Abstract
Background
Right ventricular function and afterload are associated with clinical outcomes in pulmonary hypertension (PH). MRI-derived interventricular septal curvature has been associated with invasive hemodynamics in PH patients. This study sought to determine the relationship of echocardiography derived septal curvature with invasive hemodynamics in pediatric PH patients.
Methods
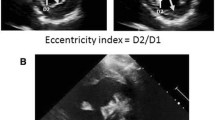
A single center chart review identified 56 pediatric patients with PH and 50 control patients with adequate echocardiography to assess septal curvature within one month of initial cardiac catheterization. Echocardiographic indices of septal flattening including end-systolic eccentricity index (EIs), maximum EI (EImax), minimum septal curvature (SCmin), and average SC (SCavg) were determined.
Results
PH patients had a median right ventricular systolic pressure of 64 mmHg (interquartile range (IQR) 48–81), mean pulmonary artery pressure of 44 mmHg (IQR 32–57), pulmonary vascular resistance of 7.9 iWU (IQR 4.8–12.9), and pulmonary capillary wedge pressure of 10 mmHg (IQR 8–12). Patients with PH had higher EIs and EImax and lower SCmin and SCavg compared to control patients. SCavg demonstrated the strongest association with right ventricular systolic pressure (R2 0.73, p < 0.0001), mean pulmonary artery pressure (R2 0.63, p < 0.0001), and pulmonary vascular resistance (R2 0.47, p < 0.0001). All septal curvature indices were associated with the composite adverse outcome, including Potts shunt, lung transplantation, and death. SCmin (HR 0.29; 95%CI 0.07–0.97) and SCavg (HR 0.15; 95%CI 0.03–0.72) were the only septal flattening indices associated with death.
Conclusions
Echocardiography derived septal curvature is a non-invasive marker of ventricular afterload and adverse outcomes.



Similar content being viewed by others
Abbreviations
- ALCAPA:
-
Anomalous left coronary artery arising from the pulmonary artery
- ASD:
-
Atrial septal defect
- CAO:
-
Composite adverse event
- CI:
-
Confidence interval
- EIs :
-
Eccentricity index at end systole
- EImax :
-
Maximum eccentricity index
- EIsc :
-
Eccentricity index at minimum septal curvature
- HR:
-
Hazard ratio
- IQR:
-
Interquartile range
- IVC:
-
Inferior vena cava
- mPAP:
-
Mean pulmonary artery pressure
- PAPVR:
-
Partial anomalous pulmonary venous return
- PAWP:
-
Pulmonary artery wedge pressure
- PH:
-
Pulmonary hypertension
- Qp:
-
Pulmonary blood flow
- Qp: Qs:
-
Ratio of pulmonary blood flow to cardiac index
- Qs:
-
Cardiac index
- ROC:
-
Receiver-operating characteristic
- Rp:
-
Pulmonary vascular resistance
- RVEDP:
-
Right ventricular end diastolic pressure
- RVSP:
-
Right ventricular systolic pressure
- SBP:
-
Systemic blood pressure
- SCavg :
-
Average septal curvature
- SCes :
-
Septal curvature at end systole
- SCmin :
-
Minimum septal curvature
- WHO:
-
World Health Organization
References
Rosenzweig EB, Abman SH, Adatia I, et al. Paediatric pulmonary arterial hypertension: updates on definition, classification, diagnostics and management. Eur Respir J. 2019;53(1).
Abman SH, Hansmann G, Archer SL, et al. Pediatric pulmonary hypertension: guidelines from the American heart association and American thoracic society. Circulation. 2015;132(21):2037–99.
del Cerro Marin MJ, Sabate Rotes A, Rodriguez Ogando A, et al. Assessing pulmonary hypertensive vascular disease in childhood. Data from the Spanish registry. Am J Respir Crit Care Med. 2014;190(12):1421–9.
van de Veerdonk MC, Kind T, Marcus JT, et al. Progressive right ventricular dysfunction in patients with pulmonary arterial hypertension responding to therapy. J Am Coll Cardiol. 2011;58(24):2511–9.
Moledina S, Pandya B, Bartsota M, et al. Prognostic significance of cardiac magnetic resonance imaging in children with pulmonary hypertension. Circ Cardiovasc Imaging. 2013;6(3):407–14.
Di Maria MV, Younoszai AK, Mertens L, et al. RV stroke work in children with pulmonary arterial hypertension: estimation based on invasive haemodynamic assessment and correlation with outcomes. Heart. 2014;100(17):1342–7.
Averin K, Michelfelder E, Sticka J, et al. Changes in ventricular geometry predict severity of right ventricular hypertension. Pediatr Cardiol. 2016;37(3):575–81.
Burkett DA, Patel SS, Mertens L, et al. Relationship between left ventricular geometry and invasive hemodynamics in pediatric pulmonary hypertension. Circ Cardiovasc Imaging. 2020;13(5): e009825.
Marcus JT, Gan CT, Zwanenburg JJ, et al. Interventricular mechanical asynchrony in pulmonary arterial hypertension: left-to-right delay in peak shortening is related to right ventricular overload and left ventricular underfilling. J Am Coll Cardiol. 2008;51(7):750–7.
Pandya B, Quail MA, Steeden JA, et al. Real-time magnetic resonance assessment of septal curvature accurately tracks acute hemodynamic changes in pediatric pulmonary hypertension. Circ Cardiovasc Imaging. 2014;7(4):706–13.
Bouchard A, Higgins CB, Byrd BF 3rd, et al. Magnetic resonance imaging in pulmonary arterial hypertension. Am J Cardiol. 1985;56(15):938–42.
Dellegrottaglie S, Sanz J, Poon M, et al. Pulmonary hypertension: accuracy of detection with left ventricular septal-to-free wall curvature ratio measured at cardiac MR. Radiology. 2007;243(1):63–9.
Roeleveld RJ, Marcus JT, Faes TJ, et al. Interventricular septal configuration at MR imaging and pulmonary arterial pressure in pulmonary hypertension. Radiology. 2005;234(3):710–7.
Sciancalepore MA, Maffessanti F, Patel AR, et al. Three-dimensional analysis of interventricular septal curvature from cardiac magnetic resonance images for the evaluation of patients with pulmonary hypertension. Int J Cardiovasc Imaging. 2012;28(5):1073–85.
Critser PJ, Higano NS, Lang SM, et al. Cardiovascular magnetic resonance imaging derived septal curvature in neonates with bronchopulmonary dysplasia associated pulmonary hypertension. J Cardiovasc Magn Reson. 2020;22(1):50.
King ME, Braun H, Goldblatt A, et al. Interventricular septal configuration as a predictor of right ventricular systolic hypertension in children: a cross-sectional echocardiographic study. Circulation. 1983;68(1):68–75.
Reisner SA, Azzam Z, Halmann M, et al. Septal/free wall curvature ratio: a noninvasive index of pulmonary arterial pressure. J Am Soc Echocardiogr. 1994;7(1):27–35.
Acknowledgements
None.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Paul Critser, Patrick Evers, and Kristin Schneider. The first draft of the manuscript was written by Paul Critser and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Paul Critser, Patrick Evers, Kristin Schneider, Russel Hirsch, Michael Taylor, Jason Woods, and Sean Lang declare that they have no conflict of interest.
Human right statement and informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1964 and later versions. The Institutional Review Board approved this study and waived the requirement for informed consent of this retrospective cohort study (study ID 2020-0391).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Critser, P.J., Evers, P.D., Schneider, K. et al. Echocardiography-derived septal curvature correlated with invasive hemodynamics in pediatric pulmonary hypertension. J Echocardiogr 20, 24–32 (2022). https://doi.org/10.1007/s12574-021-00545-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12574-021-00545-6