Abstract
Voluntary muscle contractions activate sympathetic efferent pathways. Using a fatiguing electrical stimulation protocol designed specifically to enhance sympathetically-mediated vasoconstrictor tone, we explored the temporal profile and mechanistic bases of the evoked vasoconstrictor response and its role in muscle fatigue. Spinotrapezius muscles of Wistar rats were exteriorized and stimulated tetanically (100 Hz, 6–8 V, stimulus duration 700 ms) every 3 s for 2.5 min. The extent and time course of diameter changes in arterioles (1A and 2A) and venules (1V and 2V) were determined after each of 10 discrete sets of muscle stimulation at 5-min intervals. At first, to compare the effect of stimulation parameters in this preparation, stimulations were performed with rectangular pulses of either 0.2- or 4-ms pulse duration. As expected the 0.2-ms pulse stimulation did not affect arteriolar diameter or muscle fatigability. In contrast, during and following 4-ms pulse stimulations, there was a surprising arteriolar vasoconstriction rather than the expected vasodilation. Arteriolar (but not venular) vasoconstriction (reduced arteriolar diameter by 38.6 ± 2.6% in the 10th set) increased progressively with muscle fatigue (to 29 ± 12% of initial tension in the 10th set) for the 4-ms pulse condition. Superfusion with the selective α1-adrenergic receptor antagonist prazosin (1 μM) and/or α2-adrenergic receptor antagonist rauwolscine (10 μM) abolished both the arteriolar vasoconstriction and significantly reduced fatigue (i.e., % initial tension, α1: 46.8 ± 10.3%; α2: 39.0 ± 5.8%; α1 + α2: 48.7 ± 16.3% in the 10th set; all P < 0.05 vs. control). We conclude that sequential bouts of contractions induce a progressively greater degree of α-adrenergic receptor-induced arteriolar (but not venular) vasoconstriction which contributes significantly to fatigue in this model.
Similar content being viewed by others
Introduction
Skeletal muscle blood flow increases in proportion to the metabolic demands during exercise [2]. Although muscle blood flow increases in an exercise intensity-dependent manner, muscle sympathetic nerve activity also increases in the same manner [12, 25]. Sympathetic activation plays an important role in the distribution of blood flow during exercise by causing vasoconstriction in non-exercising tissue. In addition, sympathetic activation is likely to be the mechanism by which increased respiratory muscle work and fatigue reduces blood flow and performance in locomotory muscles [1, 10, 11, 15, 28, 31]. Half a century ago, Remensnyder et al. [27] coined the term ‘functional sympatholysis’ to describe the relative insensitivity of the exercising muscle vascular bed to sympathetic vasoconstriction. However, despite the presence of functional sympatholysis, some sympathetic vasoconstriction may still constrain the increase of muscle blood flow during exercise [6, 12, 14, 29]. Although controversial, there is evidence that sympathetic activation leading to vasoconstriction is attenuated in the active muscles, in part due to an effect of muscle metabolites and nitric oxide which act to diminish the vasoconstrictor response to α-adrenergic receptor activation [3, 7, 35–37]. However, it has not been established whether such increases of sympathetic nerve activity or alternatively reduced functional sympatholysis mediate the attenuated vasodilator response observed during muscle fatigue evoked by repeated bouts of tetanic contractions [3, 7, 35–37].
Previous studies suggest that α-adrenergic receptors play an important role in functional sympatholysis during exercise [7, 36]. Furthermore, it is well known that an inverse relationshiip exists for resistance vessel diameter and the sensitivity to sympathetically-mediated vasoconstriction [5, 22, 26]. Specifically, in the rat cremaster muscle, Ohyanagi et al. [26] demonstrated that during sympathetic nerve stimulation the effect of inhibiting α1- and α2-adrenergic receptors was different in large (1A) versus small (3A) arterioles. The distribution of α-adrenergic receptors is stratified along the arterial tree, and both α1 and α2 have been implicated in vascular control during contractions. Thus, it is necessary to use specific antagonists in order to examine effectively the role of each α-adrenergic receptor on vasomotor control during contractions.
The purpose of the present investigation was to explore the role of functional sympatholysis on vasomotor control and fatigue during and following isometric tetanic contractions in the rat spinotrapezius muscle microcirculation. Specifically, using a stimulation protocol designed to increase sympathetically-mediated vasoconstrictor tone in combination with α-adrenergic blockade (prazosin and/or rauwolcine), we tested the hypotheses that: (1) fatiguing contractions would alter the vasoconstriction–vasodilation balance towards vasoconstriction; and (2) this vasoconstriction would be partially or wholly ablated by α1 and/or α2 receptor antagonism and fatigue would be reduced.
Methods
Animal care and preliminary surgery
Male Wistar rats (n = 30, 9–15 weeks of age; Japan SLC) were used in this study. All procedures were approved by the University of Electro-Communications Institutional Animal Care and Use Committee and conducted under the guidelines established by the Physiological Society of Japan. Rats were maintained at 24°C on a 12:12-h light:dark cycle and received food and water ad libitum. Surgical procedures were performed under a stereo microscope. Rats were anaesthetized with sodium pentbarbital (70 mg/kg i.p.) and supplemental doses of anesthesia were administered as needed during surgery. Cannulae were secured in the right carotid artery to monitor blood pressure. Body temperature was maintained near 37°C by placing the animal on a heating pad during surgery. At the end of the experimental protocol, animals were sacrificed by pentobarbital sodium overdose.
Muscle preparation
Following preliminary surgery, the right spinotrapezius muscle was prepared for in vivo microscopic observation as previously described [19, 32, 33]. This muscle has been likened to the human quadriceps femoris with respect to containing each of the major muscle fiber types and possesses a similar oxidative capacity [9, 21] which strengthens its relevance to understanding vascular control in humans. Exteriorization of the right spinotrapezius muscle, accessed through a midline incision, was performed with as little disruption as possible to minimize tissue damage. The exposed tissue was kept moist by superfusing with warmed Krebs–Henseleit buffer solution (KHB; 132 NaCl, 4.7 KCl, 21.8 NaHCO3, 2 MgSO4, 2 CaCl2 mM), equilibrated with 95% N2–5% CO2 and adjusted to pH 7.35–7.4, at 37°C. Loose connective tissue covering the muscle surface was carefully removed. The exposed spinotrapezius muscle with principal vascular and neural pathways maintained was attached to a wire horseshoe around the caudal periphery by 6 equidistant sutures placed around the caudal perimeter [19, 32, 33]. This procedure has been demonstrated not to impact the blood flow or O2 delivery-to-VO2 relationships at rest or in response to muscle contractions [4]. For the contraction protocols, two partially-insulated electrodes were placed on the dorsal spinotrapezius surface along the caudal periphery at least 10 mm away from the viewing area, facilitating whole muscle contractions. The fixed horse shoe attachment prevented reduction of the origin (scapula)-to-horseshoe insertion length of the muscle. However, some movement occurred during stimulation as the series elastic component allowed for a modest reduction of mean sarcomere length. After the surgical preparations, the rat was placed on a 37°C glass hotplate (Kitazato Supply, Japan) and mounted to reduce any movements due to breathing and cardiac contractions. Then, the rat was switched from pentobarbital to urethane (4 g; α-chloralose, 25 g; Urethan, 100 ml; Polyethylene Glycol 200, 2 ml/kg, i.p.) anesthesia.
Experimental protocols
Animals were allowed to stabilize for ~30 min after completion of the surgical procedure. Each spinotrapezius muscle was subjected to 10 discrete sets of isometric muscle stimulations in a manner similar to that described previously [32, 33]. Specifically, each set consisted of the muscle being stimulated tetanically, with isometric contractions evoked by trains of stimuli (700 ms duration, 100 Hz frequency) at 3 s intervals for 2.5 min (i.e., 50 contractions) interspersed with 5-min rest intervals using an electro-stimulator (model 3F46; NEC, Tokyo) via a stimulus isolation unit (model 5384; NEC). To excite the sympathetic nerve activity and muscle contractions simultaneously, stimulations were performed, unless otherwise stated, with rectangular pulses of 8 V and 4 ms duration [17, 20].
Protocol 1: effect of stimulation parameters
In the first experiment designed to compare the effect of stimulation parameters in this preparation, stimulations were performed with rectangular pulses of 8 V intensity and 4 ms duration (n = 8) or of 6 V intensity and 0.2 ms duration (n = 6).
Protocol 2: effect of pharmacological sympathetic nervous system activity inhibition
To investigate the role of sympathetic nerve activity during muscle fatigue, the selective α1-adrenergic receptor antagonist prazosin (1 μM, dissolved in KHB) and/or selective α2-adrenergic receptor antagonist rauwolscine (10 μM, dissolved in KHB), were added to the superfusion solution. These concentrations represented approximately the IC50 concentration to inhibit the vasoconstriction evoked with each agonist (10 μM phenylephrine, 10 μM clonidine and 10 μM norepinephrine) superfused in this preparation. Subsequently, spinotrapezius muscles were stimulated tetanically at resting sarcomere length under (1) control (rectangular pulses of 8 V intensity and 4-ms duration in protocol 1) and (2) prazosin (n = 6), (3) rauwolscine (n = 5) and (4) prazosin + rauwolscine (n = 5) superfused conditions.
In vivo measurements
Arterial pressure was monitored by computer throughout the experiment using a DTX Plus pressure transducer connected to Multi-channel Amplifier (Nihon Koden, Tokyo). Data were analyzed offline to calculate the absolute changes in mean arterial pressure (MAP) and heart rate (HR). To measure muscle force during contractions, the wire horseshoe that was attached to the spinotrapezius muscle was connected by a fine wire to a strain gauge. Torque (0–10 mN, full scale deflection) was monitored by computer using Mac Lab/8s (A/D Instruments, USA) via a strain gauge-linked motor device (Model RU-72; NEC) during all contraction protocols. In preliminary investigations, we determined that there was a certain modest variability in force production amongst different muscles presumably related to differences in muscle cross-sectional area and also architectural differences. Accordingly, as is standard in many investigations and to more clearly show the responses to the experimental conditions within and among groups, at any given time and condition, the force was expressed relative to the initial force for that muscle. Our preliminary investigations also determined that, in agreement with Honig and Frierson [17], there were no changes in force induced by different pulse width stimulations. In addition, in the same rat spinotrapezius muscles superfused in random order, there was no difference in absolute initial force induced by α-adrenergic blockade (0.2 ms: −8.4 ± 2.5%; prazosin: −1.8 ± 3.4%; rauwolscine: −8.4 ± 4.4%, compared with 4-ms pulse condition, P > 0.05 for all comparisons). Among the 10 sets of 50 contractions the first 5 and last 5 contractions of set numbers 1, 5 and 10 were averaged and plotted graphically as an index of fatigue.
The microcirculation of the spinotrapezius muscle was transilluminated and observed under an intravital microscope using a ×10 objective lens (0.30 numerical aperture; Nikon, Japan). The microscopic images were captured by a charge-coupled device digital camera (DP70; Olympus, Japan) and viewed at 1.55 pixel/μm using image-capture software (DP Control; Olympus). Vessels were classified according to location within the arteriolar network [22]. Briefly, the arterial vessels are arranged in two anastomosing networks, one composed of primary arterioles (22–50 μm, 1A) and the other of secondary arterioles (13–18 μm, 2A). Images of 1A or 2A arterioles and venules were obtained in the resting muscles every 5 s for the first minute and every 30 s for the next 4 min after each of 10 discrete sets of muscle contractions. Each designated captured area included the vessel branch and mean vessel diameters reported were the average diameters at 0, 50, and 100 μm upstream from each branch. Captured images were analyzed after the experiments using ImageJ software (National Institutes of Health, USA). The diameter measurements of arterioles and venules were reproducible to within ±1 μm.
Statistical analysis
All statistical analyses were performed in Prism version 4.0 (GraphPad Software, USA). A two-way repeated-measures ANOVA and Bonferroni post-hoc test were used for control versus each α-adrenergic receptor antagonist superfused condition. A one-way repeated-measures ANOVA and Bonferroni post-hoc test was used for comparison of relative force, MAP and HR among conditions. Peason product moment correlation coefficients (r) were calculated to evaluate the relationship between baseline diameter and vasoconstriction. Measured values are presented as mean ± SE. Significance was established at P < 0.05.
Results
Mean arterial pressure during the resting period was 90–110 mmHg and did not change significantly during superfusions and/or muscle contractions in any group (Table 1).
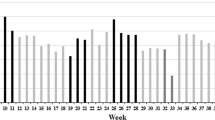
Figure 1 shows the changes of relative tetanic force production. In the 0.2-ms pulse duration condition, tetanic force decreased 20–40% within a set, and recovered to the initial level after each interval. Thus, there was no significant attenuation of the tetanic force at the initiation of subsequent contraction sets. In marked contrast, while the 4-ms pulse duration condition also demonstrates decreasing tetanic force within a given set, there was a progressive inability to recover the initial tension across sets such that, by the end of the final 10th set, tetanic force was decreased significantly to 21.4 ± 9.7% of initial force (P < 0.01).
Change of relative tetanic force during contraction protocols. Force normalized to initial (100%) denotes the average of first and last 5 contractions of sets 1, 5, and 10 from 0.2-ms pulse duration condition (closed circles) and 4-ms pulse duration condition (open circles). Values are means ± SE (0.2 ms: n = 5; 4 ms: n = 4). Significance compared with initial value for each condition: *P < 0.01
Figures 2 and 3 show the changes of arteriolar and venular inner diameter (relative to pre-contraction values) immediately after contractions in both conditions. In the 0.2-ms condition, arteriolar diameter did not change significantly and the changes were within 10%. In contrast, arteriolar vasoconstriction increased systematically with subsequent sets of contractions in the 4-ms condition, such that a significant decrease of arteriolar diameter was observed after 10 sets of contractions (−38.6% vs. pre-contraction, P < 0.01). In neither the 0.2-ms nor the 4-ms condition did venular inner diameter change significantly.
Captured images of arteriole before stimulation, after 1 set and 10 sets of contractions in 0.2- and 4-ms pulse duration conditions. Captured areas include the branch of each vessels, and mean vessel diameters were represented the average diameter of 0, 50, and 100 μm distance from each branch. Arrow indicates the 50-μm part of the analyzed arteriole. Bar 20 μm
Relative changes of arteriolar and venular diameter immediately after contractions. Arteriolar and venular diameter changes relative to pre-contraction values (which was unchanged during the course of the experiment) at sets 1, 5 and 10 from 0.2-ms pulse duration condition (open bars) and 4ms pulse duration condition (closed bars). Measurements were made immediately after contractions in each condition. Values are means ± SE. Significance compared with pre-contraction diameter for each condition: *P < 0.05
The time courses of change in arteriolar and venular inner diameter for 0.2- and 4-ms conditions during recovery are shown in Fig. 4. Specifically in the 4 ms condition, there was a tendency for arteriolar vasoconstriction after set 5 (−16.6 ± 1.4%) which reached significance after set 10 (−38.6 ± 2.6%). The time constant (τ) of diameter recovery also increased progressively with sets and after sets 5 and 10 was 25 ± 7 s and 46 ± 13 s (P < 0.05 between sets 5 and 10). The data for set 1 was not analyzed in this manner because no reduction was observed after stimulation. The relationship between arteriolar baseline diameter and vasoconstriction during fatigue in the 4-ms pulse duration condition is shown in Fig. 5. There was no correlation after 1 or 5 sets of contractions. However, a strong correlation became manifested after the 10th set as muscle fatigue became more extreme (Fig. 1).
Time course of arteriolar and venular diameter changes during recovery after 1, 5, and 10 sets for each contraction protocols. Values of vessel inner diameter are normalized to each pre-contracting baseline diameter which was unchanged during the time course of the experiment. In the 0.2- and 4-ms pulse duration conditions, relative arteriolar and venular diameter changes are shown. Values are means ± SE (0.2 ms: n = 6; 4 ms: n = 8)
The changes in relative tetanic force production during stimulation with superfused α-adrenergic receptor antagonists are shown in Fig. 6. Compared with control (4 ms), force attenuation was reduced substantially at the final set (i.e., 10th set: α1, 46.8 ± 10.3%; α2, 39.0 ± 5.8%; α1 + α2, 48.7 ± 16.3%). The time course of change in arteriolar inner diameter during recovery after the 1st, 5th and 10th sets for each α-adrenergic receptor inhibition condition is shown in Fig. 7. The progressive arteriolar vasoconstriction observed in subsequent bouts in the control conditions was almost completely abolished. This was especially evident with both α1- and α2-antagonists. Indeed, in this instance, the arteriolar inner diameter was more dilated after 10 sets of muscle contractions compared with sets 1 and 5.
Change of relative tetanic force during contraction protocols in alpha adrenergic blocker superfused condition. Force normalized to initial (set 1) denotes the average of first 5 and last 5 contractions from sets 1, 5, and 10 from all groups. Values shown are means ± SE. Significance compared with initial value for each group: *P < 0.05
Time course of arteriolar diameter changes during recovery after 1, 5, and 10 sets in alpha adrenergic blocker superfused condition. Values of vessel inner diameter normalized to each baseline diameter. Relative arteriolar diameter changes in α1 and α2 and combined (α1 and α2) α-antagonist conditions are shown. Values are means ± SE
Figure 8 shows the changes of arteriolar inner diameter (relative to pre-contraction values) immediately after contractions for sets 1, 5 and 10 in each condition. After 10 sets the significant decrease of luminal diameter observed in control was abolished by each α-adrenergic receptor antagonist.
Relative changes of arteriolar diameter immediately after contractions. Arteriolar diameter changes relative to pre-contraction values after sets 1, 5 and 10 for the control condition and each α-antagonist condition. Values are means ± SE. Significance compared with pre-contraction diameter for each condition: *P < 0.05
Discussion
The principal original finding of this investigation was that repetitive, fatiguing muscle contractions of the mixed fiber type spinotrapezius muscle [9] evoke a progressive vasoconstrictor response that is: (1) blocked by α1- and α2-adrenergic receptor antagonists, and (2) intimately associated with the fatigue process.
Effect of stimulation parameters
Static or isometric locomotor muscle contractions elicit the exercise pressor response, and MAP and HR are increase immediately after the onset of exercise [16, 23]. In this study, however, MAP and HR did not change significantly in the temporal proximity of the stimulations. This difference is likely to have resulted from the small size of the spinotrapezius muscle compared to locomotor muscles, and the fact that the stimulation protocol was localized to this muscle. Thus, circulating catecholamine concentrations and afferent nerve activity levels were not likely to change following stimulations. This paradigm isolates the response investigated to a degree not possible in conscious, voluntarily exercising rats where the balance of central and local vasomotor control may be uncertain.
Regarding the central purpose of the present investigation, Kjellmer [20] confirmed that sympathetic axons associated with the motor nerve are not activated by very short stimulus duration (0.1 ms) and it is generally accepted, and supported herein, that electric stimulation using shorter pulse duration excites skeletal muscle motor but not autonomic nerves. Additionally, Honig and Frierson [17] demonstrated that, in canine skeletal muscle, stimulation of obturator nerves with 2- and 5-ms pulses elicited maximal tension and arterial vasoconstriction, while 0.2- and 0.5-ms pulse stimulation elicited similar tension but a substantial and well-sustained vasodilation. In order to examine the functional sympatholysis phenomenon during exercise in anesthetized animals, it is necessary to elicit motor nerve stimulation and sympathetic nerve stimulation simultaneously. VanTeeffelen and Segal [38] examined the changes of proximal (FA and 1A) and distal arterioles (2A and 3A) directly using combined direct muscle stimulation and sympathetic stimulation in hamster retractor muscle. Thus, as contractile activity and sympathetic nerve activity (SNA) increased, total blood flow into the muscle was restricted progressively through constriction of feed artery and proximal arterioles while sympathetic vasoconstriction was antagonized by muscle contractions in the distal arterioles. Importantly, local stimulation of muscle fibres and sympathetic nerves did not change the systemic blood pressure [38]. In the present study, 0.2-ms pulse stimulation did not affect arteriolar diameter, while arteriolar vasoconstriction occurred progressively with increasing numbers of contraction sets in the 4-ms pulse stimulation condition. Rowell et al. [29] and Harms et al. [15] demonstrated the role of the SNA in limiting muscle blood flow during maximal exercise. Therefore, the 4-ms pulse stimulation condition likely serves to increase SNA and, as such decrease muscle blood flow, which we demonstrated exacerbated fatigue in the spinotrapezius muscle. If the muscle contracts in the absence of electrically-stimulated SNA with 0.2-ms pulses, there should have been a vasodilation and contraction-induced hyperemia. However, a definite vasodilator response was not observed in the 0.2-ms pulse stimulation condition. Whilst there were individual examples of arteriolar dilatation at our measurement sites (e.g., Fig. 3, left hand middle panel) it is probable that a more robust dilatator response may have occurred in more distal arterioles. At least one previous study [18] suggested that the exercise hyperemia for moderately intense contraction is likely controlled by downstream (i.e., 3A) rather than proximal (i.e., 1A) arterioles. According to Fig. 5, the smaller arterioles seemed to be more fatigue-sensitive than larger arterioles. The mechanistic bases of this phenomenon are still unclear, however, putative mechanisms include: (1) the distributions of α- adrenergic receptor subtypes are heterogeneous within the arteriolar tree, and (2) the magnitude of arteriolar sympathetic innervations may also be heterogeneous.
Effect of α-adrenoceptor blockade
Sympathetic nerves innervate feed arteries and arterioles throughout the rat spinotrapezius muscle microcirculation [22]. α2-adrenergic receptors are located predominantly in distal branches (3A) while both α1- and α2-adrenergic receptors are located in proximal arterioles (1A and 2A) [13]. Buckwalter et al. [7] demonstrated that exercise may attenuate both α1- and α2-mediated vasoconstriction in dog hindlimbs dependent, in part, upon its intensity: specifically, α2 responsiveness was blunted throughout mild to heavy exercise levels while α1-mediated vasoconstriction was attenuated only during heavy exercise. Moreover, α2 adrenergic receptor-mediated vasoconstriction is more sensitive than α1-mediated vasoconstriction to metabolic modulation such as decreases in PO2 (70–10 mmHg) and pH (7.4–7.0) [24, 34], or NO via KATP channel activation [35]. In the present study, there was a progressively greater degree of arteriolar vasoconstriction following stimulations. This vasoconstriction was attenuated substantially by both α1- and/or α2-adrenergic inhibition, and the effect of selective and non-selective α-adrenergic blockade on arteriolar inner diameter during and following stimulation was similar. Thus, the doses of both α-adrenergic receptor antagonists were sufficient to prevent the sympathetically-evoked vasoconstrictor response and yet, crucially, did not result in sufficient systemic spillover to impact MAP or HR regulation. However, a definitive vasodilator response was not observed in either α-adrenergic receptor antagonist superfusions until the 10 sets of contractions where blockade reduced the magnitude of vasoconstriction below that seen under control conditions. Our data suggest that the distribution of α1 and α2-adrenergic receptor in 1A and 2A arterioles of rat spinotrapezius muscle may be similar. On the other hand, the protocol devised for this study did not impact venous vessel diameter following muscle contractions and this finding is consistent with previous reports that venules are not under sympathetic control [22]. Also, this observation suggests that there was little or no change in muscle internal pressure, which, had it occurred, might be the consequence of mechanical alterations of the vasculature.
Functional sympatholysis during skeletal muscle fatigue
In the present study, there was a progressive sympathetic vasoconstriction with muscle fatigue. It has long been recognized that studying the interaction between functional vasodilation and sympathetic vasoconstriction is fundamental to understanding blood flow control during exercise. Although the local vasodilator responses override the sympathetic vasoconstriction during exercise, as fatigue increases, sympathetic vasoconstriction may become more pronounced. Saito et al. [30] showed that muscle sympathetic nerve activity was enhanced during fatigue induced at 25% of maximal voluntary contraction of the forearm musculature. Jacobs and Segal [18] reported that post-contraction vasodilation was attenuated with muscle fatigue in the feed artery and proximal arterioles. Previous studies in animals demonstrated that functional sympatholysis is due mainly to blunting of postjunctional α2-adrenergic receptor-mediated vasoconstriction [3, 7, 24, 36]. From the results of these investigations, the increase of vasoconstriction with muscle fatigue observed in the present investigation might be caused by metabolites/ions, for example, potassium, the muscle release of which (and vascular and perivascular concentrations of) decrease with the decline of muscle force [8]. Together, these previous findings and the results of the present investigation suggest that the competing balances of local vasodilator responses and sympathetic vasoconstriction shift in favor of vasoconstriction with muscle fatigue. This compliments the observations made herein and supports the proposed mechanistic bases for increased respiratory muscle work and fatigue decreasing locomotory muscle blood flow and contractile performance [1, 10, 11, 15, 28, 31].
In summary, using a fatiguing stimulation protocol designed specifically to enhance sympathetically-mediated vasoconstrictor tone, we explored the temporal profile of the evoked vasoconstrictor responses, quantitatively assessed changes in sympatholysis, and determined the role of α-adrenergic receptor-mediated vasoconstriction on muscle performance. The principal findings were as follows: (1) fatiguing contractions induced by 4-ms pulses increased the vasoconstriction–vasodilation balance towards vasoconstriction; and (2) this vasoconstriction was largely ablated by the α1-adrenergic receptor antagonist (prazosin) or α2-adrenergic receptor antagonist (rauwolscine) and wholly ablated by combining α1- and α2-receptor antagonism. Muscle fatigue was significantly decreased concomitant with the increased arteriolar diameter and presumably enhanced blood flow during α-adrenergic inhibition. These results demonstrate that, in this preparation, as muscle fatigue becomes more pronounced there is a greater sympathetically-mediated vasoconstriction (i.e., partial attenuation of sympatholysis) relief of which can improve muscle performance, presumably, in part, through restoration of muscle blood flow.
References
Amann M, Regan MS, Kobitary M, Eldridge MW, Boutellier U, Pegelow DF, Dempsey JA (2010) Impact of pulmonary system limitations on locomotor muscle fatigue in patients with COPD. Am J Physiol Regul Integr Comp Physiol 299:R314–R324
Andersen P, Saltin B (1985) Maximal perfusion of skeletal muscle in man. J Physiol 366:233–249
Anderson KM, Faber JE (1991) Differential sensitivity of arteriolar alpha 1- and alpha 2-adrenoceptor constriction to metabolic inhibition during rat skeletal muscle contraction. Circ Res 69:174–184
Bailey JK, Kindig CA, Behnke BJ, Musch TI, Schmid-Schoenbein GW, Poole DC (2000) Spinotrapezius muscle microcirculatory function: effects of surgical exteriorization. Am J Physiol Heart Circ Physiol 279:H3131–H3137
Boegehold MA, Johnson PC (1988) Response of arteriolar network of skeletal muscle to sympathetic nerve stimulation. Am J Physiol 254:H919–H928
Buckwalter JB, Clifford PS (1999) alpha-adrenergic vasoconstriction in active skeletal muscles during dynamic exercise. Am J Physiol 277:H33–H39
Buckwalter JB, Naik JS, Valic Z, Clifford PS (2001) Exercise attenuates alpha-adrenergic-receptor responsiveness in skeletal muscle vasculature. J Appl Physiol 90:172–178
Burcher E, Garlick D (1973) Antagonism of vasoconstrictor responses by exercise in the gracilis muscle of the dog. J Pharmacol Exp Ther 187:78–85
Delp MD, Duan C (1996) Composition and size of type I, IIA, IID/X, and IIB fibers and citrate synthase activity of rat muscle. J Appl Physiol 80:261–270
Dempsey JA, McKenzie DC, Haverkamp HC, Eldridge MW (2008) Update in the understanding of respiratory limitations to exercise performance in fit, active adults. Chest 134:613–622
Dempsey JA, Romer L, Rodman J, Miller J, Smith C (2006) Consequences of exercise-induced respiratory muscle work. Respir Physiol Neurobiol 151:242–250
DiCarlo SE, Chen CY, Collins HL (1996) Onset of exercise increases lumbar sympathetic nerve activity in rats. Med Sci Sports Exerc 28:677–684
Faber JE (1988) In situ analysis of alpha-adrenoceptors on arteriolar and venular smooth muscle in rat skeletal muscle microcirculation. Circ Res 62:37–50
Hamann JJ, Buckwalter JB, Valic Z, Clifford PS (2002) Sympathetic restraint of muscle blood flow at the onset of dynamic exercise. J Appl Physiol 92:2452–2456
Harms CA, Wetter TJ, St. Croix CM, Pegelow DF, Dempsey JA (2000) Effects of respiratory muscle work on exercise performance. J Appl Physiol 89:131–138
Hill JM, Adreani CM, Kaufman MP (1996) Muscle reflex stimulates sympathetic postganglionic efferents innervating triceps surae muscles of cats. Am J Physiol 271:H38–H43
Honig CR, Frierson JL (1976) Neurons intrinsic to arterioles initiate postcontraction vasodilation. Am J Physiol 230:493–507
Jacobs TL, Segal SS (2000) Attenuation of vasodilatation with skeletal muscle fatigue in hamster retractor. J Physiol 524:929–941
Kindig CA, Musch TI, Basaraba RJ, Poole DC (1999) Impaired capillary hemodynamics in skeletal muscle of rats in chronic heart failure. J Appl Physiol 87:652–660
Kjellmer I (1964) The effect of exercise on the vascular bed of skeletal muscle. Acta Physiol Scand 62:18–30
Leek BT, Mudaliar SR, Henry R, Mathieu-Costello O, Richardson RS (2001) Effect of acute exercise on citrate synthase activity in untrained and trained human skeletal muscle. Am J Physiol Regul Integr Comp Physiol 280:R441–R447
Marshall JM (1982) The influence of the sympathetic nervous system on individual vessels of the microcirculation of skeletal muscle of the rat. J Physiol 332:169–186
Matsukawa K, Sadamoto T, Tsuchimochi H, Komine H, Murata J, Shimizu K (2001) Reflex responses in plasma catecholamines caused by static contraction of skeletal muscle. Jpn J Physiol 51:591–597
McGillivray-Anderson KM, Faber JE (1990) Effect of acidosis on contraction of microvascular smooth muscle by alpha 1- and alpha 2-adrenoceptors. Implications for neural and metabolic regulation. Circ Res 66:1643–1657
O’Leary DS, Robinson ED, Butler JL (1997) Is active skeletal muscle functionally vasoconstricted during dynamic exercise in conscious dogs? Am J Physiol 272:R386–R391
Ohyanagi M, Faber JE, Nishigaki K (1991) Differential activation of alpha 1- and alpha 2-adrenoceptors on microvascular smooth muscle during sympathetic nerve stimulation. Circ Res 68:232–244
Remensnyder JP, Mitchell JH, Sarnoff SJ (1962) Functional sympatholysis during muscular activity. Observations on influence of carotid sinus on oxygen uptake. Circ Res 11:370–380
Romer LM, Lovering AT, Haverkamp HC, Pegelow DF, Dempsey JA (2006) Effect of inspiratory muscle work on peripheral fatigue of locomotor muscles in healthy humans. J Physiol 571:425–439
Rowell LB, Saltin B, Kiens B, Christensen NJ (1986) Is peak quadriceps blood flow in humans even higher during exercise with hypoxemia? Am J Physiol 251:H1038–H1044
Saito M, Mano T, Iwase S (1989) Sympathetic nerve activity related to local fatigue sensation during static contraction. J Appl Physiol 67:980–984
Sheel AW, Derchak PA, Morgan BJ, Pegelow DF, Jacques AJ, Dempsey JA (2001) Fatiguing inspiratory muscle work causes reflex reduction in resting leg blood flow in humans. J Physiol 537:277–289
Sonobe T, Inagaki T, Poole DC, Kano Y (2008) Intracellular calcium accumulation following eccentric contractions in rat skeletal muscle in vivo: role of stretch-activated channels. Am J Physiol Regul Integr Comp Physiol 294:R1329–R1337
Suzuki H, Poole DC, Zweifach BW, Schmid-Schonbein GW (1995) Temporal correlation between maximum tetanic force and cell death in postischemic rat skeletal muscle. J Clin Invest 96:2892–2897
Tateishi J, Faber JE (1995) Inhibition of arteriole alpha 2- but not alpha 1-adrenoceptor constriction by acidosis and hypoxia in vitro. Am J Physiol 268:H2068–H2076
Thomas GD, Hansen J, Victor RG (1997) ATP-sensitive potassium channels mediate contraction-induced attenuation of sympathetic vasoconstriction in rat skeletal muscle. J Clin Invest 99:2602–2609
Thomas GD, Hansen J, Victor RG (1994) Inhibition of alpha 2-adrenergic vasoconstriction during contraction of glycolytic, not oxidative, rat hindlimb muscle. Am J Physiol 266:H920–H929
Thomas GD, Victor RG (1998) Nitric oxide mediates contraction-induced attenuation of sympathetic vasoconstriction in rat skeletal muscle. J Physiol 506:817–826
VanTeeffelen JW, Segal SS (2003) Interaction between sympathetic nerve activation and muscle fibre contraction in resistance vessels of hamster retractor muscle. J Physiol 550:563–574
Acknowledgments
This study is supported in part by Sasakawa Scientific Research Grant from the Japan Science Society and by Research Fellowships of the Japan Society for the Promotion of Science for Young Scientists.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Inagaki, T., Sonobe, T., Poole, D.C. et al. Progressive arteriolar vasoconstriction and fatigue during tetanic contractions of rat skeletal muscle are inhibited by α-receptor blockade. J Physiol Sci 61, 181–189 (2011). https://doi.org/10.1007/s12576-011-0134-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12576-011-0134-2