be related to local regulation in the vessels and long-term regulation of that network. This is discussed in the following paragraphs.
Local control theory
Local regulation mechanisms have come to be included in research efforts in recent years. As shown in Table 2, regulation of vascular smooth muscle contraction by vascular endothelial cells has been shown by a number of investigators [49–62] since about 1956. However, as stated by Swales [55] in 1987, there were questions about the “competence” of such a mechanism. Regulation of vascular smooth muscle contraction by vascular endothelial cells attracted much attention with the discovery of nitric oxide (NO) in 1980. The discoveries of endothelin [61] and the C-type natriuretic peptide (CNP) [62] further advanced this concept, which has come to be established as a local regulation mechanism.
The commander for the local regulation mechanism is the local cell population, consisting mainly of vascular endothelial cells; it is not located in the central nerves. Signals generated in local endothelial cells (cytokines in the sense of physiologically active substances secreted by cells) act as paracrine signals in nearby smooth muscle cells, characterized by control. Of course, they also respond to circulating hormones and sympathetic nerves, but the main actors are locally generated signals. A typical example is coronary circulation, which, although affected by autonomic nerves and hormones, is mainly controlled by locally produced adenosine and NO. The vasodilatory action from these signals considerably exceeds the constriction effect from nerves and hormones [63]. Based on this mechanism, the heart itself can set the blood flow volume to the heart according to its own workload [63]. No matter what the “central authority” says, the “outlying regions” have their own circumstances and cannot do what they cannot do. Unless the entrusted “regional” mission is fulfilled with “regional” power, the overall life of the individual will not exist.
Reconstruction of concept of regulation system
With the addition of such local regulation mechanisms, there are understood to be three main mechanisms that contribute to the regulation of blood pressure: (1) feedback regulation based on information from baroreceptors, (2) central drive regulation from central nerves in the limbic system and hypothalamus of the brain and elsewhere, as well as central nerves that regulate functions other than circulation, and (3) local regulation based on local circumstances and features (Fig. 15).
Can the local control system regulate systemic blood pressure?
Chen and Sanders [64] administered l-arginine orally to Dahl salt-sensitive hypertensive rats and reported that the hypertension improved with a high-salt diet. This effect was not seen with d-arginine. The arteries of the Dahl rats with hypertension induced by high-salt intake were removed, then its vasoconstrictivity was examined by the Magnus method. The results revealed that they had greater constrictive activity [65] (Fig. 16). Further investigation showed that NO production capacity of the vascular endothelial cells had decreased and that the NO responsiveness of vascular smooth muscle had decreased [65]. Lüscher et al. [66] and Hayakawa [67] reported similar findings. Thus, abnormality of the local regulatory function of NO production by vascular endothelial cells leads to the long-term blood pressure regulation abnormality of salt-sensitive hypertension, and if the local abnormality is resolved, hypertension can be greatly corrected [64]. A similar disorder of vascular endothelial cell NO production was also indicated in the spontaneously hypertensive rat (SHR) [68]. Not only NO but also endothelin production and secretion disorders have been pointed out in such cases [69–71]. In addition, a novel special vasoconstrictive factor has been discovered in salt-sensitive hypertension [72]. While local regulatory abnormalities are too numerous to list here, they show general arterial pressure abnormalities resulting from local or target tissue abnormalities.
Contractions evoked by norepinephrine (NE, 10−8 to 10−6 M) in aortic rings of rats in the 4 groups, modified from Ref. [65]. DS-8% rats Dahl salt-sensitive rats fed 8% NaCl diet (n = 10); DS-0.4% rats Dahl salt-sensitive rats fed 0.4% NaCl diet (n = 12); DR-8%, 0.4% rats Dahl salt-resistant rats fed 8 or 0.4% NaCl diet (n = 12, 10, respectively); ED50 half maximal responses, Emax maximum responses. *p < 0.05 between high-salt and normal-salt Dahl salt-sensitive rats
The sympathetic center
What then is happening with control by the central and sympathetic nervous systems at this time? Are abnormalities also occurring on the controller side? When NO synthase (NOS) and 7-nitroindazole were administered intraperitoneally to salt-sensitive hypertensive rats and NO production was blocked, it was found that renal sympathetic nerve activity was increased even though blood pressure had become even higher (Fig. 17). The increase in sympathetic activity was surprisingly large and occurred at a level of the generator site of the rostral ventrolateral medulla, based on the data from the suppressing study of the baroreflex [73]. Thus, in salt-sensitive hypertension, the sympathetic nerve activity inhibiting mechanism was strongly amplified centrally via nNOS neurons. Since then, results have shown that compensatory mechanisms for hypertension are amplified centrally. However, since 7-nitroindazole lacks specificity for neuronal NOS (nNOS) [74, 75], and the action of inhibitors is not limited to central nerves with general administration, a change was made to s-methyl-l-thiocitrulline, which has a high specificity for nNOS. It was administered intra-cerebroventricularly, and, as expected, sympathetic nerve inhibition was seen due to amplification of central nNOS in salt-sensitive hypertensive rats (Fig. 18) [76]. Moreover, it was found that nerve nuclei that were strongly related to the inhibition of sympathetic nerve activity showed a rise in nNOS activity (Fig. 19) [77]. It thus appears that in high-salt hypertension the inhibitory limb in the sympathetic center is strongly enhanced. In other words, it has been shown that in salt-sensitive hypertension there are disorders in the local regulation mechanism and not in the regulation center, and rather that the sympathetic nerve centers respond as if compensating (Fig. 20).
Analog recordings showing responses of arterial pressure (AP), mean arterial pressure (MAP), heart rate (HR), renal sympathetic nerve activity (RSNA), and mean RSNA to a ramp decrease in MAP by caval occlusion (Oc) before and after intraperitoneal administration of 7-nitroindazole (nNOS inhibitor, 307 μmol/kg) in a hypertensive Dahl salt-sensitive rat. PE phenylephrine (15 μg/kg) intravenously, modified from Ref. [73]
Analog recordings showing responses of arterial pressure (AP), mean arterial pressure (MAP), heart rate (HR), renal sympathetic nerve activity (RSNA), and mean RSNA to a ramp decrease in MAP by caval occlusion (Oc) after the intracerebroventricular (icv) infusion of artificial cerebrospinal fluid (aCSF), and then of s-methyl-l-thiocitrulline (SMTC, 50 nmol), and l-arginine (l -Arg, 1,000 nmol), modified from Ref. [76]. Each arrow indicates a peak response of mean RSNA to a ramp decrease in MAP by caval occlusion, modified from Ref. [76]
Distribution of neurons containing neuronal nitric oxide synthase (nNOS neurons) in the rat brain, modified from Ref. [77]. Red bars nNOS neuronal area where its number was increased in salt-sensitive hypertensive rats compared with salt-sensitive normotensive rats. Red characters of the name show the part of sympathetic center. Numbers are the plate number in the book by George Paxinos, The Rat Brain in Stereotaxic Coordinates, London: Academic, 1988). PVN paraventricular nucleus, SON supraoptic nuecleus, DMH dorsomedial hypothalamus, PAG periaqueductal grey matter, PB parabrachial nucleus, NTS nucleus tractus solitarius, RM raphe magnus, RVLM rostral ventrolateral medulla, CVLM caudal ventrolateral medulla, CPA caudal pressor area, IML intermediolateral column
Central disturbances in essential hypertension
However, it is also well known that peripheral sympathetic nerve activity is elevated in patients with essential hypertension [78]. It has been reported that patients with spontaneous and essential hypertension have a genetic overexpression of the inflammation precursor JAM-1 in vascular endothelial cells in solitary tract nuclei of the brainstem, which results in hypertension [79]. It has also come to be thought that active enzymes produced by inflammatory reactions or immune responses, or oxidative stress, act on central nerves via circumventricular organs, particularly the AV3V region, raising sympathetic nerve activity and producing hypertension [80]. Meanwhile, inflammatory oxidative stress of peripheral vessels has also come to be included as a cause of hypertension [80]. These findings indicate that faulty control of central nerves plays a main role in conditions such as essential hypertension and SHR. If at this time sympathetic nerve activity is again enhanced in a similar manner to the case of salt-sensitive hypertension, a question is whether this will still be overcome, even though sympathetic nerve inhibition due to central nNOS causes peripheral nerve activity to increase. The answer to this will have to await further research. Conversely, another question is whether there are central abnormalities due to oxidative stress in salt-sensitive hypertension, as seen in SHR. This answer will also have to wait for further research.
Conclusion
The mechanisms of long-term blood pressure regulation remain unresolved. The quest for understanding needs to keep moving forward, even in small steps. There are two main types of blood pressure regulation, homeodynamic regulation and homeostatic regulation; it may be that the two missions of circulation are fulfilled by these two types of regulation (Fig. 21). To achieve the purpose of the former of integrating the differentiated functions into one, the systemic media of nerves and hormones based on a central drive with compromise or cooperation is used. The latter also uses the systemic media of nerves or hormones so as not to exceed a certain line, based on short-term feedback regulation. Long-term regulation, however, might be achieved by a local regulation network or harmonization.
Conceptual scheme for the meaning and method of blood pressure control. The blood pressure control system has separate functions for two biological missions. One is homeodynamic regulation by feed-forward control for the ‘all for one’ theory. The other is homeostatic regulation by feedback control and local control for the support of life
Perspectives
The peripheral resistance vessels that are the “sites” of local regulation are given the two jobs simultaneously of maintaining the circulatory driving force for the entire body and attracting blood flow to the blood flow region that is governed by that vessel. If a vessel is constricted, the former role can be fulfilled but the latter cannot. If a vessel is dilated, the latter role can be fulfilled but the former cannot. Peripheral resistance vessels are given the mission of balancing this tradeoff (Fig. 22). Of course, the blood flow distribution within tissue is left to the precapillaries by resistance vessels, but if the resistance vessels constrict, no blood flow above that level is produced in precapillary resistance of the control region. In addition to the mission of balancing this tradeoff, a dilemma is also produced by a clash between central control via nerves and hormones and local regulatory control. It is an extremely difficult situation. If the vessels of a given organ thicken and sufficient blood flow is not obtained with normal arterial pressure, the systemic blood pressure must unavoidably be raised in the long term [81]. Once blood pressure increases over a long period, systemic arteriosclerosis progresses and blood pressure is forced to go even higher. It is a vicious spiral. In consideration of this, one starts to think that perhaps the tradeoff mission may be formed by chance. This area may be a huge source of frustration for the “blood pressure regulation” researcher. While striving to solve this problem, if 120/80 mmHg is taken as the value that meets the needs for existence in the earth’s environment, where will that value settle if future generations of humans come to live in zero gravity or very low gravity environments?
References
Cowley AW Jr (1992) Long-term control of arterial blood pressure. Physiol Rev 72:231–300
Malpas SC (2004) What sets the long-term level of sympathetic nerve activity: is there a role for arterial baroreceptors? Am J Physiol Regul Integr Comp Physiol 286:R1–R12
Osborn JW (2005) Hypothesis: set-points and Long-term control of arterial pressure. A theoretical argument for a long-term arterial pressure control system in the brain rather than the kidney. Clin Exp Pharmacol Physiol 32:384–393
Kangawa K, Tawaragi Y, Oikawa S, Mizuno A, Sakuragawa Y, Nakazato H, Fukuda A, Minamino N, Matsuo H (1984) Identification of rat gamma atrial natriuretic polypeptide and characterization of the cDNA encoding its precursor. Nature 312:152–155
Kitamura K, Kangawa K, Kawamoto N, Ichiki Y, Nakamura S, Matsuo H, Eto T (1993) Adrenomedullin: a novel hypotensive peptide isolated from human pheochromocytoma. Biochem Biophys Res Commun 192:553–560
Hamlyn JM (1989) Increased levels of a humoral digitalis-like factor in deoxycorticosterone acetate-induced hypertension in the pig. J Endocrinol 122:409–420
Yanai K, Hirota K, Taniguchi-Yanai K, Shigematsu Y, Shimamoto Y, Saito T, Chowdhury S, Takiguchi M, Arakawa M, Nibu Y, Sugiyama F, Yagami K, Fukamizu A (1999) Regulated expression of human angiotensinogen gene by hepatocyte nuclear factor 4 and chicken ovalbumin upstream promoter-transcription factor. J Biol Chem 274:34605–34612
Ishida J, Sugiyama F, Tanimoto K, Taniguchi K, Syouji M, Takimoto E, Horiguchi H, Murakami K, Yagami K, Fukamizu A (1998) Rescue of angiotensinogen-knockout mice. Biochem Biophys Res Commun 252:610–616
Tsuchida S, Matsusaka T, Chen X, Okubo S, Niimura F, Nishimura H, Fogo A, Utsunomiya H, Inagami T, Ichikawa I (1998) Murine double nullizygotes of the angiotensin type 1Α and 1B receptor genes duplicate severe abnormal phenotypes of angiotensinogen nullizygotes. J Clin Invest 101:755–760
Ito M, Oliverio MI, Mannon PJ, Best CF, Maeda N, Smithies O, Coffman TM (1995) Regulation of blood pressure by the type 1A angiotensin II receptor gene. Proc Natl Acad Sci USA 92:3521–3525
Hein L, Barsh GS, Pratt RE, Dzau VJ, Kobilka BK (1995) Behavioural and cardiovascular effects of disrupting the angiotensin II type-2 receptor in mice. Nature 377:744–747
Carlson SH, Oparil S, Chen YF, Wyss JM (2002) Blood pressure and NaCl-sensitive hypertension are influenced by angiotensin-converting enzyme gene expression in transgenic mice. Hypertension 39:214–218
Gardiner SM, Bennett T, Compton AM (1988) Regional haemodynamic effects of neuropeptide Y, vasopressin and angiotensin II in conscious, unrestrained, Long Evans and Brattleboro rats. J Auton Nerv Syst 24:15–27
Madeddu P, Milia AF, Salis MB, Gaspa L, Gross W, Lippoldt A, Emanueli C (1998) Renovascular hypertension in bradykinin B2-receptor knockout mice. Hypertension 32:503–509
John SW, Veress AT, Honrath U, Chong CK, Peng L, Smithies O, Sonnenberg H (1996) Blood pressure and fluid-electrolyte balance in mice with reduced or absent ANP. Am J Physiol 271:R109–R114
Lopez MJ, Wong SK, Kishimoto I, Dubois S, Mach V, Friesen J, Garbers DL, Beuve A (1995) Salt-resistant hypertension in mice lacking the guanylyl cyclase-A receptor for atrial natriuretic peptide. Nature 378:65–68
Holtwick R, Gotthardt M, Skryabin B, Steinmetz M, Potthast R, Zetsche B, Hammer RE, Herz J, Kuhn M (2002) Smooth muscle-selective deletion of guanylyl cyclase-A prevents the acute but not chronic effects of ANP on blood pressure. Proc Natl Acad Sci USA 99:7142–7147
Shindo T, Kurihara Y, Nishimatsu H, Moriyama N, Kakoki M, Wang Y, Imai Y, Ebihara A, Kuwaki T, Ju KH, Minamino N, Kangawa K, Ishikawa T, Fukuda M, Akimoto Y, Kawakami H, Imai T, Morita H, Yazaki Y, Nagai R, Hirata Y, Kurihara H (2001) Vascular abnormalities and elevated blood pressure in mice lacking adrenomedullin gene. Circulation 104:1964–1971
Potthast R, Ehler E, Scheving LA, Sindic A, Schlatter E, Kuhn M (2001) High salt intake increases uroguanylin expression in mouse kidney. Endocrinology 142:3087–3097
Kaide J, Ura N, Torii T, Nakagawa M, Takada T, Shimamoto K (1999) Effects of digoxin-specific antibody Fab fragment (Digibind) on blood pressure and renal water-sodium metabolism in 5/6 reduced renal mass hypertensive rats. Am J Hypertens 12:611–619
Nishida Y (1994) Nuuro-humoral interactions by vasopressin or angiotensin II (in Japanese). Jpn J Circ Res 17:55–64
Abboud FM, Aylward PE, Floras JS, Gupta BN (1986) Sensitization of aortic and cardiac baroreceptors by arginine vasopressin in mammals. J Physiol 377:251–265
Schmid PG, Guo GB, Abboud FM (1985) Different effects of vasopressin and angiotensin II on baroreflexes. Fed Proc 44:2388–2392
Munch PA, Longhurst JC (1991) Bradykinin increases myocardial contractility: relation to the Gregg phenomenon. Am J Physiol 260:R1095–R1103
Yang TE, Cheng J, Levy MN (1990) Effects of the spatial dispersion of acetylcholine release on the chronotropic responses to vagal stimulation in dogs. Circ Res 67:844–851
Wang BC, Ginter GF, Goetz KL (1987) Augmented pressor response to vasopressin in awake dogs after cardiac denervation. Am J Physiol 252:R145–R152
Brizzee BL, Walker BR (1990) Vasopressinergic augmentation of cardiac baroreceptor reflex in conscious rats. Am J Physiol 258:R860–R868
Scott JA, Konstam M, Kolodny GM (1982) Absence of a direct chronotropic effect of vasopressin on the myocardial cell. Pharmacology 24:57–60
Imaizumi T, Thames MD (1986) Influence of intravenous and intracerebroventricular vasopressin on baroreflex control of renal nerve traffic. Circ Res 58:17–25
Undesser KP, Hasser EM, Haywood JR, Johnson AK, Bishop VS (1985) Interaction of vasopressin with the area postrema in arterial baroreflex function in conscious rabbits. Circ Res 56:410–417
Hasser EM, Bishop VS (1990) Reflex effect of vasopressin after blockade of V1 receptors in the area postrema. Circ Res 67:265–271
Nishida Y, Bishop VS (1992) Vasopressin-induced suppression of renal sympathetic outflow depends on the number of baroafferent inputs in rabbits. Am J Physiol Regul Integr Comp Physiol 263:R1187–R1194
Nishida Y, Hosomi H, Bishop VS (1993) Sympathetic outflow requires tonic baroafferent input stimuli in rabbit. In: Terui N, Suzuki H (eds) Central nervous system and blood pressure control: proceedings of the 7th workshop on “brain and blood pressure control, 1992”. Yubunsha, Tokyo
Nishida Y, Ryan KL, Bishop VS (1995) Angiotensin II modulates arterial baroreflex function via a central α 1-adrenoceptor mechanism in rabbits. Am J Physiol Regul Integr Comp Physiol 269:R1009–R1016
Bishop VS, Ryuzaki M, Cai Y, Nishida Y, Cox BF (1995) Angiotensin II-dependent hypertension and the arterial baroreflex. Clin Exp Hypertens 17:29–38
Murakami H, Liu JL, Yoneyama H, Nishida Y, Okada K, Kosaka H, Morita H, Zucker IH (1998) Blockade of neuronal nitric oxide synthase alters the baroreflex control of heart rate in the rabbit. Am J Phyiol Regul Integr Comp Physiol 274:R181–R186
Nishida Y, Hosomi H, Bishop VS (1997) Long-term effects of AVP-induced neurohumoral interaction via area postrema on body fluid and blood pressure. Am J Physiol Regul Integr Comp Physiol 273:R1696–R1703
Cowley AW Jr, Liard JF, Guyton AC (1973) Role of the baroreceptor reflex in daily control of arterial blood pressure and other variables in dogs. Circ Res 32:564–576
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL et al (2003) The National High Blood Pressure Education Program Coordinating Committee. Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. JAMA 289:2560–2572
Osborn JW, Hornefeldt BJ (1998) Arterial baroreceptor denervation impairs long-term regulation of arterial pressure during dietary salt loading. Am J Physiol Heart Circ Phyiol 275:H1558–H1566
Jacob F, Ariza P, Osborn JW (2003) Renal denervation chronically lowers arterial pressure independent of dietary sodium intake in normal rats. Am J Physiol Heart Circ Physiol 284:H2302–H2310
Osborn JW, Jacob F, Guzman P (2005) A neural setpoint for the long-term control of arterial pressure: beyond the arterial baroreceptor reflex. Am J Physiol Regul Integr Comp Physiol 288:R846–R855
Miki K, Yoshimoto M, Tanimizu M (2003) Acute shifts of baroreflex control of renal sympathetic nerve activity induced by tredmill exercise in rats. J Physiol 548:313–322
Nishida Y, Chen QH, Zhou MS, Horiuchi J (2002) Sinoaortic denervation abolishes pressure resetting for daily physical activity in rabbits. Am J Physiol Regul Integr Comp Physiol 282:R649–R657
Guyton AC (1987) Renal function curve—a key to understanding the pathogenesis of hypertension. Hypertension 10:1–6
Dorrington KL, Pandit JJ (2009) The obligatory role of the kidney in long-term arterial blood pressure control: extending Guyton’s model of the circulation. Anesthesia 64:1218–1228
Hall JE (1991) Renal function in one-kidney, one-clip hypertension and low renin essential hypertension. Am J Hypertens 4:523S–533S
Kimura G, Brenner BM (1997) Implications of the linear pressure-natriuresis relationship and importance of sodium sensitivity in hypertension. J Hypertens 15:1055–1061
Dengler H (1956) Renin-like active substance in artery extracts (in German). Naunyn Schmiedebergs Arch Exp Pathol Pharmakol 227:481–487
Ganten D, Minnich JL, Granger P, Hayduk K, Brecht HM, Barbeau A, Boucher R, Genest J (1971) Angiotensin-forming enzyme in brain tissue. Science 173:64–65
Fischer-Ferraro C, Nahmod VE, Goldstein DJ, Finkielman S (1971) Angiotensin and renin in rat and dog brain. J Exp Med 133:353–361
Ganten D, Schelling P, Vecsei P, Ganten U (1976) Iso-renin of extrarenal origin. “The tissue angiotensinogenase systems”. Am J Med 60:760–772
Dzau VJ (1984) Vascular renin–angiotensin: a possible autocrine or paracrine system in control of vascular function. J Cardiovasc Pharmacol 6:S377–S382
Oliver JA, Sciacca RR (1984) Local generation of angiotensin II as a mechanism of regulation of peripheral vascular tone in the rat. J Clin Invest 74:1247–1251
Swales JD, Heagerty AM (1987) Vascular renin–angiotensin system: the unanswered questions. J Hypertens Suppl 5:S1–S5
Inagami T, Mizuno K, Nakamaru M, Pandey KN, Naruse M, Naruse K, Misono K, Okamura T, Kawamura M, Higashimori K (1988) The renin–angiotensin system: an overview of its intracellular function. Cardiovasc Drugs Ther 2:453–458
Urata H, Kinoshita A, Misono KS, Bumpus FM, Husain A (1990) Identification of a highly specific chymase as the major angiotensin II-forming enzyme in the human heart. J Biol Chem 265:22348–22357
Ju H, Gros R, You X, Tsang S, Husain M, Rabinovitch M (2001) Conditional and targeted overexpression of vascular chymase causes hypertension in transgenic mice. Proc Natl Acad Sci USA 98:7469–7474
Bunting S, Gryglewski R, Moncada S, Vane JR (1976) Arterial walls generate from prostaglandin endoperoxides a substance (prostaglandin X) which relaxes strips of mesenteric and coeliac arteries and inhibits platelet aggregation. Prostaglandins 12:897–913
Furchgott RF, Zawadzki JV (1980) The obligatory role of endothelial cells in the relaxation of arterial smooth muscle by acetylcholine. Nature 288:373–376
Yanagisawa M, Kurihara H, Kimura S, Tomobe Y, Kobayashi M et al (1988) A novel potent vasoconstrictor peptide produced by vascular endothelial cells. Nature 332:411–415
Sudoh T, Minamino N, Kangawa K, Matsuo H (1990) C-type natriuretic peptide (CNP): a new member of natriuretic peptide family identified in porcine brain. Biochem Biophys Res Commun 168:863–870
Duncker DJ, Bache RJ (2008) Regulation of coronary blood flow during exercise. Physiol Rev 88:1009–1086
Chen PY, Sanders PW (1991) l-arginine abrogates salt-sensitive hypertension in Dahl/Rapp rats. J Clin Invest 88:1559–1567
Nishida Y, Ding J, Zhou MS, Chen QH, Murakami H, Wu XZ et al (1998) Role of nitric oxide in vascular hyper-responsiveness to norepinephrine in hypertensive Dahl rats. J Hypertens 16:1611–1618
Lüscher TF, Vanhoutte PM, Raij L (1987) Antihypertensive treatment normalizes decreased endothelium-dependent relaxations in rats with salt-induced hypertension. Hypertension 9:193–197
Hayakawa H, Raij L (1997) The link among nitric oxide synthase activity, endothelial function, and aortic and ventricular hypertrophy in hypertension. Hypertension 29:235–241
Rizzoni D, Porteri E, Piccoli A, Castellano M, Bettoni G, Muiesan ML et al (1998) Effects of losartan and enalapril on small artery structure in hypertensive rats. Hypertension 32:305–310
Kassab S, Miller MT, Novak J, Reckelhoff J, Clower B, Granger JP (1998) Endothelin-A receptor antagonism attenuates the hypertension and renal injury in Dahl salt-sensitive rats. Hypertension 31:397–402
Barton M, d’Uscio LV, Shaw S, Meyer P, Moreau P, Lüscher TF (1998) ET(A) receptor blockade prevents increased tissue endothelin-1, vascular hypertrophy, and endothelial dysfunction in salt-sensitive hypertension. Hypertension 31:499–504
Ergul A (2000) Hypertension in black patients: an emerging role of the endothelin system in salt-sensitive hypertension. Hypertension 36:62–67
Zhou MS, Nishida Y, Chen QH, Kosaka H (1999) Endothelium-derived contracting factor in carotid artery of hypertensive Dahl rat. Hypertension 34:39–43
Nishida Y, Chen QH, Tandai-Hiruma M, Terada S, Horiuchi J (2001) Neuronal NO strongly suppresses sympathetic outflow in high salt-Dahl rats. J Hypertens 19:627–634
Zagvazdin Y, Sancesario G, Wang YX, Share L, Fitzgerald ME, Reiner A (1996) Evidence from its cardiovascular effects that 7-nitroindazole may inhibit endothelial nitric oxide synthase in vivo. Eur J Pharmacol 303:61–69
Babbedge RC, Bland-Ward PA, Hart SL, Moore PK (1993) Inhibition of rat cerebellar nitric oxide synthase by 7-nitro indazole and related substituted indazoles. Br J Pharmacol 110:225–228
Tandai-Hiruma M, Horiuchi J, Sakamoto H, Kemuriyama T, Hirakawa H, Nishida Y (2005) Brain nNOS neuron-mediated sympathoinhibition is enhanced in hypertensive Dahl rats. J Hypertens 23:825–834
Nishida Y, Tandai-Hiruma M, Kemuriyama T, Sato Y, Tsukada S, Maruyama S, Ideda T, Kato K (2007) Central nNOS neuron-mediated sympathetic regulation in salt-sensitive hypertension. In: Kubo T, Kuwaki T (eds) Central mechanisms of cardiovascular regulation. Transworld Research Network, Kerala
Matsukawa T, Mano T, Gotoh E, Ishii M (1993) Elevated sympathetic nerve activity in patients with accelerated essential hypertension. J Clin Invest 92:25–28
Waki H, Gouraud SS, Maeda M, Paton JF (2008) Specific inflammatory condition in nucleus tractus solitarii of the SHR: novel insight for neurogenic hypertension? Auton Neurosci 142:25–31
Harrison DG, Guzik TJ, Lob HE, Madhur MS, Marvar PJ, Thabet SR et al (2011) Inflammation, immunity, and hypertension. Hypertension 57:132–140
Johnson RJ, Feig DI, Nakagawa T, Sanchez-Lozada L, Rodriguez-Iturbe B (2008) Pathogenesis of essential hypertension: historical paradigms and modern insights. J Hypertens 26:381–391
Acknowledgments
The authors wish to thank Koichi Fukuda and his associates in Animal Research Laboratory of National Defense Medical College for supporting animal research. The investigations were supported in part by The Salt Science Research Foundation, Grant #0338, 0435, 0535, National Defense Medical College Special Grant 2007–2009 and Grants-in-Aid for Scientific Research [C 11009567] from the Ministry of Education, Science, Sports and Culture of Japan. There is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Nishida, Y., Tandai-Hiruma, M., Kemuriyama, T. et al. Long-term blood pressure control: is there a set-point in the brain?. J Physiol Sci 62, 147–161 (2012). https://doi.org/10.1007/s12576-012-0192-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12576-012-0192-0