Abstract
The prognosis of patients with cancer has improved due to an early diagnosis of cancer and advances in cancer treatment. There are emerging reports on cardiotoxicity in cancer treatment and on cardiovascular disease in cancer patients, from which cardiovascular disease has been recognized as a common cause of death among cancer survivors. This situation has led to the need for a medical system in which oncologists and cardiologists work together to treat patients. With the growing importance of onco-cardiology, the role of echocardiography in cancer care is rapidly expanding, but at present, the practice of echocardiography in clinical settings varies from institution to institution, and is empirical with no established systematic guidance. In view of these circumstances, we thought that brief guidance for clinical application was necessary and have therefore developed this guidance, although evidence in this field is still insufficient.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Cancer therapeutics-related cardiac dysfunction: general
Background
The prognosis of patients with cancer has improved due to an early diagnosis of cancer and advances in cancer treatment, while the number of cancer patients tends to increase over time with the aging of society [1,2,3]. There are emerging reports on cardiotoxicity in cancer treatment and on cardiovascular diseases in cancer patients, from which cardiovascular disease has been recognized as a common cause of death among cancer survivors [4,5,6,7].
In the meantime, patients with heart failure are reported to have increased risk of cancer [8]. Indeed, cancer is the leading cause of death, and cardiovascular disease is the second leading cause of death in Japan, with increasing numbers of patients suffering from both conditions due to the aging of society and advances in cancer treatment. This situation has led to the need for a medical system in which oncologists and cardiologists work together to treat patients.
With the growing importance of onco-cardiology, the role of echocardiography in cancer care is rapidly expanding, but at present, the practice of echocardiography in clinical settings varies from institution to institution, and is empirical with no established systematic guidance. In view of these circumstances, we thought that brief guidance for clinical application was necessary and have, therefore, developed this guidance, although evidence in this field is still insufficient.
Definition of terms “cancer therapeutics-related cardiac dysfunction”
In general, cardiovascular complications of cancer therapy can be divided into the following nine categories [9]: (1) myocardial dysfunction and heart failure, (2) coronary artery disease, (3) valvular heart disease, (4) arrhythmias, especially those induced by QT-prolonging drugs, (5) arterial hypertension, (6) thromboembolic disease, (7) peripheral vascular disease and stroke, (8) pulmonary hypertension, and (9) pericardial complications.
Cancer therapeutics-related cardiac dysfunction refers primarily to (1) myocardial dysfunction and heart failure. This condition is typically abbreviated as “CTRCD,” but the definition of CTRCD is inconsistent and also may refer to ChemoTherapy-related Cardiac Dysfunction. Accordingly, to avoid confusion, the term “CTRCD” is not used in this guidance.
This guidance is primarily concerned with the clinical practice of echocardiography for chemotherapy-related cardiac dysfunction. Cancer treatment-related pulmonary hypertension, cancer-related thrombosis, and radiation-induced heart disease are also described briefly. The term “radiation-induced heart disease (RIHD)” is used distinctly from chemotherapy-related cardiac dysfunction.
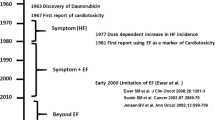
Classification of cancer therapeutics-related cardiac dysfunction (Table 1)
Anthracyclines directly induce myocardial damage and necrosis through oxidative stress and other mechanisms. Because of disability to repair or regenerate, cardiomyocytes are “irreversibly" injured, progressing to cardiotoxicity. Anthracycline-induced cardiotoxicity is dose dependent and even increases exponentially with dose [4].
In contrast, trastuzumab, an anti-HER2 antibody, can cause cardiomyocyte dysfunction but not necrosis, and its induced cardiotoxicity is reversible. Subsequently emerging tyrosine kinase inhibitors, such as sunitinib, imatinib, and sorafenib, which are also known as angiogenesis inhibitors because of their inhibitory action on vascular endothelial growth factor (VEGF) receptors, can cause reversible and dose-independent myocardial dysfunction but not necrosis [10].
Anthracycline-induced irreversible cardiac dysfunction is defined as Type I, while reversible cardiac dysfunction is defined as Type II [11]. However, about 20% of drugs classified as Type II may induce irreversible damage due to mechanisms overlapping with those of Type I drugs. In the actual treatment of cancer, many patients receive a combination of Types I and II drugs, with many cases of both types of cardiotoxicity.
Based on the concept that consequent cardiotoxicity and cardiac dysfunction are more important than the mechanisms by which drugs cause cardiotoxicity (irreversible or reversible, namely, Type I or II), the most recent American Society of Clinical Oncology (ASCO) guidelines do not adopt the terms Type I or II.
There are also emerging reports on the cardiotoxic effect of immune checkpoint inhibitors (ICIs), such as nivolumab [12].
Incidence and risk factors of cancer therapeutics-related cardiac dysfunction
In patients with cancer treated with regimens of trastuzumab alone or in combination with anthracyclines, the incidences of cardiotoxicity have been reported to be 4–27% for left ventricular (LV) dysfunction, and 0.4–16% for heart failure. A study of trastuzumab combined with an anthracycline showed an extremely high incidence rate of LV dysfunction (27%) and heart failure (16%) [13]. The other studies of combinations of trastuzumab and anthracyclines, in which the time difference between the start of chemotherapy and trastuzumab was 21–105 days, showed incidences of LV dysfunction of 4%–18.6%, and heart failure of 0.4–4% [4].
Although ICI-associated cardiac dysfunction is rare, with an incidence of approximately 1% [12, 14], deaths from fulminant myocarditis have been reported [10, 12, 15, 16]. ICI-related myocarditis occurred most frequently in the weeks after administration, but one case occurred as much as one year after administration. Risk factors for ICI-related myocarditis include combination ICI therapy, current or history of concurrent use of anticancer drugs with strong cardiotoxicity, such as VEGF inhibitors, ICI-related skeletal myositis, underlying cardiovascular disease with previous myocardial injury, underlying autoimmune disease, and antibodies to self cardiac antigens expressed in tumors. ICI-associated myocarditis is treated with high-dose steroids, although some cases are fatal.
Risk factors for cancer therapeutics-related cardiac dysfunction have been described in published guidelines and position papers in the cardiovascular and oncological fields [9, 17,18,19]. Table 2 summarizes the key risk factors from these references.
Prognosis and significance of early diagnosis of cancer therapeutics-related cardiac dysfunction
Anthracycline-related cardiotoxicity is classified into acute and chronic types according to the time of onset. Acute cardiotoxicity occurs shortly after drug administration, but it is very rare and usually reversible. Chronic cardiotoxicity is further divided into early-onset type, occurring within the first year of administration, and late-onset type, occurring several years after administration. Most studies of anthracycline-related cardiotoxicity were conducted retrospectively and showed highly inconsistent incidences and prognosis partly due to the widely varying definitions of cardiotoxicity and duration of follow-up [20]. Older studies reported that the 2-year survival rate was < 50% when anthracycline-related heart failure occurred [21, 22]. Felker et al. [23] reported that patients with cardiomyopathy due to doxorubicin had a poorer prognosis than those with idiopathic cardiomyopathy and ischemic heart disease. A prospective study of 2625 patients receiving anthracycline-containing regimen [24], reported in 2015, showed that anthracycline-induced cardiotoxicity (defined as a reduction in left ventricular ejection fraction [LVEF] of > 10 percentage points from baseline and LVEF of < 50%) occurred in 9% of the patients, with a median time to onset of 3.5 months (98% of cases occurred in the first year after the end of treatment). Of these, 71% had improved cardiac function, and 11% had full recovery by initiating cardioprotective agents soon after the detection of cardiac dysfunction. These results suggested that anthracycline induces cardiac myocyte death (which is irreversible) but the residual cardiac function can be ameliorated by early treatment with cardioprotective agents, such as angiotensin-converting inhibitors (ACE inhibitors)/angiotensin receptor blockers (ARBs) and β-blockers. In addition, current advances in nonpharmacological therapy for severe heart failure, such as cardiac resynchronization therapy, transcatheter mitral repair, and mechanical circulatory support, may further help to achieve better prognosis of anthracycline-induced cardiotoxicity than before.
Cardiotoxicity caused by trastuzumab, a molecular targeting agent, is generally considered reversible with a favorable prognosis. Although trastuzumab monotherapy rarely induces cardiac dysfunction, cancer therapeutics-related cardiac dysfunction occurs more frequently when trastuzumab is administered combined with anthracyclines, paclitaxel, or cyclophosphamide [25]. Echocardiography monitoring of LV systolic function is crucial because trastuzumab-induced-cardiac dysfunction responds well to drugs for heart failure, such as ACE inhibitors/ARBs and β-blockers, and trastuzumab can be resumed in many cases [26].
Diagnosis of cancer therapeutics-related cardiac dysfunction
Biomarkers
-
(i)
Implications for biomarker measurements
The required role of biomarkers in cancer therapeutics-related cardiac dysfunction is stratification of cardiac risks and early detection of cardiac dysfunction. So far, studies of biomarkers have focused mainly on troponins, B-type natriuretic peptide (BNP), and N-Terminal/Pro-B-Type natriuretic peptide (NT-proBNP). The results from prospective studies with adequate sample sizes are limited, and the appropriate timing and frequency, and the optimal cutoff values of biomarker measurements by cancer type and anticancer agent, remain insufficiently clear. Nevertheless, the European and American guidelines recommend biomarker measurements before, during and after cancer treatment (moderate recommendation) [18, 27].
The expert consensus of the European Association of Cardiovascular Imaging (EACVI) recommends troponin I (TnI) measurement in addition to echocardiographic indices [28]. Measuring BNP and Tn levels before starting treatment may be useful at least for risk assessment and evaluation of changes over time in cardiac function.
-
(ii)
Troponins
Cardiac troponin I (cTnI) and TnT (cTnT) are biomarkers specific to cardiac dysfunction, and, in particular, cTnI has been commonly used in studies of anthracycline-related cardiotoxicity. Recently, high-sensitivity troponin (hsTn) has been available, allowing the detection of trace levels of troponin. Cardinale et al. [29]. described the relationship between cTnI and high-dose chemotherapy for the first time in 2000. Their study included patients with a range of cancers (n = 204), including breast cancer, lymphomas, and ovarian cancer, who were receiving various chemotherapy regimens. TnI was measured before, immediately after, and 12, 24, 36, and 72 h after every single cycle of chemotherapy, while echocardiography was performed before the initiation and 1, 2, 3, 4, and 7 months after the end of chemotherapy. Patients in the positive TnI group showed a significantly more persistent reduction in LVEF. Cardinale et al. [30] also conducted a study of a larger number of cancer patients (n = 703), measured TnI soon after chemotherapy and 1 month later, and demonstrated that patients whose TnI tests were both positive had significantly reduced LVEF and more cardiovascular events. Furthermore, they conducted a study in patients with elevated TnI levels soon after receiving high-dose anthracycline-based chemotherapy (n = 114). The patients were randomized into the enalapril and control groups. The incidence of heart failure was significantly reduced in the enalapril group [31]. Another study group reported that the association between elevated Tn and cardiotoxicity was not significant. These conflicting results may be explained by differences in timing of Tn measurements and Tn assay methods and the small numbers of patients.
Trastuzumab, a molecular-targeting agent, is used in patients with HER2-positive breast and gastric cancer. There are limited reports on the implications of Tn measurements in trastuzumab-related cardiotoxicity. Sawaya et al. [32] demonstrated that a combination of elevated hsTnI and reduced global longitudinal strain (GLS) predicted subsequent cardiotoxicity in patients with breast cancer treated with anthracyclines, taxanes and trastuzumab (n = 81). Ky et al. [33] showed that early elevation of hsTnI levels (at 3 months) was associated with subsequent cardiac dysfunction in patients with breast cancer who received regimens similar to those used by Sawaya et al.
Cases of immune checkpoint inhibitor-related fulminant myocarditis have been reported, although they are rare. At present, the implications of monitoring Tn levels remain unclear in such cases.
-
(iii)
BNP/NT-proBNP
BNP/NT-proBNP is secreted in response to ventricular volume loading and wall stress. They are critical biomarkers in the assessment of heart failure in routine clinical practice. Among patients with active cancer who received high-dose chemotherapy (n = 52), those with persistently increased BNP/NT-proBNP levels had decreased LVEF 6–12 months after treatment [34]. Among cancer patients who received anthracyclines (n = 109), those who experienced cardiovascular events had a significantly higher BNP value before the cardiac event [35]. In contrast, BNP/NT-proBNP has not been demonstrated to predict the development of cardiotoxicity in patients with breast cancer [36]. Based on these findings, BNP/NT-proBNP is likely to be helpful for detecting cardiac dysfunction in the remote period after treatment, although it does not appear to be useful for early detection of cardiotoxicity. It should be noted that BNP/NT-proBNP is influenced by age, renal function, inflammation due to cancer, and the presence of arrhythmias, such as extrasystoles and atrial fibrillation.
Echocardiography
Echocardiography is the most commonly used diagnostic imaging tool for the assessment of cardiac function before, during and after cancer treatment because this procedure is non-invasive, can be performed repeatedly due to the absence of radiation exposure, and is widely available in current clinical settings. This modality is not only used to assess LV and RV sizes and cardiac function (contractility and distensibility), but also frequently used to diagnose ischemic heart disease, organic cardiovascular diseases, such as valvular disease, macrovascular disease, pericardial disease, cardiac tumors (primary and metastatic), and to assess the severity of these diseases [37]. Thus, echocardiography is widely useful not only for the diagnosis and management of cancer therapeutics-related cardiac dysfunction, but also for the diagnosis of cardiac abnormalities in the onco-cardiology field.
LV contractility
-
(a)
LVEF
LVEF is used in the definition of cancer therapeutics-related cardiac dysfunction, and requires accurate quantitative assessment.
-
(1)
Measurement method
The method of discs is recommended, whereby end-systolic and end-diastolic LV volumes are measured by tracing endocardial borders in apical four- and two-chamber views by two-dimensional echocardiography. However, LVEF determined by this method poses the issue that reproducibility is not always good. How to address this issue is discussed later (“Drug-induced pulmonary artery hypertension and cancer-associated thrombosis (CAT)” section).
The American Society of Echocardiography (ASE) and the European Society of Cardiovascular Imaging (EACVI) recommend determining LVEF by three-dimensional (3D) echocardiography [28]. Due to advances in ultrasound diagnostic machines and automated measurement techniques, 3D echocardiography allows us to obtain more accurate and reproducible LV volume measurements than those measured by the method of discs in patients with 3D images of good quality [38]. However, the 3D method has not achieved the recommended level for the assessment of cancer therapeutics-related cardiac dysfunction in routine clinical use for the following reasons: there are only a limited number of centers performing 3D echocardiography routinely, reliable measurements cannot be obtained in some patients due to image quality issues [39]; unlike the disk method, the normal value of LVEF by 3D echocardiography has not been widely published, and the cut-off value for cancer therapeutics-related cardiac dysfunction has not been well established [40].
Patients with cancer therapeutics-related cardiac dysfunction typically have diffuse LV wall motion abnormalities, but LV regional wall motion abnormalities may occur with certain anticancer drugs that increase the risk of developing ischemic heart disease [41]. Considering the fact that LV wall motion does not always impaired uniformly and that accurate quantification of LVEF is critical for the assessment of cancer therapeutics-related cardiac dysfunction, determination of LVEF by the eyeball method or the Teichholz method using M-mode echocardiography is inadequate.
-
(2)
Normal value
Based on the lower limit of normal for LVEF of 55% in the 2005 ASE guidelines for chamber quantification [42], LVEF of 55% had been used as the diagnostic criteria for cancer therapeutics-related cardiac dysfunction. The guidelines updated in 2015 provide the lower limit of normal for LVEF at 53%, taking into account the results of further studies [40]. Since the position paper of the European Society of Cardiology (ESC) defines cancer therapeutics-related cardiac dysfunction as “a decrease in LVEF of > 10 percentage points from baseline, to a value below the lower limit of normal” [9]. However, there is an issue of a measurement error in LVEF and normal value of LVEF may also change according to studies. Considering these matters, we set the cut-off value of LVEF at 50%. Therefore, a diagnosis of cancer therapeutics-related cardiac dysfunction is made when a patient has “a decrease in LVEF of > 10 percentage points from baseline, and to a value of < 50%.” (E.g., LVEF 57% → 46% meets the criteria, whereas LVEF 57% → 49% or LVEF 65% → 54% does not meet the criteria.) There is a possibility that the cut-off value may change by accumulation of evidence in Onco-Cardiology, thus a focused update should be implemented. In addition, it is important that we should do the close follow-up considering the time course of LVEF and clinical parameters, even if the value is not fulfilled the definition above.
-
(1)
-
(b)
Global longitudinal strain (GLS)
The method of discs has a measurement error of approximately 10% for LVEF [43, 44]. This value is equal to a diagnostic criterion (10% decrease from baseline) for cancer therapeutics-related cardiac dysfunction, which poses the significant issue that small changes in the LVEF value may not necessarily represent true changes due to reproducibility issues. Recently, GLS using speckle-tracking echocardiography has become utilized. GLS is a more sensitive and reproducible indicator of cardiac dysfunction than LVEF, and its use is recommended by the European and American cardiovascular guidelines [9, 28] and the American Society of Oncology guidelines.
In institutions where GLS measurements by speckle-tracking echocardiography are not feasible, mitral annular plane systolic excursion (MAPSE) calculated by M-mode echocardiography (a measure of left ventricular longitudinal function similar to GLS) or mitral annular systolic velocity (S’) by tissue pulsed Doppler echocardiography is recommended [28]. However, since, unlike GLS, the MAPSE and S’ do not have cut-off values for detecting the cardiotoxicity of anticancer drugs, interpretation of the results limited to that latent LV dysfunction is suspected if a significant decrease is noted compared with the previous or baseline value.
-
(1)
Measurement method
GLS is measured using two-dimensional speckle-tracking echocardiography on three apical views (long-axis and two- and four-chamber views) from video data of cardiac cycles, using analysis software built into the device or on a computer. GLS is defined as the average peak strain of 18 LV segments.
-
(2)
Normal value
Takigiku et al. have reported the normal range of LV GLS in Japanese subjects [45].
Table 3 summarizes the prediction of adverse cardiac events by GLS measurements before cancer treatment [46,47,48,49]. The cut-off values for GLS used in these studies ranged from 16 to 19%. Given that 18% is most commonly used as the lower limit of normal for GLS, a value of less than 16% is considered high risk, and 16–18% as borderline.
Negishi et al. [50] reported that 11% reduction in GLS over time predicted subsequent decrease in LVEF. In 2016 ESC Position paper [9], a relative percentage reduction of GLS of > 15% from baseline after cancer treatment (e.g., 25% → 21%, resulting in a relative percentage reduction of 16%, meets the criteria; but 25% → 22%, resulting in a relative percentage reduction 12%, does not meet the criteria) should be considered as a marker of early cardiotoxicity of anticancer drugs (i.e., subclinical LV cardiac dysfunction), even without a significant decrease in LVEF [9, 28]. On the other hand, relative percentage reductions of GLS of < 8% from baseline after cancer treatment appear not to be clinically meaningful (no cardiotoxicity of anticancer drugs or subclinical LV cardiac dysfunction) [28]. There are also ongoing clinical studies (e.g., SUCCOUR trial), and the cutoff values for these GLS may change in the future.
Table 4 shows the echocardiographic definitions of cancer therapeutics-related cardiac dysfunction in the relevant guidelines.
-
(1)
LV diastolic function
Data supporting the utility of LV diastolic function parameters for the diagnosis, follow-up, and prognostic prediction of cancer therapeutics-related cardiac dysfunction are sparse. Nevertheless, a routine systematic evaluation of LV diastolic function should be performed together with LV filling pressure according to the recommendations of the existing guidelines [51]. Caution should be exercised when E/e' is used to estimate the LV filling pressure, because the loading conditions are altered by the side effects (nausea, vomiting, diarrhea) of cancer treatment. Elevated LV filling pressure is suggestive of heart failure. Patients with such findings should be referred to a cardiologist even if they are asymptomatic.
Right ventricular (RV) function and pulmonary artery pressure
Data supporting the utility of RV function evaluation for the diagnosis of cancer therapeutics-related cardiac dysfunction are sparse. An assessment of RV contractility is critical when drugs with the risk of pulmonary arterial hypertension, including dasatinib and other tyrosine kinase inhibitors, are used, or when cancer-associated thrombosis is suspected. Echocardiography is also helpful in diagnosing a cancer-related disease called pulmonary tumor thrombotic microangiopathy (PTTM), which is characterized by a sudden elevation of pulmonary pressure.
Patients who have enlarged RV or decreased RV contractility, or those who are suspected of having pulmonary hypertension in the echocardiographic examination, should be referred to a cardiologist.
Other imaging modalities
-
(i)
Nuclear cardiology (myocardial scintigraphy)
ECG-gated pooled cardiac imaging enables the measurement of LVEF, in which technetium-99 m-labeled red blood cells in the heart chamber are counted using a γ camera to synchronize image acquisition with the heart rate. This technique allows the monitoring of cardiac function during chemotherapy, [52] and is indicated as class IA in the ACC/AHA guidelines [53]. Its utility in the early detection of cardiotoxicity has been demonstrated [54]. This method has good reproducibility and is helpful where LVEF cannot be assessed by echocardiography, but has the disadvantages of exposure to radiation and high cost.
-
(ii)
Cardiac MRI
Currently, cardiac MRI is regarded as the gold standard for measurement of the LV volume and LVEF, which provides the most accurate LV volume [55]. Cardiac MRI can also evaluate myocardial properties not possible by echocardiography. Cardiac MRI may be useful, specifically in those with suboptimal echocardiography or discrepant results. It is reported that delayed contrast enhancement is often distributed in the middle layer of the myocardium on the lateral wall in cardiomyopathy caused by trastuzumab [56]. A hyper-intense signal suggestive of potential cardiac dysfunction has been demonstrated by T1 mapping in some cancer survivors after anthracycline-based chemotherapy [57].
Cardiac MRI is safe, accurate, and reproducible with no radiation exposure, and is used for the diagnosis of cardiac involvement or metastasis of cancer, apart from cancer therapeutics-related cardiac dysfunction. However, this method has the disadvantages of being time-consuming and expensive, which limits the number of institutions that can implement it. Therefore, cardiac MRI should be considered when LVEF assessment by echocardiography is difficult.
Echocardiographic protocols for patients treated with anticancer drugs
Echocardiography before treatment with anticancer drugs (Tables 5, 6)
The purposes of echocardiographic examination prior to anticancer drug treatment are to assess cardiovascular risk, to predict possible cardiovascular complications, and to obtain control data for the early diagnosis of cardiovascular complications in the course of treatment. The examination should be conducted in all patients before initiating regimens containing drugs listed in Table 1 and immune checkpoint inhibitors.
An assessment of all routine echocardiographic parameters is mandatory. In particular, LVEF measurement is paramount, since this parameter is the basis of the definition of cancer therapeutics-related cardiac dysfunction. GLS is also recommended as a more sensitive indicator of left ventricular cardiac dysfunction, and GLS measurement is mandatory where feasible since this is recommended as a more sensitive parameter than LV cardiac dysfunction.
Echocardiography during treatment with anticancer drugs
-
(i)
Frequency of follow-up (Tables 5, 6; Fig. 1)
Anthracycline-related cardiac dysfunction is dose related. In other guidelines, [58] echocardiographic imaging is recommended in patients receiving anthracyclines at cumulative doses of > 240 mg/m2, and follow-up echocardiography should be repeated by accumulating additional doses. Regarding timing, it is recommended to perform echocardiography before each additional dose of 50 mg/m2, but in clinical practice, it is difficult to perform a follow-up examination at this frequency. Therefore, after consultation with physicians involved in cancer treatment, we have decided that echocardiography should be performed when the accumulated dose exceeds 500 mg/m2 in this guideline. Anthracycline-based anticancer regimens are listed by cancer type in Appendix Table 11, together with doses expressed as adriamycin equivalents. In some patients, it is difficult for cardiologists to know for certain the appropriate doses of anticancer drugs. In such cases, echocardiography may preferably be repeated about every 3 months during the follow-up period, and the frequency may be determined according to the circumstances and conditions of each institution. Most importantly, the required follow-up echocardiography should not be missed.
Cardiac dysfunction due to trastuzumab, an anti-HER2 monoclonal antibody, is not dose related. Follow-up evaluation every 3 months is desirable during treatment, as described in a Scientific Statement from American Heart Association [58]. Similar timing of follow-up evaluation is prescribed for novel anti-cancer drugs in their Guides for Proper Use. All of the recommended frequencies in these Guides for Proper Use have inadequate evidence, but are largely based on echocardiography schedules specified in the clinical study protocols of individual drugs. Therefore, it is not practical to perform echocardiography at every timing described in the Guides for Proper Use. In clinical practice use, echocardiographic evaluation should be considered as clinically indicated, for example, when clinical manifestations appear, or the cardiac shadow appears to enlarge on thorax XP or CT scans, compared with before treatment.
For a patient who meets the criteria for cancer therapeutics-related cardiac dysfunction for the first time, his/her oncologist and cardiologist should discuss whether or not to use cardioprotective drugs and whether or not to continue the anticancer drugs. Follow-up echocardiography should be conducted once within 2–3 weeks after meeting the criteria for the first time. After that, an echocardiographic examination should be conducted as appropriate, and a decision will be made as to whether to resume or discontinue the anti-cancer drugs after discussion between the oncologist and the cardiologist.
Follow-up intervals may be adjusted, taking into account the risk factors listed in Table 2.
Table 5 lists the recommended frequency of follow-up echocardiography, and Table 6 shows typical anticancer drugs.
-
(ii)
Evaluation parameters
The aim of the imaging examination during treatment is the early detection of cancer therapeutics-related cardiac dysfunction to initiate the administration of cardioprotective agents and adjustment of the anticancer regimen to allow cancer treatment to be completed as far as possible. As described in the previous section, it is challenging to repeat echocardiography as frequently as recommended in all cancer patients during treatment, partly due to limited laboratory human resources.
Therefore, mandatory items should be LV contractility, which is the basis of the definition of cancer therapeutics-related cardiac dysfunction, and other parameters that are helpful for the early detection of heart failure (Table 7) [28, 59, 60].
Comparison with previous or baseline values is essential for any parameters.
Echocardiography after treatment with anticancer drugs
-
1.
Frequency and duration of follow-up (Tables 5, 6, 8; Fig. 1)
Both pediatric and adult survivors of chemotherapy have a lifelong risk of development of cardiac dysfunction [9]. In particular, survivors treated with anthracyclines are more likely to develop cardiac dysfunction and require regular follow-up using echocardiography, biomarkers, and other measures. Since 98% of cases of anthracycline-induced cardiac dysfunction are reported to occur within the first year, with a mean time to development of 3.5 months, particularly close follow-up is necessary during the first 6 months of treatment [24].
Although there is no evidence on the time of completion of follow-up, patients who have received cardioprotective agents or whose regimen has been modified or altered during and after cancer treatment because of reduced cardiac function should be followed up on for life (preferably about once a year but it depends on the individual cardiac function and symptoms). Among cancer survivors who have no abnormal cardiac function during and 6 months after treatment, those who have received anthracyclines should be followed up on for up to 1 year after treatment, and their follow-up may be finished if no abnormal cardiac function occurs by that time; whereas for those who have never received anthracyclines, the follow-up can be finished if there are no abnormalities in the examination at the end of treatment. The intervals and duration of follow-up echocardiography are determined as appropriate by referring to Table 2 of risk factors.
-
(ii)
Evaluation parameters
Follow-up examinations after the end of treatment should include all parameters evaluated in routine echocardiography, as with the examination before treatment. The same is true for GLS measurements.
Drug-induced pulmonary artery hypertension and cancer-associated thrombosis (CAT)
Although this guidance is mainly intended to help the practice of echocardiography in the medical care of cancer therapeutics-related cardiac dysfunction, cancer treatment-related pulmonary hypertension, cancer-associated thrombosis, and radiation-induced heart disease are briefly described in “Drug-induced pulmonary artery hypertension and cancer-associated thrombosis (CAT)” and “Radiation-induced heart disease (RIHD)” sections.
Pulmonary hypertension
In the clinical classification of pulmonary hypertension, pulmonary hypertension induced by anticancer drugs is included in Group 1 as drug-induced pulmonary arterial hypertension (DPAH) [61]. Some alkylating agents (mitomycin C and cyclophosphamide) and interferon-α are traditionally considered possible risk factors of pulmonary hypertension. More recently, pulmonary hypertension has been reported in patients with chronic myeloid leukemia after treatment with dasatinib (tyrosine kinase inhibitor) [62, 63]. Dasatinib was considered a likely risk factor of pulmonary hypertension in the 2018 Nice Classification [64]. Of note, pulmonary hypertension due to chronic myeloid leukemia itself is classified as Group 5.
Thrombosis
In 1865, Trousseau described the association between migratory thrombophlebitis and occult malignancy for the first time, [65] and in 1936, Gross and Friedberg reported that patients with cancer were more likely to develop nonbacterial thromboendocarditis (NBTE) [66]. Systemic embolism induced by cancer-related hypercoagulability or NBTE in patients with cancer is called “Trousseau's syndrome,” for which special attention is needed because thrombosis can occur in both veins and arteries.
Cancer cells produce some factors that activate the coagulation pathway such as tissue factor. In addition, patients with cancer may develop blood flow stasis due to decreased physical activity or compression of vessels due to a tumor, and vascular endothelial injury can be induced by surgery and chemotherapy. Thus, cancer patients often suffer from Virchow’s triad (hypercoagulability, blood flow stasis, and vascular endothelial injury), which is a risk factor of thromboembolism. Thromboembolism is the second leading cause of death, following progression of cancer, in cancer patients treated with chemotherapy [67].
Among cancer-associated thrombosis, cerebral infarction is sometimes specifically called "Trousseau's syndrome" in a narrow sense. NBTE, one of the causes of cerebral infarction, develops most commonly in patients with adenocarcinomas, including lung, pancreatic and gastric cancer among the types of cancer. If patients with cancer develop cerebral infarction, echocardiography should be performed to evaluate for the presence of NBTE. Heparin, but not warfarin, is often helpful for the treatment of NBTE.
The incidence of venous thromboembolism (VTE) tends to increase year by year in cancer patients but not in non-cancer patients [68]. Cancer is a major risk factor for VTE, and patients with cancer account for 23–27% of patients with VTE [69, 70]. Among the types of cancer, the incidence of VTE is higher in gynecologic or hematopoietic malignancies relative to the prevalence of these malignancies [70]. Patients with cancer often suffer from recurrent VTE or major bleeding due to difficulties with anticoagulation control. VTE is also more likely to develop in patients with cancer during chemotherapy and those with distant metastases [70]. Therefore, patients with cancer should be treated with awareness of the high risk of VTE according to cancer sites and cancer status. Low-molecular-weight heparin (LMWH) is not used for the treatment of VTE in standard clinical practice in Japan because this indication is not covered by the National Health Insurance, while LMWH is the standard therapy for cancer-associated VTE in Europe and the U.S. Warfarin is often less controllable than LMWH. Emerging evidence that direct oral anticoagulants (DOACs) are noninferior to LMWH for the treatment of VTE [71, 72] has been spurring the use of DOACs for this condition.
Radiation-induced heart disease (RIHD)
Chest radiotherapy is used for the treatment of malignant lymphoma and breast, lung and esophageal cancer. It was once believed that radiation had minimal effect on the heart and blood vessels, but it is increasingly recognized that heart disease may develop as a late complication as long-term cancer survivors increase due to advances of cancer therapy. Radiation can cause pericarditis, cardiomyopathy, valvular disease, coronary artery disease, and carotid artery disease, depending on the area irradiated, with incidences of 10–30% in patients at 5–10 years after radiotherapy. RIHD, a heterogeneous disease that can manifest years or decades, is associated with high morbidity and mortality [73]. Patients with risk factors for RIHD, including younger age, high radiation doses, and use of anthracyclines (Table 9), require special caution [74].
Common types of RIHD
-
(i)
Pericardial disease
Acute pericarditis is an early complication of radiotherapy. Its incidence has decreased by modern radiotherapy techniques, such as reduction in dose and field size [75]. Delayed pericarditis may manifest several weeks to years after radiotherapy, with pericardial fibrous thickening and adhesions, chronic constriction, and chronic pericardial effusion, progressing to constrictive pericarditis. Constrictive pericarditis can be observed in about 4–20% of patients, and its incidence increases with increasing radiation dose [74].
-
(ii)
Cardiomyopathy
Cardiomyocytes themselves are resistant to radiation because they do not undergo cell division, but the vascular endothelial injury can be induced by radiation. The resulting microvascular damage can cause ischemia and eventually myocardial dysfunction. Myocardial compliance decreases as myocardial fibrosis progresses, possibly leading mainly to diastolic dysfunction, although systolic dysfunction also may occur. Conduction disturbance may occur. Incidence of cardiomyopathy is reported about 10% [76]. In patients with Hodgkin lymphoma treated with non-anthracycline-based regimens, the 25-year cumulative risks of heart failure after radiotherapy were 4.4%, 6.2%, and 13.3% with 0–15 Gy, 16–20 Gy, and ≥ 21 Gy, respectively, appearing to be dose dependent [77].
-
(iii)
Valvular heart disease
Radiotherapy can cause thickening, fibrosis, shortening, and calcification of the leaflets and perivalvular tissues. These findings are more predominant in the left-sided than the right-sided valves and are probably related to pressure overload. Radiation-induced valvular disease can be differentiated from rheumatic valve disease by the lesser degree of degeneration of the leaflet tips and commissures and the presence of calcification of the ascending aorta and annulus. Aortomitral curtain thickening/calcification is a hallmark of previous heart irradiation and its extent is associated with mortality [78]. Valvular regurgitation is more commonly encountered than valvular stenosis because of shortening of the valve. Stenotic lesions more often involve the aortic valve. The reported incidence of clinically significant valvular disease is about 1% at 10 years, 5% at 15 years, and 6% at 20 years after radiation exposure. The incidence at 20 years after radiotherapy of mild aortic regurgitation is about 45%, moderate or severe aortic regurgitation about 15%, aortic stenosis about 16%, mild mitral regurgitation about 48%, and mild pulmonary regurgitation about 12% [74]. If surgery is considered in patients with severe valvular disease, transcatheter aortic valve implantation (TAVI) may be preferred for aortic stenosis due to the high risks associated with open heart surgery, such as mediastinal adhesions, high risk pulmonary findings, or calcification of the ascending aorta [73], 79
-
(iv)
Coronary artery disease
Radiation-induced coronary artery disease develops due to arteriosclerosis accelerated by vascular endothelial injury. It manifests 15–20 years after radiotherapy and is more likely to occur in younger patients [80]. Coronary artery disease is reported to occur in 10% of patients with Hodgkin lymphoma at 20 years after radiation [81].
Concomitant atherosclerotic risk factors further enhance the development of the disease. In patients with left-sided breast cancer, who undergo left-side chest irradiation, the left coronary main trunk and proximal segments are typically involved [74]. Open heart surgery is high risk, and catheterization for radiation-induced coronary artery stenosis is associated with more restenosis than typical atherosclerotic lesions. Therefore, careful consideration is required for treatment indications.
-
(v)
Carotid artery disease
As with coronary artery disease, vascular endothelial injury can be induced in vessels within the radiation field, accelerating the progression of arteriosclerosis. Radiotherapy-induced lesions are more extensive, involving atypical areas of carotid segments [74]. A total of 7% of survivors of Hodgkin lymphoma treated with radiation therapy developed carotid and/or subclavian artery disease 20 years after radiotherapy [81]. The relative risk of stroke was 5.6 in patients with head and neck tumors treated with radiotherapy [82]. Therefore, patients receiving radiation to the head and neck require a follow-up for carotid artery disease.
Follow-up after radiotherapy (Fig. 2)
It is not necessary to perform echocardiography routinely before and during radiotherapy.
As described above, since radiation-induced cardiac damage often becomes overt after several years or even more than a decade after radiation, it is important to perform regular physical examination and risk factor assessment. For patients at high risk, evaluation focusing on coronary lesions should be initiated around 5 years after radiotherapy. Valvular disease becomes apparent later than coronary arterial disease and requires long-term echocardiographic follow-up.
Although regular follow-up is desirable after radiotherapy, there is a lack of evidence regarding its frequency and evaluation parameters, and further accumulation of new findings is awaited.
Considerations in practical application
Echocardiographic parameters and measurement errors
Although the development of various automatic measurement techniques has been advancing, the majority of echocardiographic measurements rely on manual measurement and tracing, and the measurement accuracy of parameters depends, to a varying degree, on the examiner's experience and skills. Since the measurement accuracy also depends on the image quality, the reproducibility decreases in cases where images of optimal quality cannot be obtained. The apical approach is difficult in some patients, particularly in those who have undergone left-sided mastectomy. Of note, the reproducibility study of LVEF measurements reported intra- and inter-examiner variability of approximately 5–10%.[83, 84]. GLS measurements also have intra- and inter-examiner variability of approximately 5% [85]. Most of these data were obtained from center hospitals where examiners have adequate echocardiographic experiences and skills. The same reproducibility may not be ensured in community hospitals and clinics. Changes in LVEF and GLS measurements are key factors in making a treatment decision for patients with cancer. Here, we describe quality control and reports of measurements that physicians and sonographers performing echocardiography should be aware of providing safe and appropriate chemotherapy to patients with cancer.
Quality control in the echocardiography laboratory (Table 10)
First, in order for the echocardiographic machines to properly work and perform measurement, it is necessary to carry out maintenance and inspection of the echocardiography laboratory and equipment in accordance with the relevant guideline [86]. To ensure the accuracy of echocardiographic measurements, it is recommended to verify intra- and inter-examiner variability for LVEF and GLS measurements at least once a year to ensure quality control in the laboratory. Above all, the education of the staff who perform echocardiography is of utmost importance for quality control of echocardiographic measurements. Well-experienced staff, such as an sonographer certified by the Japanese Society of Echocardiography and an echocardiologist, should educate inexperienced staff to perform echocardiography uniformly with good accuracy. In addition, equipment should be adequately maintained to ensure that the still images and videos of echocardiography are stored in the storage server and are accessible at any time for reference or re-measurement as needed.
Considerations for echocardiographic measurements (Table 10)
To make an appropriate treatment decision, it is necessary to minimize the measurement errors of echocardiographic parameters as much as possible. To provide proper measurements, echocardiography should be performed with the following considerations:
-
(a) Review of previous and baseline measurements
In patients who have previously undergone echocardiography, the previous and baseline measurements and images should be reviewed prior to echocardiography (Class I). For this reason, baseline still and motion images should always be recorded. If a well-experienced examiner considers that the previous measurements are not valid compared to the image, they should be re-measured and the examiner should contact the attending physician.
-
(b) Measurements by the same examiner
If possible, the same examiner should be responsible for repeated examinations of the same patient. This does not apply if it is impracticable due to personnel allocation.
-
(c) Measurements with the same echocardiographic machine
Inter-vendor variability of echocardiographic measurements has been reported, particularly for GLS measurements. Standardization has been advanced by a task force led by ASE and EACVI, [85] which has reduced the inter-vendor variability of echocardiographic measurements [87]. However, it is desirable that echocardiographic machines from the same manufacturer be used for the same patient as far as possible. However, this does not apply if it is difficult from the viewpoint of resources for each laboratory.
-
(d) Validation of measurements
Echocardiographic measurements should be assessed by a well-experienced examiner to ensure agreement with visual assessment (Class I). If possible, apart from the examiner, an echocardiologist or certified sonographer should examine the validity of the measurements. In patients who have previously undergone echocardiography, changes in echocardiographic measurements should be examined to ensure agreement with visual changes on the image.
For deciding appropriate treatment
If there are significant changes in echocardiographic measurements that may lead alterations in chemotherapy, or if there is any doubt about the accuracy of the measurements, the validity of the measurements should be examined by an echocardiologist or certified sonographer as appropriate. If their validity is doubtful, re-measurement or evaluation using other modalities should be performed.
Future directions
Advances in echocardiography have allowed the automatic analysis of various parameters, and it is expected that the reproducibility will be improved by using automated measurement. It was recently reported that the use of artificial intelligence (AI) improves the accuracy of echocardiographic measurements [88]. In the future, with the use of such technologies, echocardiographic measurements are expected to be performed with good accuracy and excellent reproducibility even by inexperienced examiners.
References
Ferlay J, Steliarova-Foucher E, Lortet-Tieulent J, et al. Cancer incidence and mortality patterns in Europe: estimates for 40 countries in 2012. Eur J Cancer. 2013;49:1374–403.
Mariotto AB, Yabroff KR, Shao Y, et al. Projections of the cost of cancer care in the United States: 2010–2020. J Natl Cancer Inst. 2011;103:117–28.
Miller KD, Siegel RL, Lin CC, et al. Cancer treatment and survivorship statistics, 2016. CA Cancer J Clin. 2016;66:271–89.
Ewer MS, Ewer SM. Cardiotoxicity of anticancer treatments. Nat Rev Cardiol. 2015;12:620.
Armstrong GT, Oeffinger KC, Chen Y, et al. Modifiable risk factors and major cardiac events among adult survivors of childhood cancer. J Clin Oncol. 2013;31:3673–80.
Patnaik JL, Byers T, DiGuiseppi C, et al. Cardiovascular disease competes with breast cancer as the leading cause of death for older females diagnosed with breast cancer: a retrospective cohort study. Breast Cancer Res. 2011;13:R64.
Koene RJ, Prizment AE, Blaes A, et al. Shared risk factors in cardiovascular disease and cancer. Circulation. 2016;133:1104–14.
Hasin T, Gerber Y, McNallan SM, et al. Patients with heart failure have an increased risk of incident cancer. J Am Coll Cardiol. 2013;62:881–6.
Zamorano JL, Lancellotti P, Rodriguez Munoz D, et al. 2016 ESC Position Paper on cancer treatments and cardiovascular toxicity developed under the auspices of the ESC Committee for Practice Guidelines: The Task Force for cancer treatments and cardiovascular toxicity of the European Society of Cardiology (ESC). Eur Heart J. 2016;37:2768–801.
Johnson DB, Balko JM, Compton ML, et al. Fulminant myocarditis with combination immune checkpoint blockade. N Engl J Med. 2016;375:1749–55.
Ewer MS, Lippman SM. Type II chemotherapy-related cardiac dysfunction: time to recognize a new entity. J Clin Oncol. 2005;23:2900–2.
Lyon AR, Yousaf N, Battisti NML, et al. Immune checkpoint inhibitors and cardiovascular toxicity. Lancet Oncol. 2018;19:e447–58.
Slamon DJ, Leyland-Jones B, Shak S, et al. Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. N Engl J Med. 2001;344:783–92.
Manouchehri A, Moey M, et al. Cardiovascular toxicities associated with immune checkpoint inhibitors: an observational, retrospective, pharmacovigilance study. Lancet Oncol. 2018;19:1579–89.
Matsuo K, Ishiguro T, Najama T, et al. Nivolumab-induced myocarditis successfully treated with corticosteroid therapy: a case report and review of the literature. Intern Med. 2019;58:2367–72.
Tajiri K, Aonuma K, Sekine I. Immune checkpoint inhibitor-related myocarditis. Jpn J Clin Oncol. 2018;48:7–12.
Virizuela JA, García AM, de Las PR, et al. SEOM clinical guideline on cardiovascular toxicity 2018. Clin Transl Oncol. 2019;21:94–105.
Armenian SH, Lacchetti C, Barac A, et al. Prevention and monitoring of cardiac dysfunction in survivors of adult cancers: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol. 2017;35:893–911.
Herrmann J, Lerman A, Sandhu NP, et al. Evaluation and management of patients with heart disease and cancer: cardio-oncology. Mayo Clin Proc. 2014;89:1287–306.
Yeh ET, Bickford CL. Cardiovascular complications of cancer therapy: incidence, pathogenesis, diagnosis, and management. J Am Coll Cardiol. 2009;53:2231–47.
Haq MM, Legha SS, Choksi J, et al. Doxorubicin-induced congestive heart failure in adults. Cancer. 1985;56:1361–5.
Ryberg M, Nielsen D, Skovsgaard T, et al. Epirubicin cardiotoxicity: an analysis of 469 patients with metastatic breast cancer. J Clin Oncol. 1998;16:3502–8.
Felker GM, Thompson RE, Hare JM, et al. Underlying causes and long-term survival in patients with initially unexplained cardiomyopathy. N Engl J Med. 2000;342:1077–84.
Cardinale D, Colombo A, Bacchiani G, et al. Early detection of anthracycline cardiotoxicity and improvement with heart failure therapy. Circulation. 2015;131:1981–8.
Guarneri V, Lenihan DJ, Valero V, et al. Long-term cardiac tolerability of trastuzumab in metastatic breast cancer: the M.D. Anderson Cancer Center experience. J Clin Oncol. 2006;24:4107–15.
Ewer MS, Vooletich MT, Durand JB, et al. Reversibility of trastuzumab-related cardiotoxicity: new insights based on clinical course and response to medical treatment. J Clin Oncol. 2005;23:7820–6.
Curigliano G, Cardinale D, Suter T, et al. Management of cardiac disease in cancer patients throughout oncological treatment: ESMO consensus recommendations. Ann Oncol. 2020;31(2):171–90.
Plana JC, Galderisi M, Barac A, et al. Expert consensus for multimodality imaging evaluation of adult patients during and after cancer therapy: a report from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2014;27:911–39.
Cardinale D, Sandri MT, Martinoni A, et al. Left ventricular dysfunction predicted by early troponin I release after high-dose chemotherapy. J Am Coll Cardiol. 2000;36:517–22.
Cardinale D, Sandri MT, Colombo A, et al. Prognostic value of troponin I in cardiac risk stratification of cancer patients undergoing high-dose chemotherapy. Circulation. 2004;109:2749–54.
Cardinale D, Colombo A, Sandri MT, et al. Prevention of high-dose chemotherapy-induced cardiotoxicity in high-risk patients by angiotensin-converting enzyme inhibition. Circulation. 2006;114:2474–81.
Sawaya H, Sebag IA, Plana JC, et al. Assessment of echocardiography and biomarkers for the extended prediction of cardiotoxicity in patients treated with anthracyclines, taxanes and trastuzumab. Circ Cardiovasc Imaging. 2012;5:596–603.
Ky B, Putt M, Sawaya H, et al. Early increases in multiple biomarkers predict subsequent cardiotoxicity in patients with breast cancer treated with doxorubicin, taxanes and trastuzumab. J Am Coll Cardiol. 2014;63:809–16.
Sandri MT, Salvatici M, Cardinale D, et al. N-terminal pro-B-type natriuretic peptide after high-dose chemotherapy: a marker predictive of cardiac dysfunction? Clin Chem. 2005;51:1405–10.
Lenihan DJ, Stevens PL, Massey M, et al. The utility of point-of-care biomarkers to detect cardiotoxicity during anthracycline chemotherapy: a feasibility study. J Cardiac Fail. 2016;22:433–8.
Sawaya H, Sebag IA, Plana JC, et al. Early detection and prediction of cardiotoxicity in chemotherapy-treated patients. Am J Cardiol. 2011;107:1375–80.
Daher IN, Kim C, Saleh RR, et al. Prevalence of abnormal echocardiographic findings in cancer patients: a retrospective evaluation of echocardiography for identifying cardiac abnormalities in cancer patients. Echocardiography. 2011;28:1061–7.
Wood Peter W, Choy JB, Nanda NC, et al. Left ventricular ejection fraction and volumes: it depends on the imaging method. Echocardiography. 2014;31:87–100.
Medvedofsky D, Mor-Avi V, Byku I, et al. Three-dimensional echocardiographic automated quantification of left heart chamber volumes using an adaptive analytics algorithm: Feasibility and impact of image quality in nonselected patients. J Am Soc Echocardiogr. 2017;30:879–85.
Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015;28(1–39):e14.
Isner JM, Ferrans VJ, Cohen SR, et al. Clinical and morphologic cardiac findings after anthracycline chemotherapy. Analysis of 64 patients studied at necropsy. Am J Cardiol. 1983;51:1167–74.
Lang RM, Bierig M, Devereux RB, et al. Chamber Quantification Writing Group, American Society of Echocardiography’s Guidelines, Standards Committee, European Association of Echocardiography. Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005;18:1440–63.
Thavendiranathan P, Grant AD, Negishi T, et al. Reproducibility of echocardiographic techniques for sequential assessment of left ventricular ejection fraction and volumes: application to patients undergoing cancer chemotherapy. J Am Coll Cardiol. 2013;61:77–84.
Otterstad JE, Froeland G, St. John Sutton M, et al. Accuracy and reproducibility of biplane two-dimensional echocardiographic measurements of left ventricular dimensions and function. Europ Heart J. 1997;18:507–13.
Takigiku K, Takeuchi M, Izumi C, et al. Normal range of left ventricular 2-dimensional strain: Japanese ultrasound speckle tracking of the left ventricle (justice) study. Circ J. 2012;76:2623–32.
Mousavi N, Tan TC, Ali M, et al. Echocardiographic parameters of left ventricular size and function as predictors of symptomatic heart failure in patients with a left ventricular ejection fraction of 50–59% treated with anthracyclines. Eur Heart J Cardiovasc Imaging. 2015;16:977–84.
Rhea IB, Uppuluri S, Sawada S, et al. Incremental prognostic value of echocardiographic strain and its association with mortality in cancer patients. J Am Soc Echocardiogr. 2015;28:667–73.
Ali MT, Yucel E, Bouras S, et al. Myocardial strain is associated with adverse clinical cardiac events in patients treated with anthracyclines. J Am Soc Echocardiogr. 2016;29(522–527):e523.
Hatazawa K, Tanaka H, Nonaka A, et al. Baseline global longitudinal strain as a predictor of left ventricular dysfunction and hospitalization for heart failure of patients with malignant lymphoma after anthracycline therapy. Circ J. 2018;82:2566–74.
Negishi K, Negishi T, Hare JL, et al. Independent and incremental value of deformation indices for prediction of trastuzumab-induced cardiotoxicity. J Am Soc Echocardiogr. 2013;26:493–8.
Nagueh SF, Smiseth OA, Appleton CP, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2016;29:277–314.
Choi BW, Berger HJ, Schwartz PE, et al. Serial radionuclide assessment of doxorubicin cardiotoxicity in cancer patients with abnormal baseline resting left ventricular performance. Am Heart J. 1983;106:638–43.
Hendel RC, Berman DS, Di Carli MF, et al. A. Accf/asnc/acr/aha/ase/scct/scmr/snm 2009 Appropriate use criteria for cardiac radionuclide imaging: a report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, the American Society of Nuclear Cardiology, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the Society of Cardiovascular Computed Tomography, the Society for Cardiovascular Magnetic Resonance, and the Society of Nuclear Medicine. Circulation. 2009;119:e561-587.
Nousiainen T, Jantunen E, Vanninen E, et al. Early decline in left ventricular ejection fraction predicts doxorubicin cardiotoxicity in lymphoma patients. Br J Cancer. 2002;86:1697–700.
Sechtem U, Neubauer S, Revel D, et al. The clinical role of magnetic resonance in cardiovascular disease. Task force of the European Society of Cardiology, in collaboration with the Association of European Paediatric Cardiologists. Eur Heart J. 1998;19:19–39.
Machann W, Beer M, Breunig M, et al. Cardiac magnetic resonance imaging findings in 20-year survivors of mediastinal radiotherapy for Hodgkin’s disease. Int J Radiat Oncol Biol Phys. 2011;79:1117–23.
Jordan JH, Vasu S, Morgan TM, et al. Anthracycline-associated t1 mapping characteristics are elevated independent of the presence of cardiovascular comorbidities in cancer survivors. Circ Cardiovasc Imaging. 2016;9:e004325.
Mehta LS. Cardiovascular disease and breast cancer: where these entities intersect: a scientific statement from the American Heart Association. Circulation. 2018;137:e30–66.
Stoddard MF, Seeger J, Liddell NE, et al. Prolongation of isovolumetric relaxation time as assessed by Doppler echocardiography predicts doxorubicin-induced systolic dysfunction in humans. J Am Coll Cardiol. 1992;20:62–9.
Dorup I, Levitt G, Sullivan I, et al. Prospective longitudinal assessment of late anthracycline cardiotoxicity after childhood cancer: the role of diastolic function. Heart. 2004;90:1214–6.
Galie N, Humbert M, Vachiery JL, et al. 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: the Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur Heart J. 2016;37:67–119.
Montani D, Bergot E, Gunther S, et al. Pulmonary arterial hypertension in patients treated by dasatinib. Circulation. 2012;125:2128–37.
Rasheed W, Flaim B, Seymour JF. Reversible severe pulmonary hypertension secondary to dasatinib in a patient with chronic myeloid leukemia. Leuk Res. 2009;33:861–4.
Simonneau G, Gatzoulis MA, Adatia I, et al. Updated clinical classification of pulmonary hypertension. J Am Coll Cardiol. 2013;62:D34-41.
Trousseau A. Phlegmasia alba dolens. Lectures on clinical medicine, delivered at the Hotel-Dieu, Paris. 1865;5:281–332.
Gross L, Friedberg CK. Nonbacterial thrombotic endocarditis. Classification and general description. Arch Intern Med. 1936;58:620–40.
Khorana AA. Venous thromboembolism and prognosis in cancer. Thromb Res. 2010;125(6):490–3.
Timp JF, Braekkan SK, Versteeg HH, et al. Epidemiology of cancer-associated venous thrombosis. Blood. 2013;122(10):1712–23.
Nakamura M, Miyata T, Ozeki Y, et al. Current venous thromboembolism management and outcomes in Japan. Circ J. 2014;78(3):708–17.
Sakamoto J, Yamashita Y, Morimoto T, et al. Cancer-associated venous thromboembolism in the real world—from the COMMAND VTE registry. Circ J. 2019;83(11):2271–81.
Raskob GE, van Es N, Verhamme P, et al. Edoxaban for the treatment of cancer-associated venous thromboembolism. N Engl J Med. 2018;378(7):615–24.
Young AM, Marshall A, Thirlwall J, et al. Comparison of an oral factor Xa inhibitor with low molecular weight heparin in patients with cancer with venous thromboembolism: results of a randomized trial (SELECT-D). J Clin Oncol. 2018;36(20):2017–23.
Desai MY, Windecker S, Lancellotti P, et al. Prevention, diagnosis, and management of radiation associated cardiac disease: JACC scientific expert panel. J Am Coll Cardiol. 2019;74:905–27.
Lancellotti P, Nkomo VT, Badano LP, et al. Expert consensus for multi-modality imaging evaluation of cardiovascular complications of radiotherapy in adults: a report from the European Association of Cardiovascular Imaging and the American Society of Echocardiography. Eur Heart J Cardiovasc Imaging. 2013;14(8):721–40.
Jaworski C, Mariani JA, Wheeler G, et al. Cardiac complications of thoracic irradiation. J Am Coll Cardiol. 2013;61(23):2319–28.
Chang HM, Okwuosa TM, Scarabelli T, et al. Cardiovascular complications of cancer therapy: best practices in diagnosis, prevention, and management: Part 2. J Am Coll Cardiol. 2017;70(20):2552–65.
van Nimwegen FA, Ntentas G, Darby SC, et al. Risk of heart failure in survivors of Hodgkin lymphoma: effects of cardiac exposure to radiation and anthracyclines. Blood. 2017;129(16):2257–65.
Desai MY, Wu W, Masri A, et al. Increased aorto-mitral curtain thickness independently predicts mortality in patients with radiation-associated cardiac disease undergoing cardiac surgery. Ann Thorac Surg. 2014;97:1348–55.
Donnellan E, Phelan D, McCarthy CP, et al. Radiation-induced heart disease: A practical guide to diagnosis and management. Cleve Clin J Med. 2016;83(12):914–22.
van Nimwegen FA, Schaapveld M, Cutter DJ, et al. Radiation dose-response relationship for risk of coronary heart disease in survivors of Hodgkin lymphoma. J Clin Oncol. 2016;34(3):235–43.
Hull MC, Morris CG, Pepine CJ, et al. Valvular dysfunction and carotid, subclavian, and coronary artery disease in survivors of Hodgkin lymphoma treated with radiation therapy. JAMA. 2003;290(21):2831–7.
Gujral DM, Chahal N, Senior R, et al. Radiation-induced carotid artery atherosclerosis. Radiother Oncol. 2014;110(1):31–8.
Grothues F, Smith GC, Moon JCC, et al. Comparison of interstudy reproducibility of cardiovascular magnetic resonance with two-dimensional echocardiography in normal subjects and in patients with heart failure or left ventricular hypertrophy. Am J Cardiol. 2002;90:29–34.
Malm S, Frigstad S, Sagberg E, et al. Real-time simultaneous triplane contrast echocardiography gives rapid, accurate, and reproducible assessment of left ventricular volumes and ejection fraction: a comparison with magnetic resonance imaging. J Am Soc Echocardiogr. 2006;19:1494–501.
Cheng S, Larson MG, McCabe EL, et al. Reproducibility of speckle-tracking-based strain measures of left ventricular function in a community-based study. J Am Soc Echocardiogr. 2013;26:1258–66.
Daimon M, Akaishi M, Asanuma T, et al. Guideline from Japanese Society of Echocardiography: 2018 focused update incorporated into Guidance for the Management and Maintenance of Echocardiography Equipment. Springer Japan. 2018:1–5. https://doi.org/10.1007/s12574-018-0370-z. Accessed 15 June 2018.
Farsalinos KE, Daraban AM, Unlu S, et al. Head-to-head comparison of global longitudinal strain measurements among nine different vendors: the eacvi/ase inter-vendor comparison study. J Am Soc Echocardiogr. 2015;28(1171–1181):e1172.
Kusunose K, Haga A, Abe T, et al. Utilization of artificial intelligence in echocardiography. Circ J. 2019;83:1623–9.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
Tetsuari Onishi has received speaker honoraria from Bayer, Medtronic, General Electric, Otsuka, Bristol-Myers, Daiichi Sankyo, and Abbott. Yoko Fukuda has received a speaker honorarium from Philips. Hirotsugu Yamada has received a manuscript fee from US-lead, and has received speaker honoraria from Daiichi-Sankyo, Bayer, Ono, Otsuka, Cannon, and Hitachi. Hidekazu Tanaka has received research grants from Novartis and has received speaker honoraria from Boehringer Ingelheim, Sumitomo Dainippon Pharma, AstraZeneca, Mitsubishi Tanabe, Taisho Pharma, TOA EIYO, Bayer, Ono, General Electric, Daiichi Sankyo, Novartis, Teijin, Merck, Sekisui Medical, and Philips. Jiro Sakamoto has received speaker honoraria from Bayer, Bristol-Myers, Daiichi Sankyo, and Pfizer. Masao Daimon has received speaker honoraria from Janssen, Cannon, Philips, and General Electronics. Akiko Nonaka has received speaker honoraria from Bristol-Myers, Bayer, Daiichi-Sankyo, and Phizer. Makoto Akaishi is a member of independent committee of Kowa Kirin CoLtd. Chisato Izumi has received speaker honoraria from Bristol-Myers Squibb, Otsuka Pharmaceutical, Edwards Lifesciences, Cannon Medical Systems, Daiichi-Sankyo Company, Sumitomo Dainippon Pharma, Toa Eiyo LTD, MSD, Pfizer, Nippon Boehringer Ingelheim, Teijin, Tsumura, and Novartis, and has received research grants from Daiichi-Sankyo Company, Cannon Medical Systems, Teijin, Pfizer, Idorsia Pharmaceuticals Japan, and AstraZeneca. Sakiko Miyazaki, and Satoshi Nakatani declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Onishi, T., Fukuda, Y., Miyazaki, S. et al. Practical guidance for echocardiography for cancer therapeutics-related cardiac dysfunction. J Echocardiogr 19, 1–20 (2021). https://doi.org/10.1007/s12574-020-00502-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12574-020-00502-9